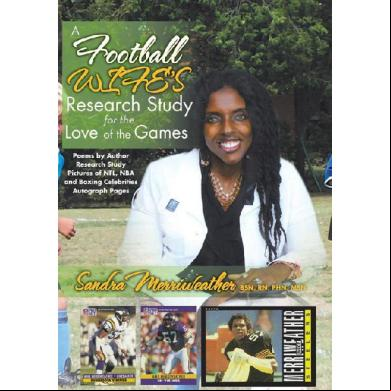
A Football Wife's Research Study For The Love Of The Games 4q3a1e
This document was ed by and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this report form. Report 3b7i
Overview 3e4r5l
& View A Football Wife's Research Study For The Love Of The Games as PDF for free.
More details w3441
- Words: 20,724
- Pages: 321
- Publisher: Xlibris US
- Released Date: 2013-02-11
- Author: Sandra Merriweather
A Football Wife’s Research Study for the Love of the Games
School Nurses’ Knowledge on Assessments of Concussions and Head Injuries in Athletes
Sandra Merriweather
Copyright © 2013 by Sandra Merriweather.
Library of Congress Control Number: 2013900410 ISBN: Hardcover Softcover Ebook
978-1-4797-7630-6 978-1-4797-7629-0 978-1-4797-7631-3
All rights reserved. No part of this book may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner.
The author is unable to give advice or judgment when it comes to specific diseases and medical problems. It is necessary that one should seek medical council and attention from the services of a competent medical provider. It is not the intent of this book to diagnose medical problems, but every effort has been made to provide accurate scholarly information. The author and publisher will not be responsible for errors or omissions. Please seek the advice of your medical doctor.
To order additional copies of this book, : Xlibris Corporation 1-888-795-4274 www.Xlibris.com [email protected] 123827
Contents
List of Tables
List of Figures
Acknowledgments
Abstract
Chapter 1: Introduction to the Problem
Introduction
Problem Statement
Research Questions
Rationale and Significance of the Study
Definition of
Summary
Chapter 2: Literature Review
Introduction
Key Words
Review of Literature
Identified Problems
The Consequences
Chronic Traumatic Encephalopathy
Second Impact Syndrome
Post-Concussion Syndrome
Mild Traumatic Brain Injury (MTBI)
Traumatic Brain Injury (TBI)
Concussion
Postconcussive Symptoms
Role of the School Nurse
Education
Current Best Practices
Interventions for School Health
Nursing Assessment, Intervention, and Evaluation
Danger Signs of a Concussion
The Glasgow Coma Scale
Summary
Chapter 3: Methodology
Introduction
Research Design
Setting
Description of Participants
Description of Instruments
Data Collection and Analysis
Assumption and Limitations
Human Subjects Protection
Summary
Chapter 4: Findings
Overview
Analysis of Data
The Nurse Educator
The Cardiologist
Triangulation of Data
Results and Interpretation
Summary
Chapter 5: Discussion and Conclusions
Overview
Discussion
Nurses Current Knowledge
Additional Knowledge Needed
Implications
Limitations
Recommendations
Conclusions
Appendix A
Appendix B
Appendix C
Appendix D
Reference
Recommendation Blurps
Book Summary
Sandra’s Bio
List of Tables
Table 1: Danger Signs of a Concussion
Table 2: Number of Participant
Table 3: Age of the Participants
Table 4: Nurses’ Responses to Question 1
Table 5: Nurses’ Responses to Question 2
Table 6: Nurses Responses to Question 3
Table 7: Nurses’ Responses to Question 4
Table 8: Nurses’ Responses to Question 5
Table 9: Nurses’ Response to Question 6
List of Figures
Figure 1: Nurses’ Response to Question 5
Figure 2: Nurses’ Response to Question 5
DEDICATION TO OUR CELEBRITY SPORTS PLAYERS
This book would not be complete, If I would not give thanks to those celebrities that we meet. Not enough has been said, About foundations and legacy you have laid. To the current and former NFL, NBA, Soccer, Baseball, Hockey and Boxing Stars, Just know that you’re appreciated right here, right now, and from afar. The charity work that each of you so graciously perform is truly recognized; Beyond the physical sport and beyond the external human eye, And appreciated by all of your significant others and your lovely wives! As many of them have kept you focused time after time. Our love for you goes beyond mere co-existence; This is why we have so much love for you and patience. You are honored by your mentors, coaches, peers and fans, For standing tall, steadfast and being real men, Driven by adversity because what you exemplify comes from way deep within; Your gifts are many as demonstrated through the variety of talents from your hands. Sometimes not enough has been mentioned, not enough has been said.
About how you often give up your family time, To help those in need while contributing to the wellness of mankind Being a football wife and a relative of NFL players, I know what happens during and after “The Game,” You continue to love all your fans just the same! Participating in celebrity sports and sport events, football camps and golf tournaments! And not to mention all those pictures of present and past And all of those lovely autographs! Giving donations and raising money for charities, Continually looking for those who are without, ill and sick, most definitely! Thanks to you all for being who you are; Because you all will forever be our famous celebrity stars! We thank you for believing in research and education, We thank you for loving our future generation! And From all the sports wives across the entire world, We thank you for making us your girls!
Written by: Mrs. Sandra Merriweather
To All Nurses
Children are innocent; continue to treat their injuries with ion
And in a timely fashion
Often they have no voice
Because they are too young to make an adult choice
As nurses we advocate
Participate and mandate
In emergencies no time to contemplate, waiver, or hesitate
While grabbing our nursing bag
We realize there’s no time to lag
It’s our duty to have a substantial medical knowledge base
As they look to us with a solemn face
We must document, document, document
Noting times and, if necessary, call the ambulance
Knowing that you’re blessed while under stress
Their lives so many times are found within our hands
Responding to the scene as fast as we can
Lying there on school grounds
Your nursing assessment, just make it count!
Hats off to you, and thanks for all that you do
Helping parents and school districts protect children while in school
Written by Sandra R. Merriweather, RN, BSN, PHN, MSN
Acknowledgments
I would like to thank my husband, Michael Merriweather, retired NFL linebacker for the Pittsburgh Steelers, Minnesota Vikings, Jets, and Packers. I am thankful for his willingness to be patient while I embark upon something new and challenging. I am grateful for his encouragement and for the words “You’ve got to be tough and make another tackle” when I felt like I couldn’t go on. I am thanking Mike for his encouragement and for the love he has shown. I am truly thankful for WGU and for granting me the opportunity in a career I so love and cherish and for providing me with the best mentors: Dee Adkins and Cindy Watson. I would also like to thank Dee Adkins for brightening my day, for the words of encouragement, and for the listening ear. I am grateful for WGU for providing me with wonderful instructors: Dr. Vince Shrader, Dr. Pat McCarver, and Dr. Debra Dukes. I would like to thank my Capstone mentor, Dr. Tori Canillas-Dufau, for her expertise, longevity, and guidance during this entire project and for helping me to remain focused and consistent yet strong. I would also like to thank Dr. Timoteo Rico and Dr. Manshadi for added and for being a great friend to me and my family. I would like to also thank my children for their patience and understanding and to my only little granddaughter, Kasiyah Irene, for her beautiful smile that always brightens my day. I am also grateful to my very dear friends Carla Harris, LVN, and Kitty Taylor, RN, CNS, PhD(c) for their encouragement, advice, and wisdom. The words “Hang in there!” reminding me of the powering words voiced to me by my deceased mother, Irene Williams, and thanks to my sister, Dr. Rita Williams-Washington, and father, Pastor E. G. Williams, for their encouragement, prayers, and . I would also like to thank my beloved church family for remaining by my side in spirit and faith. Dear Mother,
To my dear mother whom I love and adore so very, very, much; Thank you for forever holding and touching my hands, Giving me direction and faith to know that, “I can” While impacting lives, helping children and helping man. You see, mother, I did pay close attention to the 41 foster and disabled Children whom you raised and gave so much love; I hope I can at least do one quarter of what you have done. You’ve nursed, clothed, guided, sheltered, comforted and fed those without; You’re greatly loved by all of us no doubt! Nor did you treat anyone of them different from your natural children; We were all treated the same; You have left me with beautiful memories and a legacy that I am not ashamed! You had this drive to reach others; You were just an exceptional mother! So, I found this one and only baby picture of you and me; What a wonderful team. Yielding our souls together, I believe; We have our legacy! Thanks for being an example of a Pastor’s Wife; It has led me to be attentive to other’s needs and to be present for changes occurring in lives.
Thanks for your many years of service to Marin General and Kaiser Hospital in Vallejo; You were a contribution to service that everyone knows. Thanks for giving me the desire to be a ed nurse; I love you so much that it can’t be explained with words. Thanks for yielding me to love children whole heartedly with unselfishness; And while I give service, “Do your very best!”
Love your daughter,
Sandra
The belated Mrs. Irene Alberty Williams and baby Sandra
Pastor E.G. Williams with wife, Irene
Abstract
The topic of concussion and associated head injuries in professional and collegiate athletes has been one of the most highly discussed subjects in sports. The recent deaths of retired NFL players associated with repeated head trauma has left communities and fans in disbelief. This topic has caused tremendous concern among medical professionals, sports officials, and families of the injured, and the media has taken it to another level because of the associated neurological, cognitive, and psychological effects that have the potential to affect the sports player later in life. Now, what has been overlooked is the problem of concussions, repeated concussions, head injuries, and its associated conditions and how it can affect the adolescent athlete. When a child becomes injured at school, there are those who attend to his/her needs. Those persons are coaches, trainers, school officials, and of course, medical professionals. In a school setting, when a child is injured, the school nurse is immediately called, and the coaches and trainers may also be the first persons on the scene. This study assessed the nurse’s current knowledge of head injuries in the adolescent athlete, and it gained additional knowledge that nurses feel they need to adequately assess and manage head injuries in athletic children. This study has revealed a need to incorporate new research findings of concussions/head injuries of young athletes into the school system as well as within the emergency rooms (ER) and trauma centers and suggests the application of concussion/head-injury scales, checklists, and guidelines to be used as a reference guide. The use of the Glasgow Coma Scale in the school systems has also been revealed as beneficial in recording the athlete’s conscious state prior to transfer to the ER. This study has also revealed the need for appropriate documentation to avoid future fatalities as in second impact syndrome and has assisted the public health arena in gaining additional nursing assessment knowledge.
Chapter 1
Introduction to the Problem
Introduction
Sport-related concussions have become an emergent problem within the collegiate and professional sports arena—as in the NFL, hockey, soccer, boxing, NBA, and other leagues—but a concussion can affect anyone and any age group. Age is most definitely not a factor. Concussions are known as a mild form of traumatic brain injury (MTBI) that happens from trauma to the head, and of course, children are prone to these types of injuries. Children who play sports have been known to continue playing in games with a known head injury because of not wanting to let their teammates or their coaches down, their eagerness to return to play, lack of knowledge of the results of continuing to play with an injury, and for many other reasons. There is a diversity of conditions that are associated with head trauma and its related , but the results are positively linked with cognitive impairment and mental development effects. Medical professionals, school officials, teachers, coaches, psychologists, and sport trainers are standing at a crossroad of preventions, solutions, and treatments because children as well as adults need solutions to this growing problem and the potential long-term effects. The resolution to part of this emergent problem will involve the entire educational team to have an individualized education plan (IEP) in place upon the return of the injured student. School nurses, both ed nurses and licensed vocational nurses, are the front-runners and the go-to persons in urgent medical situations that occur on school grounds. ed nurses are equipped with knowledge to teach parents and school staff about concussion safety, appropriate interventions, and implementation procedures upon returning to school post injury. Nurses are well educated and active participants in all health care settings that can set the tone for future generations to follow. It is extremely important for nurses to stay
current in knowing the signs and symptoms, to be aware of the risks of repeated head injuries, needed interventions, and treatment modalities in regards to concussions as this is becoming an important problem in the public health area. Current records suggests that concussions for 8.9 percent of all high school sports injuries and that females may be prone to higher rates of concussive injuries compared to male athletes participating in the same sports (Piebes, Gourley, Valovich-McLeod 2009; Gessel, Fields, Collins, Dick, and Comstock 2007). Research is also signifying that there may be enduring effects from a sport-related concussion that may impinge on the adolescent child’s physical and mental health, causing academic problems (McCrory, Meeuwisse, Johnston, Dvorak, Aubry, Malloy, and Cantu 2008). Due to these current studies, statements, and facts, it is imperative that all education personnel, school nurses, physicians, counselors, coaches, and athletic trainers collaborate to provide the best environment for the injured athletes. This Capstone Research Project has examined the current knowledge of school nurses’ assessment of head injuries in athletes as well as examined knowledge that the school nurses feel they need to provide the proper management and treatment. This research project has also discussed concussions along with its related , the signs and symptoms of a concussion, and the need for adequate recovery time, and it has identified conditions that can alter cognitive function and mental development. This research study has also discussed the possible effects of repeated concussions in athletes.
Problem Statement
It is a known fact that a history of repeated concussions can have damaging effects leading toward neurological, cognitive, and mental impairments as with some of our famous celebrity sports figures that have experienced permanent disabilities and, in some cases, have even died. Concussions/head trauma and injuries not only affect professional ball players but it can also have an effect in athletic children. There is now a growing public health need to promote safety, teaching, and interventions that will protect the immature brain. It is important that school nurses play an active role by first keeping current in new developments, treatments, and return-to-play guidelines and be advocates for the
children. Having a substantial amount of current information while promoting teaching to the families and collaborating with physicians, school personnel, coaches, trainers, et al., will provide a foundation and a plan that will be beneficial for the child upon returning to school after being injured. It’s going to take the whole village of professionals to get a grip on this growing problem.
Research Questions
1. What are school nurses’ current knowledge related to the assessment of head injuries in athletes? 2. What additional knowledge do school nurses believe they need to adequately assess and manage head injuries in athletes?
Rationale and Significance of the Study
Concussions and head injuries among the youth are becoming a fast-growing concern among medical professionals. This growing public health concern is challenging our nurses to be proactive, caring, advocates, teachers, and collaborators among peers, families, physicians, and coworkers. The time has come to upgrade our assessment skills from the standards of past time because of current medical research advancements and findings. Nurses must assist the child with care and treatment after sustaining a concussion. The child will need follow-up treatment and ongoing assessment while attending school. Therefore, working closely with other school officials and staff will provide an optimal environment during the healing process and will further aid in the recovery stage. Also, depending on the type and level of injury, the child may soon return to play per physician, but exactly how will the nurse assess this? The need for this study is great, and the problem to be addressed is so very real. With the school officials’ willingness to learn and cooperate with the nurses and physicians, the injured child will have the that will aid in recovery.
Definition of
The following were used in this study: Chronic Traumatic Encephalopathy (CTE): This is a neurological disorder associated with repeated concussions. This condition is associated with the presence of tau proteins in the brain. The effects are long lasting and may appear years later after having played in sports (Omalu, Dekosky, Hamilton, Minster, Kamboh, Shakir, and Wecht 2005; Omalu, Dekosky, Hamilton, Minster, Kamboh, Shakir, and Wecht, 2006). CTE is the term applied to chronic cognitive, intellectual, and neuropsychiatric symptoms of chronic neurodegeneration following a single episode of severe traumatic brain injury or (more commonly) repeated episodes of mild traumatic brain injury (MTBI). CTE represents the cumulative, long-term neurodegenerative consequences of repetitive concussive and subconcussive impacts to the head (Omalu, Fitzsimmons, Hammers, and Bailes 2010). Concussion: A concussion is a type of mild traumatic brain injury (MTBI) that occurs due to an impact or jolt to the head. The American Academy of Neurology clearly defines concussion as a “trauma-induced alteration in mental status that may or may not involve a loss of consciousness” (Kirkwood, Yeates, and Wilson 2006; Neurology 1997). Mild Traumatic Brain Injury: The traditional definition of mild has been a Glasgow Coma Score (GCS) of 13 to 15. The many words that have been used interchangeably are subtle, minor, minimal, or concussion and continually add to the confusion because of the snowball effect it has when a child has been subjected to recurring head trauma (Cook, Schweer, Shebesta, Harties, and Falcone 2006). Second Impact Syndrome: This is another type of head injury that has been determined as a fatal, overpowering increase in intracranial pressure (I) that occurs from swelling of the brain due to a previous blow to the head that had not recovered (Miele, Norwig, Bailes, 2006; Kelly and Rosenberg l997). Traumatic Brain Injury: A traumatic brain injury is a serious injury to the brain
from an outside force that can lead to lasting or momentary destruction of cognitive, mental, physical, and psychosocial disorders. There may also be an associated or diminished altered state of consciousness.
Summary
The school nurse plays an important role when children are injured on the school site and should be called immediately to attend to the emergent needs, as well as the athletic trainer and coaches, which are also first responders. While research knowledge continues to grow in the area of concussions in athletic children, so must the knowledge base in our nursing and medical curriculum while extending into the profession. As one can see, the injured child will require collaboration among medical professionals, school officials, s, teachers, and counselors due to problems associated with cumulative effects. We all must learn to listen, observe, and watch for signs and symptoms of impending threats to the health and well-being of our children. Why listen? We listen because a child’s pain grows silent when the eagerness to continue to play in the games outweighs sitting on the bench. We listen and observe because a child’s words need to be heard, but when they are silent, we must be advocates. Nurses are advocates who are well-trained licensed professionals that are equipped with an abundance of information, but as research expands, so must nurses’ knowledge. This research has examined school nurses’ current knowledge related to the assessment of head injuries in athletes. Staying current on the latest research in this area not only expands the nurses’ medical knowledge but also enables them to assess, implement, evaluate, and teach with the most up-to-date information. Chapter 2 has reviewed scholarly published literature that is of valuable importance in addressing the issue of concussions and head injuries, return-toplay guidelines, and signs and symptoms in the injured athlete.
Chapter 2
Literature Review
Introduction
The medical field and even the news media have really grasped the facts of the growing problems and the long-term effects that concussions have demonstrated in professional athletes. There have been a number of unfortunate, highly profiled deaths of NFL players that have gained the attention of the media, and now, finally, concussed children are drawing much-needed attention. Presently, attention to concussions in athletic children is beginning to take first-class seats. This literature review will explore evidence-based research previously conducted on the subject of concussions and head injuries in those persons that have played sports. The literature will review pertinent information that reveals signs and symptoms of not only concussions but also its associated conditions.
Key Words
Head injuries, head trauma, concussions, sport-related concussion and mild traumatic brain injuries (MTBI), multiple concussions, cerebral concussions, recurrent concussions, cognitive impairment, depression, sudden impact syndrome (SIS), mental impairment and mental disability, cumulative brain injury, postconcussive syndrome (PCS), chronic traumatic encephalopathy (CTE), school athletes, school nurses and management.
Review of Literature
Included in this research study, the literature also contains three articles. Two were written in1997. The article by Kelly and Rosenberg, both credible physicians, discussed the diagnosis and management of a sports’ concussion, which is also a key factor in this study. This article was chosen due to the limited literature of concussion studies in children. The second article included (Mittenberg, Wittner, and Miller 1997) recognized that post-concussion syndrome occurs in children, and it also discusses the need of nurses and others to be active in identifying the signs and symptoms in concussion. The article by the Virginia Brain Injury Lawyers discussed the death of an NFL player that suffered repeated head trauma. These three articles contain pertinent information.
Identified Problems
Concussions, head injuries, mild traumatic brain injury (MTBI), and sportrelated concussions appear to be one of the most popular and yet intriguing topics as they relate to professional athletes of the present and of the past. The interesting thing is that these are used interchangeably and contribute to the confusion of the topic at hand. There are also other conditions associated with head injuries such as post-concussion syndrome (PCS), second impact syndrome (SIS), and chronic traumatic encephalopathy (CTE), but what is common to each concussion term is the associated cognitive impairment and mental development effects.
The Consequences
These conditions can have long-lasting effects resulting in serious conditions
that affect the emotional well-being of the athlete. What seems to be an issue that has been downplayed, overlooked, and somewhat ignored is that a sport-related injury can happen to any person, as in our athletic youth not just in college or among professional athletes. One must keep in mind that a child’s brain is underdeveloped and that the head injuries sustained can increase the risks of further complications. These complications can result in progressive deterioration in social and cognitive function: loss of memory and memory disturbances, loss of executive functioning, paranoid ideations, exaggerated responses to life stressors, rampant fluctuations in mood, problems with intimate and family relationships, sleep disturbances, major depression, alcohol and/or drug abuse, violent behavior, increase interest in religion, body aches, pains and headaches, direct autopsy brain tissue with evidence of cerebral taupathy (Omalu, Hamilton, Kamboh, Dekosky, and Bailes 2010). There have been several studies on college and professional athletes regarding the effects of concussions but few revealing the effects of such on high school athletes even though many youth have died due to second impact syndrome (SIS). More research needs to be done in regards to the effects of concussions on age, immaturity, and developmental differences. Research studies have concluded that their data suggest that a history of repeated concussions may be a risk factor for late-life memory impairment, mild cognitive impairment (MCI), and Alzheimer’s disease (AD) (Guskiewicz, Marshall, Bailes, McCrea, Cantu, Randolph, and Jordan 2005; CDC 2011).
Chronic Traumatic Encephalopathy
Chronic traumatic encephalopathy (CTE) refers to persistent cognitive and neuropsychiatric symptoms of continual neurodegeneration following a single episode of severe TBI or recurring episodes of MTBI. CTE can only be definitely diagnosed by direct tissue examination (Omalu, Bailes, Hammer, and Fitzsimmons 2010). CTE has been previously termed as dementia pugilistica due to its association with boxing as initially described by Corsellis in l973 (Gavett, Stern, and McKee 2011). Dr. Bennet Omalu initially discovered physical evidence of concussions and
CTE in sports other than boxing. Dr. Bennet Omalu along with other founding (Julian E. Bailes, MD, and Atty. Robert P. Fitzsimmons) developed a new center called the Brain Injury Research Institute (BIRI) for the study and prevention of traumatic brain injuries. The institute has constituted a brain and tissue bank that contains 20 brains for future studies. It is the desire of the founders to develop appropriate treatment and intervention protocol for this disease as well as to ascertain genetic predisposition that will decrease progression and, hopefully one day, to provide a cure (Brain Injury Research Institute 2009). The long-term effects of concussions and head injuries are many, and something beneficial in the reduction of concussions must be done to protect children now and throughout their adulthood as several adolescent and college youth have been found to exhibit early signs of CTE. Chronic traumatic encephalopathy (CTE) must be taken seriously as this is not just a threat but also a word of warning to advancing destruction to the human brain and the centers that control certain operations. CTE can alter and threaten a sports player’s life no matter what age the person may be. CTE, in connection with pathologic changes, can alter memory and managerial functioning; behavioral and personality disturbances (apathy, depression, irritability, impulsiveness, and suicidality); Parkinsonism and irregularly; and motor neuron disease as seen in affected persons (Gavett et al. 2011). The diagnosis of CTE has not changed; it is diagnosed after death by examination of brain tissue. Yes, the problems attached to CTE can be fatal and/or long lasting, but the question is, how many lives will it take to truly grab the attention of children and head injuries while realizing that the adult professionals were also once children and played as children? Presently, there are no current neuropathological criteria that have been agreed upon for the diagnosing of CTE or large-scale, longitudinal clinicopathological correlation studies, and this makes the diagnosing of CTE difficult (Gavett et al. 2011). On February 17, 2011, a well-known NFL safety for the Chicago Bears committed suicide. He had a remarkable defense career playing football in 1985. Today this man is no longer with us because his symptoms resulted in his suicidal death. His behavior prior to his death exhibited a downward spiral in reasoning ability, erratic and violent behavior with signs and symptoms of
depression. He was discovered to have significant changes in personality and character (Virginia Brain Injury Lawyers 2011). This man, known as Dave Duerson, was only 50 years old, and after studies by Boston University physicians and the director of Neuropathology Care at Boston University’s Alzeimer’s Disease Center, it was confirmed that this man showed classic and moderately advanced symptoms of CTE (Needle and Ellenberg 2011).
Second Impact Syndrome
Another problem that is so unique to this topic—like that of NFL, NBA, hockey, soccer, boxing professionals, etc.—is that major injuries and death have occurred among this group, and it has occurred in athletic youth as well. It is especially important to treat head injuries, thus allowing time for adequate healing because a second blow or injury to the head without sufficient time to heal from the initial injury will lead to second impact syndrome (SIS), complications, and even death—a potential lethal combination. Second impact syndrome is another type of head injury that has been determined as a fatal, overpowering increase in intracranial pressure (I) that occurs from swelling of the brain due to a previous blow to the head that had not recovered (Miele, Norwig, and Bailes 2006; Kelly and Rosenberg l997). A second brain injury can lead to an increase in cellular death (Zink and McQuillan 2011). If a player continues to reenter games of sports with untreated head injuries, then the results can be CTE and its complications; this is why documentation of head injuries and adequate records are very crucial. There is much controversy surrounding the second impact syndrome due to lack of documentation of the first head injury, continued symptoms, and medical problems and the severity of the second impact (Miele et al. 2006; McCrory 2001). Again, early intervention from medical professionals with adequate documentation is necessary and crucial at the sidelines. The possibility of getting a concussion is now even more frightening. This new information has alerted the medical world to researching preventative treatments and, hopefully one day, a cure. Researching this area matters as it affects not only current and former NFL players but also all persons
in sports, from our youth to adults, friends and families, and persons we all love. Examining this area will alert all persons involved in sports, such as persons in the medical field, athletic trainers and coaches, referees, school officials, and others to take precautions in preventing head trauma/concussions. This information will also alert them to the signs and symptoms of the subject at hand, thus enhancing teaching, documentation, and observation skills.
Post-Concussion Syndrome
There are many postconcussive symptoms (PCS) that have been divided into three groups: somatic, emotional/behavioral, and cognitive. The symptoms of each of these three groups make the injured minor subjective to close observation at home and at school because of somatic disturbances (headaches, fatigue, nausea, vomiting, visual changes, tinnitus, dizziness, balance problems, and sensitivity to light and noise). There are also emotional and behavioral problems that can occur as a result of postconcussive symptoms (lowered frustration tolerance, irritability, increased emotionality, depression, anxiety, dizziness, and personality changes). The cognitive problems that can exist affects a child’s intellect (a slowed thinking or response speed, mental fogginess, poor concentration, distractibility, trouble with learning and memory, disorganization, and problem-solving difficulties) (Kirkwood 2006).
Mild Traumatic Brain Injury (MTBI)
Mild traumatic brain injury (MTBI) is a growing and an important public health problem. The traditional definition of mild has been a Glasgow Coma Score (GCS) of 13 to 15. The many words that have been used interchangeably are subtle, minor, minimal, or concussion and continually add to the confusion because of the snowball effect it has when a child has been subjected to recurring head trauma (Cook, Schweer, Shebesta, Harties, and Falcone 2006). MTBI can escalate into a more serious health care condition. The consequence
results in physical, cognitive and behavioral impairments, and serious disabilities, depending on the severity of the damage (Cook 2006; Piebes, Gourley, Velovich-MCleod 2009). There are many articles on children playing in the games of sports as well as the problems associated with concussions, and there are several youth who have died while playing in the games, but there is a great amount of room for further research in this area. An important point is to note that the literature concerning the epidemiology, treatment, diagnosis, prognosis, and costs of mild traumatic brain injury (MTBI) has been searched, and it has been clear on the fact that children’s prognosis after an MTBI is good with quick interventions and resolutions of symptoms (Carroll et al. 2004).
Traumatic Brain Injury (TBI)
An important public health concern is traumatic brain injury (TBI) because every year, it affects more than 1.7 million Americans (Guskiewicz 2005; CDC 2011). Fatalities of head injuries occur in 52,000 persons in the United States each year, but the majority of head injuries are determined to be TBI. A TBI is a nondegenerative and noncongenital hit to the head or an object that has caused piercing of the skull to the brain, possibly leading to permanent or temporary injury of cognitive, physical, and mental functions with an associated decreased or altered state of consciousness (Dawodu and Campagnolo 2011). It can result when the head suddenly hits an object or when an object penetrates the skull, entering the brain tissue. The amount of damage to the brain determines the severity of the condition. An estimated $60 billion is spent annually on brain injury treatment and rehabilitation (Bay 2011; Iavagnilia C, 2011). Severe sportrelated injuries of the head are many as there are several diagnoses, but a mild traumatic brain injury (MTBI) is a more common injury that causes difficulty in management. It becomes especially hard to manage when the decision of returning a player to the game is needed. With an epidural hematoma injury, a player can be initially stunned and appear to be doing well right after, but within the next 15-30 minutes, they may experience progressive neurological impairment. Observation and early recognition are essential during this period (Miele, Norwig, and Bailes 2006).
Traumatic brain injury has received limited national attention from various public agencies until recently. This condition has captured the attention of public policy makers, elected officials, and even among military officials. The is now readily available as research continues to formulate discoveries. What is needed and desired are policies, procedures, and of course, medical and nursing protocols for providing necessary treatments (Trudel, Scherer, and Elias 2011). Research findings have implicated consistent evidence that most children and adolescent children recuperate fully from a single straightforward MTBI. Prognosis has been determined well after MTBI (Kirkwood, Yeates, and Wilson 2006; Carroll, Cassidy, Peloso, Borg, Holst, Holm, Paniak, and Pepin 2004). It is, however, important that the healing process be allowed ample time to recover no matter how long it takes to reduce neurobehavioral problems, the same problems reported in adults (Kirkwood et al. 2006; Mittenberg, Wittner, and Miller l997).
Concussion
A concussion is a type of mild traumatic brain injury (MTBI) that occurs due to an impact or jolt to the head. The American Academy of Neurology clearly defines concussion as a “trauma-induced alteration in mental status that may or may not involve a loss of consciousness” (Kirkwood et al. 2006; Neurology 1997). Concussion is a functional, rather than a structural, injury that results from shear stress to brain tissue caused by rotational or angular forces. Many people believe that it is mandatory that the impact involves an injury directly to the head, but it does not. An impact can occur from other areas of the body. Initial assessment involves eliminating cervical spine injury and serious traumatic brain injury. The most common symptom of a concussion involves headaches, but symptoms can occur from other clinical domains (e.g., somatic, cognitive, affective). There is a range of assessment tools to assist with diagnosis, including symptoms checklists, neuropsychological and postural stability tests, and sideline assessment. Both cognitive and physical rest contributes to the initial management of this condition. There are no specific treatments for concussions.
The goal is to control symptoms and return the individual to play (Scorza, Raleigh, and O’Connor 2012). Children may need a longer recovery process due to the immature developed brain. Further study is needed in this area to determine the effects of impact on the immature brain. A concussion also disrupts cellular activity in the brain from functioning properly. Even though most individuals will recover wholly after a concussion, the signs and symptoms of this injury may last from several minutes to several months or even longer. Long-term effects from a concussion can alter thinking, memory, learning, language, and emotions (Samiento, Mitchko, Klein, and Wong 2010). There are many immediate signs and symptoms of a sport-related concussion, which are similar in younger and older athletes, as follows:
• A change in playing ability • A vacant stare • Fogginess • Confusion • Slowing • Memory disturbance • Loss of consciousness • Increased emotionality • Incoordination • Headache • Dizziness • Vomiting
It is highly recommended that a child who has suffered a single MTBI be allowed enough time to recover from the initial injury; if not, these children may encounter serious complications similar to the adult professional ball players as in a study performed on a professional football player that began organized football at age 18 and resulting in 14-year span of play (Omalu et al. 2006). Sportsmen that are subjected to recurring MTBI are also subjected to enduring neurodegenerative outcomes (Omalu et al. 2005).
Postconcussive Symptoms
The conditions that a child may now face will exhibit postconcussive symptoms (PCS) that are categorized into three different areas termed somatic, emotional/behavioral, and cognitive effects (Kirkwood et al. 2006). Even though children may respond to head injuries similar to that of the adult, there are some major differences. Some of the signs and symptoms of a serious concussion include the following:
• A headache that gets worse and will not go away • Muscular numbness and weakness including decreased coordination • Ongoing nausea and vomiting • Slurred speech patterns
New advancements have been made in protecting our youth participating in athletic activity for children between the ages of 11 and 18. As of January 2012, all coaches of any organized youth athletic activity will be required to take an online course for recognition of concussions (Castellanos and Oakes 2011).
Several key words were used to represent this research design and will be used to guide the information obtained. These key words are head injuries, head trauma, concussions, sport-related concussion, mild traumatic brain injuries (MTBI), multiple concussions, cerebral concussions, recurrent concussions, cognitive impairment, depression, sudden impact syndrome (SIS), mental impairment and mental disability, cumulative brain injury, postconcussive syndrome (PCS), chronic traumatic enceph4alopathy (CTE), school athletes, and school nurses.
Role of the School Nurse
The school nurse plays an important role when children are injured on the school site and should be called immediately to attend to the emergent needs along with the athletic trainer and coaches, which are also first responders. While research knowledge continues to grow in the area of concussions in athletic children, so must the knowledge base in our nursing and medical curriculum and within the profession. As one can see, the injured child will require collaboration among medical professionals, school officials, s, teachers, and counselors due to problems associated with cumulative effects. We all must learn to listen, observe, and watch for signs and symptoms of impending threats to the health and well-being of our children. Why listen? We listen because a child’s pain grows silent especially when they are eager and desire to continue to play in the games, and besides, in their eyesight, this outweighs sitting on the bench. We listen and observe closely because a child’s words need to be heard, and when they are quiet, we must be their voice while acting as advocates.
Education
The primary focus within this research design is to gain knowledge of what school nurses know about assessing head injuries in adolescent athletes. It is important for school nurses to gain current knowledge on how to assess and treat acute head injuries/concussions as it is common practice to notify nursing staff
of any impending emergencies or acute situation at the school site. The nurse is usually responsible for coordinating and managing quality care. Documentation is a must for future reference as well as a guide in managing second-impact injuries. Evaluation and recovery is essential for return-to-play guidelines. It is equally important for the nurse to collaborate with the family, physicians, school officials, trainers, coaches, and personnel as well so that the best education can be provided while the child is absent from school, returns to school half-day, and returns to school full time. The time of the healing process is varied and depends upon the type of injury and whether it is a second-impact injury. Most children who have sustained a sport concussion can recover fully with proper treatment. There are many reasons as one can see why the need is so great to provide the most current information for school nurses, officials, as well as the parents so that children can receive the most beneficial treatment toward the recovery process. Researching this area is necessary because the research in this area continues to make new discoveries, and as new information becomes available, it is also a necessity to alert and increase the knowledge of the school nurses as they are immediate responders. The results in this area will provide the researcher of which assessment areas need clarification, training, and/or more knowledge.
Current Best Practices
Head injuries and concussions occur on the school grounds more often than the media, medical personnel, school officials, and parents once believed due to the lack of knowledge by adults and the reluctance to report by children for fear of not being able to continue to play in the games. Now that there has been an increase in awareness of concussions, there are certain points that need clarity and addressing. School nurses play a very large role in the security of children while they are attending school, and it is necessary for the nurse to have a knowledge base that is current and accurate. Knowledge, assessment, and implementation of initial treatment are three components that the nurse must possess when responding to an injured child. Providing quality and effective care will promote the best
optimal level of well-being. Head injuries and concussions can no longer be considered as “just another bump on the head” as its long-term effects without treatment can be devastating, resulting in both cognitive and mental disabilities. Nursing management, collaboration with physicians along with other medical personnel professionals, school officials, coaches, trainers, and parents and psychologist will also equip the child with a good foundation to cope and begin the healing process. Nursing management should make sure that a head-injury protocol is in place at every school so that nurses will be knowledgeable of their duties and will be aware of designated responders during emergent situations (Pennington 2010). The CDC has taken a positive step in deg a tool kit for coaches of secondary school. It has information about concussions in youth. The CDC has also conducted a study to determine which items were helpful to the coaches in increasing their knowledge, practices, and prevention to safely manage sport concussions. The tool kit consists of facts about concussions and what to observe (Samiento, Mitchko, Klein, and Wong 2010).
Interventions for School Health
School professionals are extremely important and play a vital role in assisting a child’s return to school post concussion due to the need to limit activities during the recovery process. There are activities that can cause concussion symptoms to reemerge and degenerate; they include studying, working on the computer, and playing video games. These activities can lead to what is called cognitiveexertional effects (Samiento et al. 2010). Thinking and learning, which are both cognitive activities, must be monitored carefully to avoid this effect. It is extremely important for clinicians to be knowledgeable about the usual course of recovery and to recognize when recovery is not taking place as expected. Clinicians must be able to screen and seek out those persons appearing to have complications and those persons that are at the greatest risks for an optimal outcome (Carrol, Cassidy, Peloso, Borg, Hoist, Holm, Paniak, and Pepin 2004).
According to Samiento (2010), “Implications for School Health,” those children
returning to school must do the following:
• Take frequent rest breaks • Spend fewer hours at school • Be given extra time to take and complete assignments • Receive help with school work • Reduce time spent on the computer, reading, or writing
Students should not return to participate in recreational activities on the same day of injury unless cleared and evaluated by a health care professional that is experienced in the evaluation of concussions. A student must also show clearance of the injury from a medical professional stating that they are symptom-free, and they must not return to these following classes until medically cleared:
• Physical education (PE) class • Physical activity at recess • Sports practices or games
It is highly important and recommended that all school officials, medical personnel, coaches, parents, and students work in collaboration to benefit the child’s health and be aware for any of the following problems:
• Increased problems paying attention or concentrating
• Increased problems ing or learning new information • Longer time needed to complete tasks or assignments • Inappropriate or impulsive behavior during class • Greater irritability • Less able to cope with stress or is more emotional • Difficulty organizing tasks • Symptoms that get worse (headache, tiredness) when doing schoolwork
It becomes difficult for a child when he/she becomes injured because of the changes that occur with the physical, cognitive, and mental health. Their activities also become altered, and many times, they cannot comprehend the importance of resting, relaxing, and taking things slow. This is why it will take the entire teaming of professionals that are involved in the child’s care to give them the attention they so deserve. The team of school educators and school nurses will need to offer and encouragement to the saddened heart, to the child that feels discouraged, and to the child who has lost his/her concentration. Let’s not forget the child that feels frustrated with the sense of “I can’t go on.” Through collaboration and cooperation from the child’s team, the child will regain encouragement and a sense of self-worth with academic achievement.
Nursing Assessment, Intervention, and Evaluation
A concussion exists when the brain is jarred while in acceleration-deceleration, momentarily disturbing the functioning of the brain. There is no association between concussions having a visual structural abnormality on a CT scan. The management of concussions is geared by treating the symptoms. Experiencing headaches is one of the most frequent complaints.
Research by Zink and McQuillan (2011) and the CDC (2011) suggest that persons experiencing a concussion may exibit the following symptoms:
1. A period of unconsciousness 2. Unconsciousness lasting seconds to hours 3. Temporary loss of reflexes 4. Amnesia prior to and after the event 5. Headache or pressure in the head 6. Fatigue, feeling sluggish, hazy, foggy, or groggy 7. Dizziness or balance problems 8. Behavioral disorders 9. Double or blurry vision 10. Irritability 11. Memory problems 12. Difficulty concentrating and paying attention 13. Trouble sleeping and anxiety 14. Nausea or vomiting 15. Bothered by light or noise 16. Confusion
The above signs and symptoms may last for months post injury and is known as post-concussion syndrome (PCS). These symptoms do lessen, given time to
recuperate. Persons with concussions are usually seen in the emergency rooms but are usually discharged. It is up to clinicians to be educated and to document accordingly and especially when an injured child returns to school. Also, the need for accurate documentation of an initial injury will assist in providing pertinent information if a second impact occurs. Offering the assistance of groups and rehabilitation services will benefit the client. Advise the family of an injured child to refrain from activities that may lead to a repeat injury and to notify their physician of ongoing, persistent problems (Zink and McQuillan 2011). Keep in mind that treatment of concussions and head injuries vary depending on the injuries sustained. It will be necessary to follow the physician’s orders, making sure that the child seeks follow-up care, provide injury prevention information and other pertinent resources, and always be sure to obtain medical clearance from a physician prior to the child returning to play. Maintain good communication between school officials, coaches, trainers, parents, physicians, and medical professionals to return the child to an optimal level of function.
Danger Signs of a Concussion
The Centers for Disease Control and Prevention (CDC 2010) explains that, in rare cases, a blood clot may develop on the brain of a person with a concussion that crowds the brain against the skull. This is an emergent medical problem, and it is important to note danger signs and impending threats to a sports player’s well-being. A sports concussion is an injury that is blind to the eye but can be detrimental to the brain and to the quality of life. Concussions, therefore, should be managed carefully, and every injury, no matter how small or large, requires medical attention. Listed below is a danger sign chart developed by the Centers for Disease Control and Prevention (CDC 2010):
Table 1 Danger Signs of a Concussion
One pupil larger than the other Drowsy and unable to awaken A headache that does not go away but worsens Weakness, numbness, or decreased coordination Repeated vomiting or nausea Slurred speech Convulsions or seizures Cannot recognize people or places Becomes increasingly confused, restless, or agitated Has unusual behavior Loses consciousness (a brief loss of consciousness should be taken seriously)
The Glasgow Coma Scale
The Glasgow Coma Scale (GCS) has been used as a method to record level of consciousness in comatose patients and predominately used in hospitals. The GCS is not readily used with the very young child due to his/her inability to communicate well. There is a pediatric version similar to the adult version. The GCS can be used in the older child to assess eye-opening verbal and motor responses according to precise grading scales. Pediatric brain injuries are classified by severity using the same grading scales as adults and can determine long-term impairments. The GCS can be used as a prehospital predictor of outcome (Gabbe, Camaron, and Finch 2003).
Summary
This area of focus has extremely limited current research conducted in the area of prolonged effects of concussions on youth athletes although the problem has been identified, and this has caused the researcher to include areas of research conducted on adult athletes. There is more room for further research studies and the possibilities of teaching new knowledge of sport-related concussions in children because they suffer injuries like everyone else. This topic even appears to have more interest in male athletes, but a research study has determined that there are even sex differences in concussion symptoms of high school athletes. After a sport-related concussion, male and female high school athletes presented different types of symptoms. Males stated they had more cognitive problems whereas the girls complained of more neurobehavioral and somatic symptoms (Frommer, Gurka, Cross, Ingersoll, Comstock, and Saliba, 2011). As one can see, gender is now an issue of interest. There are many questions that arise concerning sport-related concussion/head injuries in athletic adolescent children as this topic needs continual interest. The literature review s the findings that concussions occur in athletic children as well as with professional athletes and that there are signs and
symptoms as well as potential prolonged effects (presently being investigated) that medical staff should be aware of, as the injured child may not discuss when they are injured because of the desire to continue to play in sport games as well as not wanting to let their teammates and coaches down. One important fact that everyone should keep in mind is that the professional and collegiate sports players that are now presenting with cognitive, psychological, and mental disabilities began playing sports as children. It is clear that school nurses need to be aware of all signs and symptoms of concussions and head injuries because medical research is discovering new findings.
Chapter 3
Methodology
Introduction
Chapter 3 describes the methodology and the research design for this study. The goal has been to address and answer the two following research questions:
1. What are school nurses’ current knowledge related to the assessment of head injuries in athletic children? 2. What additional knowledge do school nurses believe they need to adequately assess and manage head injuries in athletes?
Research Design
This research design used a qualitative approach that applied triangulation by way of questionnaires (one that was designed for the school nurses and one especially designed for the nurse educator/advanced practice nurse) and a structured interview with a cardiologist in California that addressed second impact and its relationship to head injury. The interview provided more in-depth information of data on second impact syndrome and revealed the importance of documenting every head injury as documentation provides medical clinicians and professionals with accurate information needed for future management of care. The researcher used a recording device to tape the interview, and the data
were immediately transcribed and stored in a secured safe along with the questionnaires in a locked room. In order to assess nurses’ knowledge, the data from the school nurses’ nonrandom questionnaire were categorized with summation of findings into narrative form. The key idea in this study was to identify common group items and key information with common factors into clusters of the same issues while applying a sincere understanding of what has occurred with the data received (Gay, Mills, and Airasian 2009).
Setting
This research has taken place within the state of California, located centrally and east of the San Francisco Bay Area. There are a total of three participating school district nurses that included licensed vocational nurses (LVNs) and ed nurses (RNs). The number of participating school nurses totaled 40 participants. Included in this study are a nurse educator and a physician that have provided information and expert advice of this research subject.
Description of Participants
The LVNs and RNs from ages 24-67 were of interest. Their experience within the nursing field is varied, ranging from 1 year to 44 years practicing. The total number of RNs participating within the 3 school districts total 34 RNs, and the total number of participating LVNs is 6. These nurses are school nurses possessing a variety of nationalities, varied educational backgrounds with the majority being RNs, and they are employees of one of three participating school districts. The role of the school nurse within these school districts is to provide school health services, promote health education, and coordinate health care. The researcher chose to include LVNs in the study as well as RNs because often they also respond to the urgent needs of the children and provide treatment. One interesting fact that most definitely is a requirement for the success of satisfying
the goals within this particular study is the collaboration of everyone involved with the care of children. The nurses have a personal interest to provide the best care possible and to collaborate with other school officials, counselors, and instructors on the medical needs of the students. The present problems that are arising in the topics of concussion/head injuries are presenting new as well as much needed information, and this is getting the attention of everyone; therefore, medical professionals need to be updated with the most current facts, treatment, and interventions. Current knowledge on the topic of head injuries and concussions among the student athlete in many school districts has not yet been addressed although the nurses have had previous schooling and knowledge of the assessment and treatment of head injuries in general. The nurses as well as school officials find this topic extremely interesting being that the media has shed new light on the current additional problems associated with head injuries as a result of discoveries by physicians and other medical professionals; even physicians find this topic challenging and fascinating. The number of participating nurses suggests their eagerness and willingness to participate and learn new treatment interventions and modalities. The school nurses within this research design work closely together among their peers and among school officials. This demographic region provides a healthy environment for the sake of children as the location is within the central valley versus being in a fastpaced city promoting a tranquil environment. Questionnaires and a personal interview have been conducted confidentially, and approval has been given per three separate school districts. The ethnic composition of the nurses is varied, and the surveys were open to any nurse who wished to participate within the specific age group stated. with a physician and a nurse educator was made as needed for clarifications on medical findings, to provide input and suggestions in the area of assessing head injuries in athletic children.
Description of Instruments
The researcher was the primary source as well as the primary instrument that collected pertinent data. The role of the researcher was to analyze, interpret, and categorize information from the questionnaires while utilizing common schemes
and patterns. The gathering of data from the interview, questionnaires, including all entries and notes, were interpreted to determine the meaning of the records and facts to the best ability of the researcher. Discovering the meaning of the outcome of data after examination and comparing previous data to the most recent data were also tasks of the researcher. The researcher continued to build upon new discoveries while trying to make logic of the data as a whole thus incorporating coding and categorizing skills. The data were tapered down and placed into less significant groups. The key idea in this study was to identify information with common factors while applying a sincere understanding of what had occurred with the data received. One of the instruments used to store and collect qualitative data was a Microsoft ® Tableau Spreadsheet. The function of the Microsoft ® Tableau Spreadsheet is to simplify information by formatting data into computerized tables by way of rows and columns. This method is able to demonstrate relationships in a simplified way. To further strengthen this study, the researcher utilized the ATLAS.ti ® software, which analyzes qualitative data using multiwindow frames while providing an overview of the findings. This feature is known to provide while working. This is a software program that was ed to clarify and substantiate the findings of this research project.
Data Collection and Analysis
The data-collection methods chosen for my project were a qualitative research design utilizing triangulation techniques to gather information regarding “School nurses’ current knowledge related to the assessment of head injuries in athletes” and “What additional knowledge do school nurses need to adequately assess and manage head injuries in athletes?” Data collection began in April 2012. Participants were instructed not to include identifiable data on the questionnaires. The researcher de-identified all personal data that were received on the questionnaires. Data received were identified by groups, and the information was transferred to the Microsoft ® Tableau Spreadsheets that showed relationships as it also simplified the data. The spreadsheet contains
different themes that arose from 40 responded RNs and LVNs. The three datacollection methods consisted of a questionnaire distribution among each participating school nurse, a questionnaire that was given to a nurse educator, and an interview/questionnaire with a cardiologist for discoveries of a hit or blow to the chest causing a second impact. The interview with the cardiologist was audiotape-recorded by the researcher and subsequently transcribed. The transcription was given to the cardiologist for review for further detail as needed. This procedure provided both clarity and accuracy. The cardiologist addressed three questions in regard to second impact syndrome and its relationship to cerebral injury, additional knowledge he felt would be beneficial to nurses in managing head trauma, as well as additional knowledge that he believes nurses needed to adequately document a second impact. These in-depth responses will increase pertinent knowledge and current practice guidelines for nurses and medical professionals in detecting and treating sports concussions and head injuries in children. The questionnaire for the nurse educator addressed current practice guidelines and additional knowledge that would benefit nurses in managing head injuries in young athletes within the emergency room and trauma units. The purpose of choosing this data-collection method was to provide comprehensive content as well as reveal a definite connection between the severely injured athlete and interventions of school nursing that continues into the ER and trauma centers. It will provide readers with content voiced directly from those treating children with concussions and head injuries and gain knowledge and insight of this newly and highly discussed growing problem in the area of public health nursing. A prearranged time was set to meet with the nurse educator to address the specific set of questions. The data obtained from the qualitative method by way of triangulation were then coded for recurring themes. The information was then explored for understanding and meaning within the data. Coding identified ideas, and this allowed grouping of the information into various categories. All data has been explored to promote clarity, ideas, and interpretation that have been received from the data within. Questionnaires and personal interviews have been conducted confidentially with consent from the school nurses, both licensed LVNs, RNs, and the nurse educator. The questionnaires for the nurses (RNs and LVNs) consisted of six open-ended questions that addressed issues within this research design that has
addressed what the nurses know about assessing head injuries in athletic children. Included within the questionnaire are four demographic questions that addressed the nurses’ type of licensure (RN or LVN), age, and number of years practicing as a licensed nurse. was also received about the use of the Glascow Coma Scale (GCS), which is a method to record the level of consciousness that is predominately used in the hospital system; the researcher has obtained consent per each school district’s research process prior to the implementation of this research project. After obtaining consent from each school district, the researcher met with nursing management to set up specific times to meet with the nurses and distribute the individual questionnaires. The participants were informed that their participation in this study was strictly voluntary and that all information collected is confidential. They were also told that their submissions are confidential, and they were advised not to write their names on the forms. The participants were well-informed that they will not be reprimanded, dismissed, discriminated against, or retaliated against for participating in this study. The participants were told that this research does not involve any risks, harm, or costs. The participants were aware that participation in this research project was at their free will thus providing informed consent. The participants were also given information for additional questions. The school districts strongly suggested that the time set for distributing questionnaires must not interfere and conflict with the times in which a nurse must be readily available for the management of providing health care to the children. It was most appropriate for this study to be conducted just prior to nurses’ meetings. This researcher distributed the questionnaires prior to nurses’ meetings at the specified times agreed upon with nursing management in each school district. The information received from both the nurse educator and the cardiologist was compared to the data received from the 40 respondent school nurses. The purpose of choosing this data-collection method was to provide comprehensive content. It provides readers with content voiced directly from those treating children with concussions and head injuries while gaining knowledge and insight of this newly and highly discussed growing problem in the area of public health nursing. The data collected were reviewed and have been put in a narrative form, yielding narrative data, common characteristics, common patterns, and themes.
Differences in responses have been noted, and the discoveries and findings have been summarized. The questionnaire for the nurse educator and the interview with the cardiologist is in narrative form.
Assumption and Limitations
The researcher has observed through this investigational study a need to update nurses’ current knowledge base on the problems associated with concussions and head trauma mainly due to the recent and current concerns of concussion/head trauma awareness in sports. What is equally important is to provide nurses with the information they feel will assist them with current assessments, interventions, and practices. This problem is worldwide, and current medical information is needed as research in this area continues to make new advancements. Nurses, both LVNs and RNs, must remain knowledgeable to reflect the current best practices due to the newly increase of concussion awareness.
Human Subjects Protection
The researcher has completed online training with the National Institute of Health and has received certification in Protecting Human Research Participants (see appendix D). The researcher has also taken several collaborative courses at Western Governors University, including instruction on values and ethics, all leading toward this potential research project. Consents to conduct research among three individual school districts has been obtained and forwarded to the chairperson. Participants have been told not to disclose their names, and identifiable markings have been removed. The data collected do not reveal any participant identifiable data, and it is stored in a secured combination safe that is known only to the researcher. Confidentiality will continue to be maintained. The safe itself is also secured in a locked room in which the researcher has possession of the key. The collected analyzed data is stored in a secured safe, and later, it will be destroyed upon permission by Western Governors University.
The participants have been informed that they have the right to participate or withdraw at any given time and that there are no potential risks or costs involved in this study; informed consent is not needed.
Summary
This qualitative research design utilizing triangulation identified pertinent data and assessed current nurses’ knowledge related to the assessment of head injuries in athletic children, and it gained knowledge on what the school nurses believe they need to adequately assess and manage head injuries in athletic children. Not only did this study seek nurses’ knowledge but it also gained knowledge from medical experts that assisted nurses to remain current on pertinent information that will benefit the health of the athletic child while promoting growth, knowledge, and collaboration in the public schools and in the public health arena. Chapter 4 presents the finding of this research study.
Chapter 4
Findings
Overview
After consent was given from each participating school district, a questionnaire that was developed by the researcher was distributed among three different school districts within the region of the San Francisco Bay Area in California. The questionnaire gathered demographic data and information about the nurses’ current knowledge in the assessment of head trauma in young athletes. Once this vital information had been collected and obtained from all three school districts, graphical analysis was used as a means to interpret the data by categorical organization (Gay et al. 2009).
Analysis of Data
The results from the nurses’ questionnaire were interpreted by the Microsoft ® Tableau and the ATLAS.ti ® software and then placed into figures 1 and 2 included in tables 2-9. The initial data from the spreadsheets included values of 1, which represented that the respondents mentioned it—any blank fields reflected that no comments/statements were made or observed. Concepts of nausea and vomiting and signs and symptoms were combined as one group. The total number of participants in the study was 40, which included 36 ed nurses (RNs) and 4 licensed vocational nurses (LVNs). The ages of the nurses ranged from 24 to 67, and a total of 5 nurses chose not to make an
entry in this category. The minimum age was 24 while the mean age was 52. The median age was 55, and the maximum age was 67. The minimum year of practice was 1 year with a mean practice of 24.22 years. The median number of years practice was 26 with a maximum number of years totaling 44. Table 2 summarizes the two types of nurses represented in this study, the total number of RNs, the total number of LVNs, and the sum of all nurses participating in this study. The total number of RNs that participated in this study was 36, and the total number of participating LVNs was 4. While there was 100% participation among the LVNs employed in the three school districts, they represented 10% of the participants in this study. There was also 100% participation among the RNs, and they represented 90% of the total participants in this study (see table 2).
Table 2: Number of Participants
ed Nurses (RNs) Licensed Vocational Nurses (LVNs) Total Number of Nurses 36
4
40
Table 3 represents how the participants responded to the age category in the questionnaire. The participants that voluntarily participated completed an informed consent form that included confidentiality, risks involved, agreement, researcher’s , and demographics that included licensure, age, and years practicing (see appendix A). Table 3 summarizes the minimum, mean, median, and maximum age of the participants.
Table 3: Age of the Participants
Minimum Age Mean Age
Median Age
Maximum Age
24
55
67
52
Table 4 represents the responded signs and symptoms (S/Sxs) of assessment mentioned by the nurses including the number and percentage of nurses that mentioned each symptom. The following responses were given in response to question 1: “What is the current practice for nurses assessing head injuries in children?” Table 4 demonstrates that 30% of the nurses would check the trauma site, and 22.5% would assess for changes in vision, and 35% would assess pupil size. The other assessments the nurses felt needed attention are listed in table 4 as well but shows an increase in what they felt is current practice in assessing head injuries in children.
Table 4: Nurses’ Responses to Question 1
Current Practice in Assessing Neurologi- cal Checks Observa- tion Check Trauma Site # of Nurse Responses 25 28 12 % of Nurse Responses 62.5 % 70.0% 30.0%
Table 5 represents the knowledge of the signs and symptoms (S/Sxs) the nurses would observe in the course of an acute concussion. The low value of percentages is in the areas of assessing for blurred vision, drowsiness, and pupil size, and their responses were 40%, 62.5%, 30%, and 27.5%, respectively. The highest responses stated by the nurses in observing for signs of an acute concussion were to observe for headaches and changes in level of consciousness (LOC) in which both ed for 70% of the responses. Observing for nausea was included at 65% of the responses by the nurses. Table 5 demonstrates their responses to question 2: “What are the signs and symptoms (S/Sxs) of an acute concussion?”
Table 5: Nurses’ Responses to Question 2
Nurses Reported S/Sxs
Blurred Vision Dizziness Drowsiness Headaches
# of Nurses Reported S/Sxs 16
25
12
28
% of Nurses Reported S/Sxs 40.0%
62.5%
30.0%
70.0%
Table 6 illustrates the results of question 3: “What signs should be observed in children with acute head injuries?” The nurses responded that they would assess for blurred vision in a child with an acute head injury at 32.5% and included drowsiness as part of the assessment ing for 45% of all responses. Assessing for blurred vision and drowsiness ed for less than half of the responses by the nurses. The nurses stated they would also observe for signs of dizziness and headaches in which both responses ed for over 50%. Observing for headaches received the highest percentage area mentioned for assessing children with an acute head injury as evidenced by 57.5% of the respondents.
Table 6: Nurses Responses to Question 3
Nurses Reported S/Sxs
Blurred Vision Dizziness Drowsiness Headache
# of S/Sxs Reported by Nurses 13
20
18
23
% of S/Sxs Reported by Nurses 32.5%
50.0%
45.0%
57.5%
Table 7 represents the nurses’ responses to question 4. There are several responses with low values in every area mentioned except assessing for headaches, which ed for 70% of the nurses’ responses. In table 7, the majority (70%) of the nurses reported that athletes will report headaches as a primary sign of a concussion/head injury while reports of dizziness, LOC, nausea, and pupil size ed for less than 40% of responses by the nurses. Table 7 includes the areas the nurses mentioned that they would assess for in regards to question 4: “What signs are usually reported by athletes with concussions/head injuries?” Their responses are as follows:
Table 7: Nurses’ Responses to Question 4
Nurses Reported S/Sxs
Drowsiness Headache LOC
Nausea Pupil Size
# of Nurses that Reported the S/Sxs 3
28
14
13
2
% of Nurses that Reported the S/Sxs 7.5%
70.0%
35.0% 32.5% 5.0%
Table 8 represents the responses from question 5: “When should athletes be cleared to return to play after receiving a concussion? Table 8 reveals that 75% of the nurses believed that an athlete should be able to return to play in the games post sustaining a concussion after the athlete has been seen and cleared by a physician. The responses demonstrate that 30 out of 40 nurses believed that an athlete’s clearance should be granted upon clearance from the medical doctor. Three nurses chose not to respond to this question while 7.5% of other nurses felt that an athlete can return to games of play when symptoms subside. There were 2.5% of nursing respondents that stated an athlete should be cleared post injury within several weeks while 2.5% stated within 15 minutes. Another 2.5% reported the athlete can return to play post assessment while another 2.5% reported an athlete should be cleared post injury in about 15 minutes.
Table 8: Nurses’ Responses to Question 5
Nurses’ Responses
Within several weeks After MD visit Within 15 min
# of Nurses Response to Each Category 1
30
1
Figure 1 and figure 2 clearly demonstrate the results of question 5. The majority of nurses (75%) believed that an athlete must be cleared by a physician before returning to the games post concussion/head injury. There were 7.5% of the participants that did not respond to this question. Figure 1 and 2 are additional figures and views that reveal how the nurses have responded to this question. These figures were adapted from the Microsoft ® Tableau software for qualitative data analysis.
Figure 1: Nurses’ Response to Question 5
Figure 2 is a bar graph that s the findings of question 5 and demonstrates the results in a different view and suggests that 75% of all nurses that participated in this study believed that an injured athlete’s clearance for returning to play is most definitely in the hands of the physician.
Figure 2: Nurses’ Response to Question 5
Table 9 represents the nurses’ responses to question 6: “Is the Glasgow Coma Scale utilized in the assessment of head injuries in children?” The answers varied in responses significantly, with 25% stating the GCS is not used in their school district, another 25% revealing yes, the GCS is used in their school district. Five percent of the participants chose not to answer while another 5% stated that they do not know if the GCS is used, and 7% stated the GCS is used in a modified version. Another 7% believed the GCS is to be utilized in the ER setting. There were 12.5% of nurses that stated the GCS is not used in a school setting and 7% stating the GCS is not utilized in the assessment of head injuries in children. Interestingly, 2% commented, “Why not?” Please see table 9.
Table 9: Nurses’ Response to Question 6
Nurse Responses to the Usage of the GCS in School Setting No Response Not in school sett The # of Reported Responses in Each Subdivision
2
5
The Nurse Educator
In addition to the six questions addressed to the three school district nurses, two additional questions were addressed to a nurse educator that is a professor currently practicing and teaching nursing students at the university level within the San Francisco Bay Area. The nurse educator has 30 years of experience as a nurse and has provided additional insight in the topic of head injuries in athletic children. Please see question 1 and question 2.
Question 1:
1. “What additional knowledge do you feel nurses need to adequately assess and manage head injuries in athletic children?”
Nurse Educator’s Response to Question 1:
The nurse educator stressed the importance that “Nurses need knowledge of actual and/or potential complications that result from repetitive sports injuries in children. Nurses also need knowledge of how head injuries in children sustained from sports differ from head injuries in adults sustained from sports.”
Question 2:
2. “What is the current practice and guidelines for assessing and evaluating acute concussions/head injuries in athletic children within the ER and trauma centers?”
Nurse Educator’s Response to Question 2:
“It has been discovered that in a major medical facility and its hospitals, there are no current practice and/or guidelines that exist for assessing and evaluating concussions/head injuries sustained from sports in children within the ER and trauma centers. The standards of practice include treating and monitoring the care of the patient with increased intracranial pressure.”
The Cardiologist
The following research questions address the same three specific interview questions asked of the cardiologist who is a well-qualified author, surgeon, and consultant for an NBA team. The cardiologist is board certified in internal medicine, cardiology, and advanced clinical training and education thus qualified to provide medical expertise.
Interview Question 1:
“What is second impact syndrome, and how does a blow to the chest affect a cerebral injury?”
Cardiologist Response to Question 1:
“Second impact syndrome [SIS] is a process whereby a second trauma to the brain soon after the first concussion can lead to a rapid and catastrophic brain
injury and death. The second trauma does not need to be a head trauma. It could happen with even a hard chest injury, which can in return propagate a shock wave to the head.”
Question 2:
“What additional knowledge do you feel nurses need to adequately assess and manage head trauma/concussions?”
Cardiologist Response to Question 2:
“The public and the nurses should be aware of patients showing up to the ER with head trauma post concussion and get a good history and note if this was a first or a second concussion, especially in teenagers. A second concussion should be evaluated for neurological deficits ASAP and given the proper management.”
Question 3:
“What additional knowledge do you feel nurses need to assess a second impact injury, and how would this relate to documentation?”
Cardiologist Response to Question 3:
“Additional factors that nurses should be aware of are the need for an immediate response if you detect a second head trauma injury. The more one delays, the
worse the outcome. On the exam, do a thorough evaluation of pupil reflexes and note any signs of confusion. More importantly, make sure that the athlete does not return to athletic activities for at least 6 weeks.”
Triangulation of Data
The findings of low percentage values in the assessment of visual changes in concussions or head injuries (see tables 4, 5, 6, and 7) the need for further education and also the cardiologist’s urge for nurses to include and incorporate visual assessment in the assessment of children with head injuries. The evaluation of headaches when an individual has sustained a concussion is one of the significant and accurate findings as represented by the nurses responding at 70%. Experiencing headaches is one of the most frequent complaints (Castellanos and Oakes 2011; Kirkwood et al. 2006; Zink and McQuillan 2011). The literature review also s the nurses’ percentage of 75% as well as s the cardiologist in that a child should not be allowed to return to game of play until he has been cleared by the physician. It is the goal of this qualitative triangulation study to educate medical professionals as well as encourage them to stay current in the areas of sports-related concussions and head injuries because the effects, if not treated, can be fatal. Triangulation in this study also reveals to be accurate and provide exceptional documentation as voiced by the cardiologist and verified in the literature review. A comprehensive literature review has been completed on the topic of head injuries and concussions. The usage of the Glasgow Coma Scale in the school setting has been ed by the literature review as needed, and it can be used as a prehospital tool evaluating the conscious state of a person (Gabbe et al. 2003). The literature review assesses the need for promoting safety to athletes, education, and health care maintenance. The questionnaires were completed by the participants with their consents and revealed their willingness to be proactive in the school setting in which they are so committed.
Results and Interpretation
The first four questions on the questionnaire that was distributed to the school nurses have similar types of observation that are required in the assessment of head injuries, and it is important to know that concussion and head trauma are used interchangeably as research continues. Table 4 in this study demonstrates that 30% of the nurses would check the trauma site, and only 22.5% would assess for changes in vision, and 35% would assess pupil size. The other assessments the nurses felt needed attention are listed in table 4 as well but shows an increase in what they felt is current practice in assessing head injuries in children. Recent data state the importance of assessing for a variety of neurological and cognitive problems including alterations in vision (Zink and McQuillan 2011). Table 5 illustrates the s/sxs the nurses would assess in an acute concussion. There were several signs mentioned, but 40% mentioned blurred vision, 30% said drowsiness, and 27% stated pupil size out of 40 respondents. According to the nurses’ responses for question 1, their answers reflect observation, neurological, and trauma checks. Observation would be changes in behavior, neuro, which is self-explanatory, and trauma checks being physical but visual around the site of impact. According to the percentages, there is a clear shift between the three areas even though the responses from questions 2-4 have common . The percentages from questions 2-4 have common theme . The difference in percentage from each theme for each question varies although the type of injury is the same (with different degree of severity); there is clear evidence of inconsistent treatment. In other words, practitioners who treat concussed children may not necessarily know what they are looking for as this area as a new research is presently ongoing with new discoveries. Question 4, however, addresses “What signs are usually reported by athletes with concussions and head injuries?” The areas mentioned by the nurses varied in small percentages, but 70% of the nurses revealed the need to assess subjective statements of headaches. According to the questionnaire from the nurse educator, there are no guidelines in place for children with head injuries in the ER and trauma rooms in some hospitals. In question 5, table 8 demonstrates that 75% of nurses believe a child should not be cleared to play post concussion until cleared by a physician. The usage of the Glasgow Coma Scale had a variety of responses. Table 9 represents the nurses’ responses to question 6: “Is the Glasgow Coma Scale utilized in the assessment of head injuries in children?” The answers varied in responses significantly, with 25% stating the GCS is not used in their school district; another 25% revealing, yes, the GCS is used; and 3 participants stating the GCS usage in a modified version. All other entries of
assessment are listed in table 9. The GCS has been found to be a tool used as a hospital precursor in the evaluation of the conscious state of a person (Gabbe et al. 2003). There were several findings in this study. The nurse educator discovered that there were no significant guidelines in the ER and trauma center at a major hospital and all its hospitals for the treatment of sports-related head injuries in children. The guidelines in place are for any persons presenting with increased intracranial pressure. The nurse educator proposed that the guidelines for children with concussions should be different than head injuries sustained from other causes. The nurse educator felt that nurses would benefit from additional knowledge provided in the areas of actual or potential complications that result from repetitive sports injuries in children. Additional knowledge needed would be how head injuries in children sustained from sports differ from head injuries in adults sustained from sports. The cardiologist interview suggests that the public and the nurses should be aware of patients showing up to the ER with head trauma post concussion and get a good history and note if this was a first or second concussion, especially in teenagers. The cardiologist was clearly stating that a second concussion should be evaluated for a neurological deficit as soon as possible (ASAP) and to give the proper treatment and management. The cardiologist also discussed second impact syndrome (SIS) and the need for immediate response and good documentation. It is important to know that the more delays, the worse the outcome. The cardiologist suggests an exam doing a thorough evaluation of the pupil reflexes and observing for any signs and symptoms of confusion. More importantly, make sure that the athlete does not return to athletic activities, which depends on severity, and at least six weeks.
Summary
This study examined demographic data that included the participants’ type of nursing licensure, their age, and their number of years practicing as a nurse. The questionnaire was designed to observe school nurses’ current knowledge and to identify what nurses feel they need to adequately assess head injuries in athletes. The results were based on the nurses’ responses to assessment questions with the identification of different themes, values, and responses. Certain concepts were combined and comparisons were made to the interview of a cardiologist that
provided knowledge necessary for nurses to adequately assess children with head injuries. Comparison was also made to a nurse educator’s questionnaire that provided areas of needed research and what knowledge nurses need to adequately assess head injuries in children. The purpose of this study was to assess school nurses’ current knowledge related to the assessment of concussions and head injuries in athletes as well as to obtain additional knowledge that nurses feel they need to adequately assess head injuries in athletes. The participants, along with their consents, revealed their willingness to be proactive in the school setting in which they are so committed. The data collection and analysis utilized in this study provided both tables and figures as measures to demonstrate responses from school nurses of multiple school districts. The information obtained will encourage education of head injuries and concussions in the public schools and public health arena as well as encourage new information into the ER and trauma centers. Additional information from this study will increase education among families, caregivers, and school officials. Further education is needed due to several inconsistencies in responses by the participants, especially since research in this area is ongoing and consistently making new advances, which is greatly needed and appreciated. Chapter 5 will present and discuss the implications, limitations, recommendations, and conclusions of this study in relation to its findings.
Chapter 5
Discussion and Conclusions
Overview
This final chapter discusses the findings, implications, and limitations of this study as interpreted by the researcher. Additional inclusions within this study will be suggestions and recommendations that will enhance assessment skills among those who treat persons with head injuries based on the results of this study and will be finalized in the conclusion.
Discussion
The research questions addressed in this study will be discussed individually and listed as follows:
1. What are school nurses’ current knowledge related to the assessment of head injuries in athletic children? 2. What additional knowledge do school nurses believe they need to adequately assess and manage head injuries in athletes?
Nurses Current Knowledge
This study did discover that most of the school nurse respondents recognized that the medical doctor is the key person to determine full recovery of an athlete that has suffered a concussion/head injury regardless of type. The physician, the ATC (certified athletic trainer), and other medical professionals work together to restore the athlete to preinjury status (Guskiewicz et al. 2004). This study has also identified three types of checks as mentioned by the nurses that they would observe for when assessing children with head injuries. The majority checks identified by the participants are neurological (neuro), observation, and trauma. Neurological checks are self-explanatory and observation checks, resulting in observing for changes in behavior while trauma is physical but visual damage around the region of impact. According to the percentages in the way the nurses responded, there is a definite clear shift between the three checks identified. It would seem that all medical practitioners would have mentioned these areas of assessment for head injuries regardless of training. It is important to note that initial assessment involves eliminating cervical spine injury and serious traumatic brain injury and that the most common symptoms of a concussion involve headaches (Scorza, Raleigh, and O’Connor 2012). In several questions regarding the signs and symptoms, observation and signs and symptoms reported by athletes, the majority of nurses recognized that assessing for headaches is a key assessment.
Additional Knowledge Needed
This study discovered that the response questions from 2-4 have common theme . The difference on percentage from each theme for each question varies although the type of injury is the same (with different degree of severity). There is clear evidence of inconsistent treatment, which may mean that practitioners may not necessarily know what they should be looking and observing for, as head injuries are of different degrees of severity, and the are presently used interchangeably while research in this area is continually advancing. Exposure may play a key role as those nurses and other practitioners that are more likely exposed are those more likely to assess the type of impact, regardless of the years of practice and age of the practitioner.
The use of the Glasgow Coma Scale has been used mostly in the hospital setting although its use in the school districts further creates ambiguity on what needs to be done. The responses from the nurses varied significantly in regards to the GCS’s usage in the school setting and suggest a need for knowledge in this area. Research has suggested that this tool would be beneficial (Gabbe et al. 2003). This is very interesting and opens the door to its usage as a hospital precursor within the school setting to record the conscious state of a person thus depending upon the severity of the injury. Yes, it is very important to know an athlete’s conscious state upon injury, but it is also important to know an athlete’s baseline neurological and cognitive status prior to games of play. Research has identified the necessity of obtaining neurocognitive, mental status, and postural stability (balance) tests prior to injury to serve as baseline data that can be compared to test results post injury. Therefore, knowing both the athlete’s preinjury status and postinjury status is beneficial for the athlete’s total well-being. There should also be a symptom scale or checklist in place (Guskiewicz et al. 2004; McCrory et al. 2009; Piebes et al. 2009). This additional knowledge will help nurses to manage and assess key factors in the identification of head injuries in athletes. The application of a symptom scale, checklist, and guidelines specific to concussions and head injuries in children will also serve as a reference guide and will further assist nurses in identifying key areas of assessment in injured athletes. This study discovered that assessing for problems with vision and pupil reflexes as suggested by the cardiologist was not a key assessment area with the nurses as identified by the low percentage rate of responses. Assessing for visual changes in head injuries has been a key factor in this study and throughout other research studies of this nature and is suggestive that all medical practitioners regardless of education should include this area of assessment. In this study, the nurses identified areas of assessment in the athletic child with a concussion/head injury and identified areas of self-reported symptoms by athletes. The responses from the nurses in regards to self-reported symptoms lacked several key assessment components that have been identified through previous research (Guskiewicz et al. 2004; Zink et al. 20011). Even though the nurses’ responses varied significantly, the total responses recorded were to assess the trauma site, check pupil size, check for blurred vision, headaches, drowsiness, dizziness, level of consciousness, nausea, and vomiting. Guskiewicz (2004) and Zink (2011) have identified the following areas to observe in both concussions and self-reported symptoms:
1. Assess cervical spine and cranial nerves recording the time of initial injury 2. Changes in level of consciousness (LOC) 3. Alterations in memory and concentration 4. Self-reported symptoms (headache, ringing in the ears, nausea/vomiting, feeling in a fog, problems sleeping, fatigue, drowsiness, sensitivity to light or noise, loss of balance, unsteadiness, double vision) 5. Check for alterations in vision 6. Balance problems 7. Check vital signs (v/s) and LOC every 5 minutes post concussion 8. Check for presence of amnesia
Scorza (2012) identifies that an initial assessment of a concussion involves the following:
1. Eliminating cervical spine injury and serious traumatic brain injury 2. Observing for signs and symptoms of a headache
The medical examiner in this study suggests assessing the following areas in second impact syndrome:
1. Do a thorough evaluation of the pupil reflexes. 2. Get a good history, noting if a second impact has occurred.
3. Check for neurological deficits as soon as possible (ASAP). 4. Do thorough documentation, recognizing this is an immediate response needing immediate attention by a physician.
An athlete can only return to full participation in the games once cleared by the medical physician or a trained expert in the field of concussion as long as there are no recurrent signs and symptoms present (Guskiewicz et al. 2004). This study has discovered that there is a major hospital along with all its d hospitals that do not have a guideline in effect for the treatment of children and athletic children with concussions and head injuries specifically. Without specific guidelines in place, certain areas of assessment will no doubt get missed, and the injuries occurring from a second impact without initial documentation, assessment, and the appropriate intervention can be fatal. This study has revealed that continuous education and training is critical, and the utility of the GCS is a good framework and tool for nurses to use in the school setting to further assist the emergency staff of a client’s initial conscious state and/or deterioration upon injury.
Implications
As a result of this study, several implications have been identified. The first implication would be that the most current knowledge of assessing, treating, and managing athletes with head injuries/concussions must be provided to school nurses and those who are involved in the care of the injured athlete by nursing supervisors and s. The second implication would be for nursing supervisors and nursing s to remain current with additional knowledge as new research progresses. The third implication would be for nursing supervisors and other staff to assist and provide concussion and head-injury awareness among school personnel,
coaches, athletic trainers, school s, parents, and all who are involved in the care of the injured athlete. The fourth implication would be for hospital s and supervisors to increase concussion awareness among the ER and trauma centers and implement guidelines specific to concussion/head injuries in children. These guidelines should be different than those for injuries sustained from other causes. The fifth implication would be for those persons involved in the individualized plan of care (IPC) of the athlete to incorporate the most updated information regarding current treatment modalities of concussions /head injuries in place upon the athlete’s return to school. The final implication would be for nursing supervisors and s to include the use of the Glasgow Coma Scale (GCS) into the policy and procedures for use in emergent situations. The GCS should be implemented in the school districts.
Limitations
This study did not take into consideration the length of time needed to incorporate three school districts along with the restrictions beyond the researcher’s control. The restrictions were necessary as this project was workable but around each school districts request to maintain their normal schedule upon each districts individual curriculum to avoid interruptions of the daily routines of the children, which is necessary. This was beyond the researcher’s control; however, it was the researcher’s choice to include three school districts versus one school district to increase the validity of the findings by going beyond the standard realm. The researcher views the findings of this study useful in incorporating a new area within the school system while increasing knowledge, assessment, needed interventions, and growth among not only school nurses but among all medical professionals and those persons involved in the plan of care with an injured athlete.
Recommendations
Based on the findings of this study, the following recommendations are made:
1. To provide the most current and up-to-date facts of assessment and treatment modalities surrounding head injuries and concussions of athletes to the school nurses by way of literature, fact sheets, current research studies, and in-services thus reviewing the school districts policies and procedures noting changes 2. For nursing supervisors, s, and those who are in leadership positions to remain current with new research findings specific to head injuries in athletes and incorporate new information into policies and procedures 3. To promote concussion awareness to school officials, coaches, athletic trainers, school staff, and parents through literature, fact sheets, and providing resources that are specific to each profession. Coaches and ATCs (certified athletic trainers) have specific new requirements and guidelines pertinent to their profession and should follow accordingly. Parents need to be provided with resources and information as well on what to look for in their child who has suffered a head injury and how to manage the athlete child in the home 4. To create concussion and head trauma guidelines, policies, and procedures within the emergency room (ER) and trauma centers specifically for injured athletic adolescent children by nursing s acting as patient and political advocates influencing decisions and actions 5. To have a concussion/head-injury guideline in place for the injured child upon the return to the school environment as part of the IEP (individualized education program) 6. To have nursing supervisors, s, educators, and public health include usage of the Glascow Coma Scale (GCS) into the policy and procedures
Conclusions
The findings of this research study s that there is a need to incorporate new research findings of concussions and head injuries into the school system. The information within this research design and the data discovered should be used to encourage knowledge among nurses, other medical professionals, coaches, certified athletic trainers (ATCs), school officials, instructors, and parents. The data should be used by nurses to enhance their assessment and observation skills to return the injured child to his/her preinjury status. The data should promote concussion and head-injury awareness by assisting medical professionals to remain current in treatment interventions and modalities, encourage supervisors and nurse educators to remain current in new research findings. The data should also encourage nursing supervisors to include guidelines of concussion and head injuries in the IEP (individualized education plan) and have it enforced upon the return of the athlete into the school environment. The data discovered suggests that nurse supervisors and educator include the Glasgow Coma Scale as a tool and hospital precursor to determine the conscious state of the injured for the ER and trauma centers. It is imperative that nurse educators study and address new research findings while taking into consideration that research in this area is ongoing. Nursing supervisors, public health nurses, and nurse educators must increase knowledge in this area of study by providing the community and nurses with facts, guidelines, continuous education, training, information, and referrals, thus encouraging nursing staff to provide the most optimal care in the concussed athlete. The data should be used to increase competency, confidence, and satisfaction of care within the nurses themselves while demonstrating their effectiveness in a job so rewarding.
Appendix A
Your participation in this study is voluntary and all information will be confidential. Entries and submissions are confidential. You will not be retaliated against, reprimanded, or dismissed for your participation, and there are no risks or costs involved. If you agree to participate in this study, it will be acknowledged by completing this questionnaire. Your input will provide information of your knowledge of assessment in athletes with head injuries and will provide knowledge to further assist children with brain trauma. Should you have any questions concerning this questionnaire, please Sandra Merriweather, RN, BSN, PHN, MSN, student at Western Governors University.
*Please do not write your name on this form.
ed Nurse _________ or Licensed Vocational Nurse _________
*Please check one of the above
Your age: ____
Number of years practicing nursing: ____
1. What is the current practice for nurses assessing head injuries in children?
2. What are the signs and symptoms of an acute concussion?
3. What signs should be observed in children with acute head injuries? 4. What signs are usually reported by athletes with concussions/head injuries?
5. When should athletes be cleared to return to play after receiving a concussion?
6. Is the Glasgow Coma Scale utilized in the assessment of head injuries of children?
Appendix B
Your participation in this study is voluntary and all information will be confidential. Entries and submissions are confidential. You will not be retaliated against, reprimanded, or dismissed for your participation. There are no risks and no costs involved. If you agree to participate in this study, it will be acknowledged by completing this questionnaire. Your input will provide information of your knowledge of assessment in athletes with head injuries and will provide knowledge to further assist children with brain trauma. Should you have any questions concerning this questionnaire, please Sandra Merriweather, RN, BSN, PHN, MSN, candidate at Western Governors University.
*Please do not write your name on this form.
Nurse Educator _________ or Advanced Practiced Nurse _________
*Please check one of the above
Your age: ____
Number of years practicing nursing: ____
1. What additional knowledge do you feel nurses need to adequately assess and manage head injuries in athletic children?
2. What is the current practice and guidelines for assessing and evaluating acute concussions/head injuries in athletic children within the ER and trauma centers?
Appendix C
Your participation in this study is voluntary and all information will be confidential. Entries and submissions are confidential unless otherwise stated by entry checked below. You will not be retaliated against, reprimanded, or dismissed for your participation and there are no risks or costs involved. If you agree to participate in this study, it will be acknowledged by completing this questionnaire. Your input will provide information of your knowledge of assessment in athletes with head injuries and will provide knowledge to further assist children with brain trauma. Should you have any questions concerning this questionnaire, please Sandra Merriweather, RN, BSN, PHN, MSN, candidate at Western Governors University.
Physician: Yes/No (circle) and Physician Specialty:
______________________________________
*Please check one of the above
Your age: ____
Number of years practicing: ____
Do you agree to discuss findings of researcher’s study if requested?
YES or NO (please circle)
1. What is second impact syndrome, and how does a blow to the chest affect a cerebral injury?
2. What additional knowledge do you feel nurses need to adequately assess and manage head trauma/concussions?
3. What additional knowledge do you feel nurses would need to assess a secondimpact injury, and how would this relate to documentation?
Appendix D
Reference
Bay, E. (2011). Mild traumatic brain injury: a Midwest survey about the assessment and documentation practices of emergency department nurses. Advanced Emergency Nursing Journal, 33, 1, 71-83. Carroll L. J., Cassidy J. D., Peloso P. M., et al. (2004). Prognosis for mild traumatic brain Injury. Results of the Who Collaborating Centre Task Force on mild traumatic brain injury. Journal of Rehabilitation Med, 43, 84-105. Castellanos, S., Oakes, C. (2011). Jantz hopeful for lasting legacy to grow from tragedy. The Aurora Sentinel, 4, 7. Centers for Disease Control and Prevention. Sport-related injuries among high school athletes-United States, 2005-2006 school year. MMWR Morb Wkly Rep. 55, 38: 1037-1040. Centers for Disease Control and Prevention. (2011). Heads Up: concussion in high school sports-fact sheet for athletes. http://www.cdc.gov/concusiion/pdf/AthletesFact_Sheet_a.pdf. Cook R. S., Schweer, L., Shebesta K. F., et al. (2006). Mild traumatic brain injury in children: Just another bump on the head? Journal of Trauma Nursing, 13, 2, 58-65. Frommer L. J., Gurka K. K., Cross K. M., et al. (2011). Sex differences in concussion symptoms of high school athletes. Journal of Athletic Training, 46, 1, 76-84. doi: 10.4085/1062-6050-46.1.76. Gabbe B. J., Cameron P. A., Finch C. (2003). The status of the glascow coma scale. Emergency Medicine, 15, 353-360. Gavett B. E., Stem R. A., McKee A. C. (2011). Chronic traumatic encephalopathy: a potential late effect of sport-related and subconcussive head trauma. Clin Sports Med., 1, 30, 1, 179-188.
Gay L. R., Mills G. E., Airasian P. (2009). Educational research: competencies for analysis and applications. Upper Saddle River, New Jersey: Pearson Education, Inc. Gessel L. M., Fields S. K., Collins C. L., Dick R. W., Comstock R. D. (2007). Concussion among United States high school and collegiate athletes. Journal of Athletic Training, 42, 495-503. Guskiewicz K. M., Bruce S. L., Cantu R. C., Ferrara M. S., Kelly J. P., McCrea M., et al. (2004). National Athletic Trainers’ Association Position Statement: Management of sport-related concussion. Journal of Athletic Training, 39, 280297. Guskiewicz K. M., Marshall S. W., Bailes J., et al. (2005). Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery, 57, 4, 719-26. doi: 10.1227/01.NEU.0000175725.75780.DD. http://www.wikipedia.org/ http://www.nflevolution.com/—Safety for your kids Kelly J. P., Rosenberg J. H. (1997). Diagnosis and management of concussion in sports. Neurology 48, 575-580. Kirkwood M. W., Yeates K. O., Wilson P. E. (2006). Pediatric sport-related concussion: A review of the clinical management of an oft-neglected population. Pediatrics, 117, 1359. Iavagnilio C. (2011). Traumatic brain injury: Improving the patient’s outcome demands timely and accurate diagnosis. Journal of Legal Nurse Consulting 22, 3, 3-10. McCrory P., Meeuwisse W., Johnston K., Dvorak J, et al. (2008). Consensus Statement on concussion in sport-the 3rd international conference on concussion in sport held in Zunich November 2008. Journal of Science and Medicine in Sport, 12, 340-351. Miele V. J., Norwig J. A., Bailes J. E. (2006). Sideline and ringside evaluation for brain and spinal injuries. Neurosurgery Focus, 21.
Mittenberg W., Wittner M. S., Miller L. J. (1997). Post concussion syndrome occurs in children. Neuropsychology, 11, 447-452. Moser R. S., Shatz P., Barry D. (2005). Prolonged effects of concussion in youth athletes. Neurosurgery, 57(2), 300-306. Needle & Ellenberg, P. A. (2011). Football player who killed himself did have serious brain injury. Brain Injuries, May 3, 2011. Omalu B. I., Fitzsimmons R. P., Hammers J., Bailes J., (2010). Chronic traumatic encephalopathy in a professional American wrestler. Journal of Forensic Nursing, 130-136. doi: 10.1111/j.1939-3938.2010.01078x. Omaulu B. I, Bailes J. E., Fitzsimmons R. P., Hammers J. L., et al. (2010). Chronic traumatic encephalopathy, suicides and parasuicides in professional American athletes. Am Forensic Med Pathology, 31, 2, 130-132. Omalu B. I., DeKosky S. T., Hamilton R. L., et al. (2005). Chronic traumatic Encephalopathy in a national football league player. Neurosurgery, 57, 1, 12834. Omalu B. I., Dekosky S. T., Hamilton R. L., et. al. (2006). Chronic traumatic encephalopathy in a national football league player: part II. Neurosurgery 59, 5, 1086-92. Omalu B. I., Hamilton, et al. (2010). Chronic traumatic encephalopathy (CTE) in a national football league player: Case report and emerging medical questions. Forensic Nurse, 6, 1, 40-6. doi:10.1111/j.1939-3938.2009.01064.x. Omalu B. I., Hamilton R. L., Kamboh M. I., Dekosky S. T., Bailes J. (2010). Chronic traumatic encephalopathy (CTE) in a national football league player: Case report and emerging medicolegal practice questions. Journal of Forensic Nursing, 40-46. Pennington N. (2010). Head injuries in children. The Journal of School Nursing, 26,1, 26-32. Piebes S. K., Gourley M., Valovich MCleod T. C. (2009). Caring for studentathletes following a concussion. The Journal of School Nursing, 25, 270. doi: 10.1177/1059840509339782.
Sarmiento K., Mitchko J., Klein C., Wong S. (2010). Evaluation of the centers for disease control and prevention’s concussion initiative for high school coaches: “Heads up concussion in High School Sports.” J School Health, 80, 112-118. Scorza K. A., Raleigh M. F., O’Connor F. G, (2012). Current concepts in concussion: evaluation and management. Am Family Physician, 82, 2, 123-32. Trudel T., Tina M., Scherer M., Elias E. (2011). Understanding traumatic brain injury: An introduction. Exceptional Parent, 41, 7, 33-7. Virginia Brain Injury Lawyers (2011). Duerson suicide due to repeated traumatic brain injuries. Brain Injury Law Center, 6, 11. Retrieved from: //http://www.brain-injury-law-center.com/2011/06/11/duerson-suicide-due-torepeated-traumatic-brain-injuries/. www.cdc.gov/concussion/headsup/high_school.htm Zink E. K., McQuillan K. (2005). Managing traumatic brain injury. Nursing 35, 9, 36-44. Retrieved from http://www.nursing2005.com/.
Recommendation Blurps
“This is an excellent and worth while project. I thought the two research questions posed are q
“Many professional football players sustain concussions that can result in long-term damage o
“. . . you are obviously ionate about this medical condition and the need to educate medic
“Unbelievable, unbelievable! What a great purpose and overlooked issue. You’ve explained ev
“This is a fascinating research study that reveals far reaching and serious implications for our
Sandra Merriweather has wrapped her arms around our children and has told significant facts
Book Summary
This research study book was designed not only to increase concussion and head injury awareness, but for the researcher to do something about it that would be creative and unique to the medical field, trainers, coaches, school personnel, officials and families. It was necessary to include school nurses as they are always called to the scene of injury along with the coaches and trainers in a school setting and mostly, they are advocates for children and adults alike in any environment surrounding health issues. The results of this study revealed pertinent information that needs further intervention to increase medical knowledge in various areas of health treatment. This book can be used as a quick reference guide for assessing the athletic child with a head injury but as in all emergency cases, seek medical attention as time and documentation are key factors. The ion for this area of study involves being safe and attentive to the signs and symptoms of head injuries. It is necessary to encourage families of children to continue practicing safety measures (Resources: www.nflevolution.com—Safety for your kids; www.cdc.gov/concussion/headsup/high_school.htm.), to be active and healthy while participating in sports and to exercise regularly in avoidance of injuries and sedentary lifestyles, other medical conditions and obesity. It is important to be educated on current facts, while observing, listening and learning from coaches and trainers in the correct training procedures and aspects of a game to be the best one can be. Be knowledgeable and seek information from our current and former athletes. We are all in this together. If any of you have a dream to play in a professional sport or know someone who does, focus on academics, obtain good grades in school, play by the rules, be observant, eat healthy, obtain plenty of rest listen to your trainers and coaches and just maybe we all will see you in the games we all so love!
Sandra’s Bio
Sandra Merriweather is the wife of Former Linebacker Michael Merriweather for the Pittsburgh Steelers, Minnesota Vikings, Jets and Packers. Even though they have a busy lifestyle, Sandra believes in finding time to service communities. She is a member of Off the Field Player’s Wives Assoc., SBNA Nurses Assoc., and she is a member of the CSNO (CA School Nurse Organization) and the NASN (Natl’ Assoc. for School Nurses), Calif. State Sherriff’s Assoc. and the NAA/ Los Angeles Chapter. She is also a ed nurse whose medical career began at age 15. It was during this time that she decided to become a “Candy Striper” and senior volunteer at Kaiser Permenente Hospital in Vallejo, CA while attending Hogan Senior High School. Upon completion of High School she received her AS degree and graduated from Bay City College as a Respiratory Therapist and EKG Technician and became so interested in the medical field that she decided to continue her education in nursing and psychology. Sandra has obtained multiple degrees and certifications in a wide range of medical professions that demonstrates her interest in promoting health awareness. She also attended Dominican University in San Rafael, CA. Sandra received her LVN (Licensed Vocational Nurse) license as well as her BSN degree in nursing. As both a LVN and RN (ed Nurse), she serviced major hospitals in the San Francisco Bay Area and San Joaquin County area through nursing registries and hospital employment. She received her MSN (Masters’ of Science) degree from Western Govenors University with a Specialty in Nursing Education and Research. The hospitals serviced by Sandra were St. Lukes Hospital, Mt. Zion Hospital, UCSF Medical Center of San Francisco, CA., St. Joseph’s Hospital in San Joaquin County and Seton Medical Center in Daly City, CA. where her specialty was in Neurology, outpatient clinics and pediatric services for many years. She has also worked for California Forensic Medical Group servicing Sonoma, Napa, Solano, Yolo and Stanislaus County Sherriff’s Departments attending to both adults and children in the Juvenile System. Her enthusiasm, dedication and charisma to provide positive effective care has led to contracted positions within California’s State Facilities as well. Sandra has also been employed for St. Joseph’s Hospital in the Rapid Care Center and currently holds PHN (Public Health Nurse) Certification. She is presently employed with Lodi Unified School District as a School Nurse/ School
Mental Health Nurse Educator servicing many schools and attending to the wellbeing of childrens’ mental and medical health. Sandra’s comion for both children and adult health care services came from assisting her parents raise 41 foster siblings and helping her parents in their Care Home and Williams Preschool and Kiddie Kare Facility in American Canyon, CA. Her drive is ambition, her talent is varied, her ion is endless and her desire is to promote positive health care is everlasting and most definitely a dream come true.
Mr. and Mrs. Michael Merriweather and Kevin Johnson (Former NBA Basketball Player for the Cleveland Cavaliers and Phoenix Suns; Mayor of Sacramento, CA.
Michael Merriweather with Ray Lewis (Current NFL Player with Baltimore Ravens)
Far Left: Evander Holyfield (Former Undisputed World Champion for both Cruiserweight and Heavyweight.
Sandra Merriweather with Hines Ward (Former NFL’s Wide Receiver of the Pittsburgh Steelers)
Far Left: Dwayne Woodruff (Former Pittsburgh Steelers) Middle: Calvin Sweeney (Former Pittsburgh Steelers) Far Right: Michael Merriweather (Former Pittsburgh Steelers, Minnesota Vikings)
Left: Dwayne Woodruff (Former Pittsburgh Steelers and Common Pleas Court Judge) Middle: Mayor Luke Ravenstahl of Pittsburgh Pennsylvania Right: Michael Merriweather (Former Pittsburgh Steeler and Minnesota Vikings
Far left: John Madden (Former NFL Player, highly Succesful Coach and Sports Announcer) Far Right: Michael Merriweather (Former NFL Player with wife Sandra.
Left: Michael Merriweather (Former Pittsburgh Steelers, Minnesota Vikings, Jets, Packers) Middle: “Bubba” Paris (Former San Francisco 49ers) Right: Jeff Barnes (Former Oakland Raiders)
Left: Kevin Geene (Retired NFL Linebacker and Outside Linebackers Coach for the Green Bay Packers; Los Angeles Rams, Pittsburgh Steelers, & Carolina Panthers Linebacker) 2nd Left: Dennis “Dirt” Winston (Former NFL Linebacker-Pittsburgh Steelers) Middle: Craig Bingham (Former NFL Linebacker-Pittsburgh Steelers/Oakland Raiders) Right: Robin Cole (Retired NFL Linebacker and Pro Bowler-Pittsburgh Steelers; Owner of Robin Cole’s Unforgettable Sweets in Pittsburgh, PA 2nd Right: Michael Merriweather (Retired NFL Linebacker, 3 time Pro Bowler, Steelers MVP-Pittsburgh Steelers, Minnesota Vikings, Jets and Packers)
Right: Ray Lewis Current NFL Player and Linebacker for the Baltimore Ravens; selected to 13 Pro Bowls; Superbowl XLV11
Mrs. Merriweather with NFL current players John Jacoby and Darrius HeywardBey/Oakland Raiders.
Far Right: Nesby Glascow, Former NFL Safety—Baltimore Ravens, Indianapolis Colts, Seattle Seahawks
Right: Rocky Bleier Retired NFL Halfback/Pittsburgh Steelers—Played in the first four Steelers Super Bowl Victories.
Left: Terry Bradshaw Retired NFL Player, TV Host, Actor and Author—Pittsburgh Steelers, MVP and NFL Player of the Year, Quarterback of the Steelers.
“Tony the Tiger” Lopez Boxer.
Michael Merriweather and the Terrible Towel
Left: Brent Jones (Former NFL Player for the SF 49ers) Right: Michael Merriweather—Pittsburgh Steelers, Minnesota Vikings…
Left: Chris Webber (Retired NBA Player)
The Merriweathers enjoying vacationing.
Jerome Bettis (Retired NFL Player/LA Rams and Pittsburgh Steelers)
Left: Michael Merriweather and Midback—Eric Wright with Dave Casper (Tight End Hall of Famer—Oakland Raiders)
Right: Vlade Divac (Retired Yugoslav and Serbian Professional Basketball player, NBA Player and Hall of the Famer—Los Angeles Lakers, Charlotte Hornets and Sacramento Kings.
Mrs. Sandra Merriweather and Fred Biletnikoff (Former NFL wide receiver, coach, and Hall of Famer.
Mr. and Mrs. Michael Merriweather at Mel Blount’s ALL-STAR Celebrity Roast
Left: Calvin Sweeney (Former NFL Wide Receiver—Pittsburgh Steelers) 2nd Left: Louis Lipps with wife (Retired NFL Wide Receiver—Pittsburgh Steelers and New Orleans Saints. MVP Steelers 1985 Right: Mr. and Mrs. Michael Merriweather.
Middle: Dennis Rodman (Retired NBA Player and Hall of Famer/Detroit Pistions, San Antonio Spurs, Dallas Mavericks, LA Lakers.
The Merriweathers with current NFL Players/Oakland Raider’s John Jacoby and Darrius Heyward-Bey.
Left: Mr. and Mrs. Michael Merriweather with Right: Mr. and Mrs. Dwayne Woodruff (Pittsburgh Steelers)
Far Left: Michael Merriweather Pittsburgh Steelers; Minnesota Vikings… Right: Tony Dungy (Former Tampa Bay Buccaneers Head Coach and Former Pittsburgh Steelers
Far Left: Ken Clark (Former Minnesota Vikings) Far Right: Michael Merriweather (Former Pittsburgh Steelers, Minnesota Vikings, New York Jets and Green Bay Packers)
Left: Evander Holyfield—Boxer
Right Back: Ken Clark—Former NFL Player, Minnesota Vikings.
NFL Players and Friends
Right: Wade Phillips—Former Dallas Cowboys Head Coach/Houston Texans Defensive Coordinator.
Former NFL Players for the Pittsburgh Steelers at Mel Blount’s ALL Star Celebrity Roast
Michael Merriweather and Right: Brett Favre (Retired NFL Quarter Back; Green Bay Packers, Atlanta Falcons, NY Jets, Minnesota Vikings.
Left: Adrian Peterson—Current NFL RB for the Minnesota Vikings Middle: Mike Merriweather (Retired NFL Linebacker/Minnesota Vikings, Pittsburgh Steelers, Jets, Packers Right: Brad Childress (Former Minnesota Vikings Coach)
Pittsburgh Steelers Stadium—Heinz Field
Right: Rob Woodson (Retired NFL Cornerback and Safety/Pittsburgh Steelers, Baltimore Ravens, San Francisco 49ers and Oakland Raiders, Hall of Famer.
Left: Robin Cole—Retired NFL Linebacker & Pro Bowler/Pittsburgh Steelers Right: Mike Merriweather—Retired NFL Linebacker & 3 time Pro Bowler/Pittsburgh Steelers, Minnesota Vikings…
Mrs. Sandra Merriweather at Pittsburgh Steelers Stadium Heinz Field.
Michael Merriweather Minnesota Vikings.
Michael Merriweather #57 NFL Linebacker standing beneath picture at Heinz Field of the Pittsburgh Steelers.
Right: Stephone Paige—Retired NFL Player/Kansas City Chiefs and Minnesota Vikings with fan Ray Talley.
Pittsburgh Steelers’ Great Hall at Heinz Field including Michael Merriweather #57.
Michael Merriweather of the Pittsburgh Steelers AKA “Sack Man” - 11 years as a NFL Linebacker - Three time consecutive Pro Bowler (1984-1986) out of the University of the Pacific in the 1982 NFL Draft; 6 seasons as a “Pittsburgh Steelers.” - Named “All Pro” three times (1984, 1986, 1987). - Set a 1984 Steelers’ record for sacks (15) which was 5th best in the NFL - Career Sacks with the Steelers totaled 31 and currently tied 14th on the all-time Steelers’ Sack list; 11 interceptions; 2 defensive TD’s; Steelers’ MVP 1987 - 1989 draft-day trade to Minnesota Vikings 1st-round pick - Led the Minnesota Vikings in tackles in 1990 and 1991 ranking #2 on the team in 1992. - Minnesota Vikings’ 1989 career-high with 189 tackles, scored a TD on an interception return against Detroit making NFL history when he blocked a punt out of the end zone for a safety against the LA Rams in overtime to win the game; the first time an NFL game ended on a safety in overtime. His tackles still rank as the 9th-best mark in team history and no Viking has had as many tackles in a season since. *Merriweather started all 63 games he played for the Vikings. He was named NFC Defensive Player of the Week twice during his Vikings’ Career. - He played on NFC Central Championship teams in 1989 and 1992 advancing to the playoffs both seasons. - Merriweather finished his career playing for the New York Jets and Green Bay Packers both in 1993 and 1994. - Career Sacks: 41 - Interceptions: 18 - Defensive Touchdowns: 4
Left: Michael Merriweather, Retired NFL Linebacker—Pittsburgh Steelers, Minnesota Vikings, Jets and Packers; 3 time Pro Bowler, 5th in the NFL in Sacks; known to fans as “Sack Man”; the first player in NFL history to score the winning points after a game went into overtime with a safety when he blocked a punt out of the end zone. Right: “Ben” Roethlisberger, Current NFL Quarterback—Pittsburgh Steelers. He is the Youngest quarterback in NFL history to win Superbowls. He was only 23 years old when he and the Steelers obtained their second Super Bowl title. He is also known as one of the great ers in NFL history ranking number 10 alltime.
Right: “Ben” Roethlisberger, Pittsburgh Steelers’ Quarterback with Coach Tomlin.
Current Head Coach of the Pittsburgh Steelers: Coach Tomlin
THE NFL GAMES IN ACTION!
“Highlights of the Game!”
Mr. and Mrs. Michael Merriweather showing a little “Steeler Spirit in Pittsburgh Style”
Left: Jerome Bettis, AKA: “The Bus” Retired NFL Halfback-Los Angeles/St. Louis Rams and Pittsburgh Steelers
Left: Maurkice Pouncey #53, Current Lineman-Pittsburgh Steelers
Left: Hines Ward, Retired NFL’s Wide Receiver—Pittsburgh Steelers
Former Pittsburgh Steelers, Mike Merriweather and Jerome Bettis having a good time!
Right: Jerry Rice, Retired NFL’s Wide Receiver: S.F. 49ers, AFC Championship with Oakland Raiders, HOF.
A little action between Merriweather’s former team, “The Jets and San Francisco 49ers”
“Get Ready, Get Set, Let’s Go!”
“Bubba” Paris: Former NFL Offensive Lineman—San Francisco 49ers
Right: Marcus Allen, NFL’s Running Back and Football Analyst—Los Angeles Raiders, Kansas City Chiefs, 6 time Pro Bowler.
Right: Larry Fitzerald, Current Wide Receiver—Arizona Cardinals
“The Merriweathers enjoying their vacation”
Northern California Chapter NFL Alumni Helping Children Succeed!
…and they truly care for kids across the country!
The NFL Alumni ing football camps as they sign autographs,
and teach education along with life skills and ethics.
Merriweather teaching safety precautions, procedures and proper body mechanics
NFL Alumni working with children in sports individually while teaching skills and techniques.
“Teamwork is very important and everyone plays an important role.”
Left: Adrian Peterson, Current NFL Running Back—Minnesota Vikings Right: Michael Merriweather, Retired Linebacker—Pittsburgh Steelers and Minnesota Vikings v
ing the fans and charities by participating in Celebrity Basketball Players.
Celebrity Basketball Players
NFL Alumni with right: Mel Blount, Retired NFL Cornerback, NFL Defensive MVP, 5 time Pro Bowler, HOF
Middle: Hines Ward, Retired NFL’s Wide Receiver—Pittsburgh Steelers
Left: Jerome Bettis, Retired NFL Halfback—Los Angeles/St. Louis Rams and Pittsburgh Steeler with Mr. and Mrs. Michael Merriweather
My Cousins “Mookie” Jones, Charles Jones Former Wide Receiver—San Diego Chargers
Mr. and Mrs. Michael Merriweather
Left: Peja Stojakovic, Retired Professional Basketball Player—Sacramento Kings #16
Right: Ed “Too Tall” Jones, Retired NFL Player—Dallas Cowboys Defensive Lineman
Middle Back: Larry Fitzgerald, Current Wide Receiver—Arizona Cardinals
Right: Barry Sanders, Former NFL Running Back, HOF—Detroit Lions
….and some Steeler Wife Spirit!
Left: Billy “White Shoes” Johnson, Former Kickoff Returner—Houston Oilers Middle: Michael Merriweather, Former Linebacker—Pittsburgh Steelers, Minnesota Vikings, New York Jets and Green Bay New York Jets. Right: Erik McMillan, Former NFL Player—Philadelphia Eagles, NYJ, Cleveland Browns, Kansas City Chiefs.
I am blessed to be around people who enjoy giving and helping others. My contribution is to say, “Thank you Celebrity Ball Players and your families for all that you do and have done to our youth and those in need and may God forever bless you!”
…We are grateful to the Celebrity Players for working with our children, ing charities, sponsoring football camps, golf tournaments….
Left: Michael Merriweather Middle: “Mean Joe” Greene, Former NFL Defensive Tackle—Pittsburgh Steelers, HOF, 4x Superbowl Champion Right: Mel Blount
Michael and Coach Tomlin of the Pittsburgh Steelers
Left: Evander Holyfield (Boxer)
Left: Rob Woodson (Retired Cornerback and Safety—Pittsburgh Steelers, Baltimore Ravens, HOF
A Little Viking Spirit
Right: Larry Fitzgerald-WR for Arizona Cardinals. Left: Michael Merriweather
Left: Mike Ditka-Former NFL Player, TV Commentator and Coach for the Chicago Bears and New Orleans Saints totaling 13 years. Right: Michael Merriweather
Left: Donald Driver-Winner of Dancing with the Stars in 2012, Former NFL WR for the Green Bay Packers and Children’s Author. Right: Michael Merriweather)
Left: Drew Brees-Current New Orleans Saints Quarterback, selected to Pro Bowl 7x’s, NFL’s Comeback Player of the year in 2004… Right: Michael Merriweather
Left: Atiim Kiambu Hakeem-Ah (“Tiki” Barber)-Former NFL Runningback, NY Giants all-time rushing and reception leader post 2006 NFL post season… Right: Michael Merriweather
Right: Gary Weaver NFL Linebacker/Oakland Raiders
AutographsAutographs
School Nurses’ Knowledge on Assessments of Concussions and Head Injuries in Athletes
Sandra Merriweather
Copyright © 2013 by Sandra Merriweather.
Library of Congress Control Number: 2013900410 ISBN: Hardcover Softcover Ebook
978-1-4797-7630-6 978-1-4797-7629-0 978-1-4797-7631-3
All rights reserved. No part of this book may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner.
The author is unable to give advice or judgment when it comes to specific diseases and medical problems. It is necessary that one should seek medical council and attention from the services of a competent medical provider. It is not the intent of this book to diagnose medical problems, but every effort has been made to provide accurate scholarly information. The author and publisher will not be responsible for errors or omissions. Please seek the advice of your medical doctor.
To order additional copies of this book, : Xlibris Corporation 1-888-795-4274 www.Xlibris.com [email protected] 123827
Contents
List of Tables
List of Figures
Acknowledgments
Abstract
Chapter 1: Introduction to the Problem
Introduction
Problem Statement
Research Questions
Rationale and Significance of the Study
Definition of
Summary
Chapter 2: Literature Review
Introduction
Key Words
Review of Literature
Identified Problems
The Consequences
Chronic Traumatic Encephalopathy
Second Impact Syndrome
Post-Concussion Syndrome
Mild Traumatic Brain Injury (MTBI)
Traumatic Brain Injury (TBI)
Concussion
Postconcussive Symptoms
Role of the School Nurse
Education
Current Best Practices
Interventions for School Health
Nursing Assessment, Intervention, and Evaluation
Danger Signs of a Concussion
The Glasgow Coma Scale
Summary
Chapter 3: Methodology
Introduction
Research Design
Setting
Description of Participants
Description of Instruments
Data Collection and Analysis
Assumption and Limitations
Human Subjects Protection
Summary
Chapter 4: Findings
Overview
Analysis of Data
The Nurse Educator
The Cardiologist
Triangulation of Data
Results and Interpretation
Summary
Chapter 5: Discussion and Conclusions
Overview
Discussion
Nurses Current Knowledge
Additional Knowledge Needed
Implications
Limitations
Recommendations
Conclusions
Appendix A
Appendix B
Appendix C
Appendix D
Reference
Recommendation Blurps
Book Summary
Sandra’s Bio
List of Tables
Table 1: Danger Signs of a Concussion
Table 2: Number of Participant
Table 3: Age of the Participants
Table 4: Nurses’ Responses to Question 1
Table 5: Nurses’ Responses to Question 2
Table 6: Nurses Responses to Question 3
Table 7: Nurses’ Responses to Question 4
Table 8: Nurses’ Responses to Question 5
Table 9: Nurses’ Response to Question 6
List of Figures
Figure 1: Nurses’ Response to Question 5
Figure 2: Nurses’ Response to Question 5
DEDICATION TO OUR CELEBRITY SPORTS PLAYERS
This book would not be complete, If I would not give thanks to those celebrities that we meet. Not enough has been said, About foundations and legacy you have laid. To the current and former NFL, NBA, Soccer, Baseball, Hockey and Boxing Stars, Just know that you’re appreciated right here, right now, and from afar. The charity work that each of you so graciously perform is truly recognized; Beyond the physical sport and beyond the external human eye, And appreciated by all of your significant others and your lovely wives! As many of them have kept you focused time after time. Our love for you goes beyond mere co-existence; This is why we have so much love for you and patience. You are honored by your mentors, coaches, peers and fans, For standing tall, steadfast and being real men, Driven by adversity because what you exemplify comes from way deep within; Your gifts are many as demonstrated through the variety of talents from your hands. Sometimes not enough has been mentioned, not enough has been said.
About how you often give up your family time, To help those in need while contributing to the wellness of mankind Being a football wife and a relative of NFL players, I know what happens during and after “The Game,” You continue to love all your fans just the same! Participating in celebrity sports and sport events, football camps and golf tournaments! And not to mention all those pictures of present and past And all of those lovely autographs! Giving donations and raising money for charities, Continually looking for those who are without, ill and sick, most definitely! Thanks to you all for being who you are; Because you all will forever be our famous celebrity stars! We thank you for believing in research and education, We thank you for loving our future generation! And From all the sports wives across the entire world, We thank you for making us your girls!
Written by: Mrs. Sandra Merriweather
To All Nurses
Children are innocent; continue to treat their injuries with ion
And in a timely fashion
Often they have no voice
Because they are too young to make an adult choice
As nurses we advocate
Participate and mandate
In emergencies no time to contemplate, waiver, or hesitate
While grabbing our nursing bag
We realize there’s no time to lag
It’s our duty to have a substantial medical knowledge base
As they look to us with a solemn face
We must document, document, document
Noting times and, if necessary, call the ambulance
Knowing that you’re blessed while under stress
Their lives so many times are found within our hands
Responding to the scene as fast as we can
Lying there on school grounds
Your nursing assessment, just make it count!
Hats off to you, and thanks for all that you do
Helping parents and school districts protect children while in school
Written by Sandra R. Merriweather, RN, BSN, PHN, MSN
Acknowledgments
I would like to thank my husband, Michael Merriweather, retired NFL linebacker for the Pittsburgh Steelers, Minnesota Vikings, Jets, and Packers. I am thankful for his willingness to be patient while I embark upon something new and challenging. I am grateful for his encouragement and for the words “You’ve got to be tough and make another tackle” when I felt like I couldn’t go on. I am thanking Mike for his encouragement and for the love he has shown. I am truly thankful for WGU and for granting me the opportunity in a career I so love and cherish and for providing me with the best mentors: Dee Adkins and Cindy Watson. I would also like to thank Dee Adkins for brightening my day, for the words of encouragement, and for the listening ear. I am grateful for WGU for providing me with wonderful instructors: Dr. Vince Shrader, Dr. Pat McCarver, and Dr. Debra Dukes. I would like to thank my Capstone mentor, Dr. Tori Canillas-Dufau, for her expertise, longevity, and guidance during this entire project and for helping me to remain focused and consistent yet strong. I would also like to thank Dr. Timoteo Rico and Dr. Manshadi for added and for being a great friend to me and my family. I would like to also thank my children for their patience and understanding and to my only little granddaughter, Kasiyah Irene, for her beautiful smile that always brightens my day. I am also grateful to my very dear friends Carla Harris, LVN, and Kitty Taylor, RN, CNS, PhD(c) for their encouragement, advice, and wisdom. The words “Hang in there!” reminding me of the powering words voiced to me by my deceased mother, Irene Williams, and thanks to my sister, Dr. Rita Williams-Washington, and father, Pastor E. G. Williams, for their encouragement, prayers, and . I would also like to thank my beloved church family for remaining by my side in spirit and faith. Dear Mother,
To my dear mother whom I love and adore so very, very, much; Thank you for forever holding and touching my hands, Giving me direction and faith to know that, “I can” While impacting lives, helping children and helping man. You see, mother, I did pay close attention to the 41 foster and disabled Children whom you raised and gave so much love; I hope I can at least do one quarter of what you have done. You’ve nursed, clothed, guided, sheltered, comforted and fed those without; You’re greatly loved by all of us no doubt! Nor did you treat anyone of them different from your natural children; We were all treated the same; You have left me with beautiful memories and a legacy that I am not ashamed! You had this drive to reach others; You were just an exceptional mother! So, I found this one and only baby picture of you and me; What a wonderful team. Yielding our souls together, I believe; We have our legacy! Thanks for being an example of a Pastor’s Wife; It has led me to be attentive to other’s needs and to be present for changes occurring in lives.
Thanks for your many years of service to Marin General and Kaiser Hospital in Vallejo; You were a contribution to service that everyone knows. Thanks for giving me the desire to be a ed nurse; I love you so much that it can’t be explained with words. Thanks for yielding me to love children whole heartedly with unselfishness; And while I give service, “Do your very best!”
Love your daughter,
Sandra
The belated Mrs. Irene Alberty Williams and baby Sandra
Pastor E.G. Williams with wife, Irene
Abstract
The topic of concussion and associated head injuries in professional and collegiate athletes has been one of the most highly discussed subjects in sports. The recent deaths of retired NFL players associated with repeated head trauma has left communities and fans in disbelief. This topic has caused tremendous concern among medical professionals, sports officials, and families of the injured, and the media has taken it to another level because of the associated neurological, cognitive, and psychological effects that have the potential to affect the sports player later in life. Now, what has been overlooked is the problem of concussions, repeated concussions, head injuries, and its associated conditions and how it can affect the adolescent athlete. When a child becomes injured at school, there are those who attend to his/her needs. Those persons are coaches, trainers, school officials, and of course, medical professionals. In a school setting, when a child is injured, the school nurse is immediately called, and the coaches and trainers may also be the first persons on the scene. This study assessed the nurse’s current knowledge of head injuries in the adolescent athlete, and it gained additional knowledge that nurses feel they need to adequately assess and manage head injuries in athletic children. This study has revealed a need to incorporate new research findings of concussions/head injuries of young athletes into the school system as well as within the emergency rooms (ER) and trauma centers and suggests the application of concussion/head-injury scales, checklists, and guidelines to be used as a reference guide. The use of the Glasgow Coma Scale in the school systems has also been revealed as beneficial in recording the athlete’s conscious state prior to transfer to the ER. This study has also revealed the need for appropriate documentation to avoid future fatalities as in second impact syndrome and has assisted the public health arena in gaining additional nursing assessment knowledge.
Chapter 1
Introduction to the Problem
Introduction
Sport-related concussions have become an emergent problem within the collegiate and professional sports arena—as in the NFL, hockey, soccer, boxing, NBA, and other leagues—but a concussion can affect anyone and any age group. Age is most definitely not a factor. Concussions are known as a mild form of traumatic brain injury (MTBI) that happens from trauma to the head, and of course, children are prone to these types of injuries. Children who play sports have been known to continue playing in games with a known head injury because of not wanting to let their teammates or their coaches down, their eagerness to return to play, lack of knowledge of the results of continuing to play with an injury, and for many other reasons. There is a diversity of conditions that are associated with head trauma and its related , but the results are positively linked with cognitive impairment and mental development effects. Medical professionals, school officials, teachers, coaches, psychologists, and sport trainers are standing at a crossroad of preventions, solutions, and treatments because children as well as adults need solutions to this growing problem and the potential long-term effects. The resolution to part of this emergent problem will involve the entire educational team to have an individualized education plan (IEP) in place upon the return of the injured student. School nurses, both ed nurses and licensed vocational nurses, are the front-runners and the go-to persons in urgent medical situations that occur on school grounds. ed nurses are equipped with knowledge to teach parents and school staff about concussion safety, appropriate interventions, and implementation procedures upon returning to school post injury. Nurses are well educated and active participants in all health care settings that can set the tone for future generations to follow. It is extremely important for nurses to stay
current in knowing the signs and symptoms, to be aware of the risks of repeated head injuries, needed interventions, and treatment modalities in regards to concussions as this is becoming an important problem in the public health area. Current records suggests that concussions for 8.9 percent of all high school sports injuries and that females may be prone to higher rates of concussive injuries compared to male athletes participating in the same sports (Piebes, Gourley, Valovich-McLeod 2009; Gessel, Fields, Collins, Dick, and Comstock 2007). Research is also signifying that there may be enduring effects from a sport-related concussion that may impinge on the adolescent child’s physical and mental health, causing academic problems (McCrory, Meeuwisse, Johnston, Dvorak, Aubry, Malloy, and Cantu 2008). Due to these current studies, statements, and facts, it is imperative that all education personnel, school nurses, physicians, counselors, coaches, and athletic trainers collaborate to provide the best environment for the injured athletes. This Capstone Research Project has examined the current knowledge of school nurses’ assessment of head injuries in athletes as well as examined knowledge that the school nurses feel they need to provide the proper management and treatment. This research project has also discussed concussions along with its related , the signs and symptoms of a concussion, and the need for adequate recovery time, and it has identified conditions that can alter cognitive function and mental development. This research study has also discussed the possible effects of repeated concussions in athletes.
Problem Statement
It is a known fact that a history of repeated concussions can have damaging effects leading toward neurological, cognitive, and mental impairments as with some of our famous celebrity sports figures that have experienced permanent disabilities and, in some cases, have even died. Concussions/head trauma and injuries not only affect professional ball players but it can also have an effect in athletic children. There is now a growing public health need to promote safety, teaching, and interventions that will protect the immature brain. It is important that school nurses play an active role by first keeping current in new developments, treatments, and return-to-play guidelines and be advocates for the
children. Having a substantial amount of current information while promoting teaching to the families and collaborating with physicians, school personnel, coaches, trainers, et al., will provide a foundation and a plan that will be beneficial for the child upon returning to school after being injured. It’s going to take the whole village of professionals to get a grip on this growing problem.
Research Questions
1. What are school nurses’ current knowledge related to the assessment of head injuries in athletes? 2. What additional knowledge do school nurses believe they need to adequately assess and manage head injuries in athletes?
Rationale and Significance of the Study
Concussions and head injuries among the youth are becoming a fast-growing concern among medical professionals. This growing public health concern is challenging our nurses to be proactive, caring, advocates, teachers, and collaborators among peers, families, physicians, and coworkers. The time has come to upgrade our assessment skills from the standards of past time because of current medical research advancements and findings. Nurses must assist the child with care and treatment after sustaining a concussion. The child will need follow-up treatment and ongoing assessment while attending school. Therefore, working closely with other school officials and staff will provide an optimal environment during the healing process and will further aid in the recovery stage. Also, depending on the type and level of injury, the child may soon return to play per physician, but exactly how will the nurse assess this? The need for this study is great, and the problem to be addressed is so very real. With the school officials’ willingness to learn and cooperate with the nurses and physicians, the injured child will have the that will aid in recovery.
Definition of
The following were used in this study: Chronic Traumatic Encephalopathy (CTE): This is a neurological disorder associated with repeated concussions. This condition is associated with the presence of tau proteins in the brain. The effects are long lasting and may appear years later after having played in sports (Omalu, Dekosky, Hamilton, Minster, Kamboh, Shakir, and Wecht 2005; Omalu, Dekosky, Hamilton, Minster, Kamboh, Shakir, and Wecht, 2006). CTE is the term applied to chronic cognitive, intellectual, and neuropsychiatric symptoms of chronic neurodegeneration following a single episode of severe traumatic brain injury or (more commonly) repeated episodes of mild traumatic brain injury (MTBI). CTE represents the cumulative, long-term neurodegenerative consequences of repetitive concussive and subconcussive impacts to the head (Omalu, Fitzsimmons, Hammers, and Bailes 2010). Concussion: A concussion is a type of mild traumatic brain injury (MTBI) that occurs due to an impact or jolt to the head. The American Academy of Neurology clearly defines concussion as a “trauma-induced alteration in mental status that may or may not involve a loss of consciousness” (Kirkwood, Yeates, and Wilson 2006; Neurology 1997). Mild Traumatic Brain Injury: The traditional definition of mild has been a Glasgow Coma Score (GCS) of 13 to 15. The many words that have been used interchangeably are subtle, minor, minimal, or concussion and continually add to the confusion because of the snowball effect it has when a child has been subjected to recurring head trauma (Cook, Schweer, Shebesta, Harties, and Falcone 2006). Second Impact Syndrome: This is another type of head injury that has been determined as a fatal, overpowering increase in intracranial pressure (I) that occurs from swelling of the brain due to a previous blow to the head that had not recovered (Miele, Norwig, Bailes, 2006; Kelly and Rosenberg l997). Traumatic Brain Injury: A traumatic brain injury is a serious injury to the brain
from an outside force that can lead to lasting or momentary destruction of cognitive, mental, physical, and psychosocial disorders. There may also be an associated or diminished altered state of consciousness.
Summary
The school nurse plays an important role when children are injured on the school site and should be called immediately to attend to the emergent needs, as well as the athletic trainer and coaches, which are also first responders. While research knowledge continues to grow in the area of concussions in athletic children, so must the knowledge base in our nursing and medical curriculum while extending into the profession. As one can see, the injured child will require collaboration among medical professionals, school officials, s, teachers, and counselors due to problems associated with cumulative effects. We all must learn to listen, observe, and watch for signs and symptoms of impending threats to the health and well-being of our children. Why listen? We listen because a child’s pain grows silent when the eagerness to continue to play in the games outweighs sitting on the bench. We listen and observe because a child’s words need to be heard, but when they are silent, we must be advocates. Nurses are advocates who are well-trained licensed professionals that are equipped with an abundance of information, but as research expands, so must nurses’ knowledge. This research has examined school nurses’ current knowledge related to the assessment of head injuries in athletes. Staying current on the latest research in this area not only expands the nurses’ medical knowledge but also enables them to assess, implement, evaluate, and teach with the most up-to-date information. Chapter 2 has reviewed scholarly published literature that is of valuable importance in addressing the issue of concussions and head injuries, return-toplay guidelines, and signs and symptoms in the injured athlete.
Chapter 2
Literature Review
Introduction
The medical field and even the news media have really grasped the facts of the growing problems and the long-term effects that concussions have demonstrated in professional athletes. There have been a number of unfortunate, highly profiled deaths of NFL players that have gained the attention of the media, and now, finally, concussed children are drawing much-needed attention. Presently, attention to concussions in athletic children is beginning to take first-class seats. This literature review will explore evidence-based research previously conducted on the subject of concussions and head injuries in those persons that have played sports. The literature will review pertinent information that reveals signs and symptoms of not only concussions but also its associated conditions.
Key Words
Head injuries, head trauma, concussions, sport-related concussion and mild traumatic brain injuries (MTBI), multiple concussions, cerebral concussions, recurrent concussions, cognitive impairment, depression, sudden impact syndrome (SIS), mental impairment and mental disability, cumulative brain injury, postconcussive syndrome (PCS), chronic traumatic encephalopathy (CTE), school athletes, school nurses and management.
Review of Literature
Included in this research study, the literature also contains three articles. Two were written in1997. The article by Kelly and Rosenberg, both credible physicians, discussed the diagnosis and management of a sports’ concussion, which is also a key factor in this study. This article was chosen due to the limited literature of concussion studies in children. The second article included (Mittenberg, Wittner, and Miller 1997) recognized that post-concussion syndrome occurs in children, and it also discusses the need of nurses and others to be active in identifying the signs and symptoms in concussion. The article by the Virginia Brain Injury Lawyers discussed the death of an NFL player that suffered repeated head trauma. These three articles contain pertinent information.
Identified Problems
Concussions, head injuries, mild traumatic brain injury (MTBI), and sportrelated concussions appear to be one of the most popular and yet intriguing topics as they relate to professional athletes of the present and of the past. The interesting thing is that these are used interchangeably and contribute to the confusion of the topic at hand. There are also other conditions associated with head injuries such as post-concussion syndrome (PCS), second impact syndrome (SIS), and chronic traumatic encephalopathy (CTE), but what is common to each concussion term is the associated cognitive impairment and mental development effects.
The Consequences
These conditions can have long-lasting effects resulting in serious conditions
that affect the emotional well-being of the athlete. What seems to be an issue that has been downplayed, overlooked, and somewhat ignored is that a sport-related injury can happen to any person, as in our athletic youth not just in college or among professional athletes. One must keep in mind that a child’s brain is underdeveloped and that the head injuries sustained can increase the risks of further complications. These complications can result in progressive deterioration in social and cognitive function: loss of memory and memory disturbances, loss of executive functioning, paranoid ideations, exaggerated responses to life stressors, rampant fluctuations in mood, problems with intimate and family relationships, sleep disturbances, major depression, alcohol and/or drug abuse, violent behavior, increase interest in religion, body aches, pains and headaches, direct autopsy brain tissue with evidence of cerebral taupathy (Omalu, Hamilton, Kamboh, Dekosky, and Bailes 2010). There have been several studies on college and professional athletes regarding the effects of concussions but few revealing the effects of such on high school athletes even though many youth have died due to second impact syndrome (SIS). More research needs to be done in regards to the effects of concussions on age, immaturity, and developmental differences. Research studies have concluded that their data suggest that a history of repeated concussions may be a risk factor for late-life memory impairment, mild cognitive impairment (MCI), and Alzheimer’s disease (AD) (Guskiewicz, Marshall, Bailes, McCrea, Cantu, Randolph, and Jordan 2005; CDC 2011).
Chronic Traumatic Encephalopathy
Chronic traumatic encephalopathy (CTE) refers to persistent cognitive and neuropsychiatric symptoms of continual neurodegeneration following a single episode of severe TBI or recurring episodes of MTBI. CTE can only be definitely diagnosed by direct tissue examination (Omalu, Bailes, Hammer, and Fitzsimmons 2010). CTE has been previously termed as dementia pugilistica due to its association with boxing as initially described by Corsellis in l973 (Gavett, Stern, and McKee 2011). Dr. Bennet Omalu initially discovered physical evidence of concussions and
CTE in sports other than boxing. Dr. Bennet Omalu along with other founding (Julian E. Bailes, MD, and Atty. Robert P. Fitzsimmons) developed a new center called the Brain Injury Research Institute (BIRI) for the study and prevention of traumatic brain injuries. The institute has constituted a brain and tissue bank that contains 20 brains for future studies. It is the desire of the founders to develop appropriate treatment and intervention protocol for this disease as well as to ascertain genetic predisposition that will decrease progression and, hopefully one day, to provide a cure (Brain Injury Research Institute 2009). The long-term effects of concussions and head injuries are many, and something beneficial in the reduction of concussions must be done to protect children now and throughout their adulthood as several adolescent and college youth have been found to exhibit early signs of CTE. Chronic traumatic encephalopathy (CTE) must be taken seriously as this is not just a threat but also a word of warning to advancing destruction to the human brain and the centers that control certain operations. CTE can alter and threaten a sports player’s life no matter what age the person may be. CTE, in connection with pathologic changes, can alter memory and managerial functioning; behavioral and personality disturbances (apathy, depression, irritability, impulsiveness, and suicidality); Parkinsonism and irregularly; and motor neuron disease as seen in affected persons (Gavett et al. 2011). The diagnosis of CTE has not changed; it is diagnosed after death by examination of brain tissue. Yes, the problems attached to CTE can be fatal and/or long lasting, but the question is, how many lives will it take to truly grab the attention of children and head injuries while realizing that the adult professionals were also once children and played as children? Presently, there are no current neuropathological criteria that have been agreed upon for the diagnosing of CTE or large-scale, longitudinal clinicopathological correlation studies, and this makes the diagnosing of CTE difficult (Gavett et al. 2011). On February 17, 2011, a well-known NFL safety for the Chicago Bears committed suicide. He had a remarkable defense career playing football in 1985. Today this man is no longer with us because his symptoms resulted in his suicidal death. His behavior prior to his death exhibited a downward spiral in reasoning ability, erratic and violent behavior with signs and symptoms of
depression. He was discovered to have significant changes in personality and character (Virginia Brain Injury Lawyers 2011). This man, known as Dave Duerson, was only 50 years old, and after studies by Boston University physicians and the director of Neuropathology Care at Boston University’s Alzeimer’s Disease Center, it was confirmed that this man showed classic and moderately advanced symptoms of CTE (Needle and Ellenberg 2011).
Second Impact Syndrome
Another problem that is so unique to this topic—like that of NFL, NBA, hockey, soccer, boxing professionals, etc.—is that major injuries and death have occurred among this group, and it has occurred in athletic youth as well. It is especially important to treat head injuries, thus allowing time for adequate healing because a second blow or injury to the head without sufficient time to heal from the initial injury will lead to second impact syndrome (SIS), complications, and even death—a potential lethal combination. Second impact syndrome is another type of head injury that has been determined as a fatal, overpowering increase in intracranial pressure (I) that occurs from swelling of the brain due to a previous blow to the head that had not recovered (Miele, Norwig, and Bailes 2006; Kelly and Rosenberg l997). A second brain injury can lead to an increase in cellular death (Zink and McQuillan 2011). If a player continues to reenter games of sports with untreated head injuries, then the results can be CTE and its complications; this is why documentation of head injuries and adequate records are very crucial. There is much controversy surrounding the second impact syndrome due to lack of documentation of the first head injury, continued symptoms, and medical problems and the severity of the second impact (Miele et al. 2006; McCrory 2001). Again, early intervention from medical professionals with adequate documentation is necessary and crucial at the sidelines. The possibility of getting a concussion is now even more frightening. This new information has alerted the medical world to researching preventative treatments and, hopefully one day, a cure. Researching this area matters as it affects not only current and former NFL players but also all persons
in sports, from our youth to adults, friends and families, and persons we all love. Examining this area will alert all persons involved in sports, such as persons in the medical field, athletic trainers and coaches, referees, school officials, and others to take precautions in preventing head trauma/concussions. This information will also alert them to the signs and symptoms of the subject at hand, thus enhancing teaching, documentation, and observation skills.
Post-Concussion Syndrome
There are many postconcussive symptoms (PCS) that have been divided into three groups: somatic, emotional/behavioral, and cognitive. The symptoms of each of these three groups make the injured minor subjective to close observation at home and at school because of somatic disturbances (headaches, fatigue, nausea, vomiting, visual changes, tinnitus, dizziness, balance problems, and sensitivity to light and noise). There are also emotional and behavioral problems that can occur as a result of postconcussive symptoms (lowered frustration tolerance, irritability, increased emotionality, depression, anxiety, dizziness, and personality changes). The cognitive problems that can exist affects a child’s intellect (a slowed thinking or response speed, mental fogginess, poor concentration, distractibility, trouble with learning and memory, disorganization, and problem-solving difficulties) (Kirkwood 2006).
Mild Traumatic Brain Injury (MTBI)
Mild traumatic brain injury (MTBI) is a growing and an important public health problem. The traditional definition of mild has been a Glasgow Coma Score (GCS) of 13 to 15. The many words that have been used interchangeably are subtle, minor, minimal, or concussion and continually add to the confusion because of the snowball effect it has when a child has been subjected to recurring head trauma (Cook, Schweer, Shebesta, Harties, and Falcone 2006). MTBI can escalate into a more serious health care condition. The consequence
results in physical, cognitive and behavioral impairments, and serious disabilities, depending on the severity of the damage (Cook 2006; Piebes, Gourley, Velovich-MCleod 2009). There are many articles on children playing in the games of sports as well as the problems associated with concussions, and there are several youth who have died while playing in the games, but there is a great amount of room for further research in this area. An important point is to note that the literature concerning the epidemiology, treatment, diagnosis, prognosis, and costs of mild traumatic brain injury (MTBI) has been searched, and it has been clear on the fact that children’s prognosis after an MTBI is good with quick interventions and resolutions of symptoms (Carroll et al. 2004).
Traumatic Brain Injury (TBI)
An important public health concern is traumatic brain injury (TBI) because every year, it affects more than 1.7 million Americans (Guskiewicz 2005; CDC 2011). Fatalities of head injuries occur in 52,000 persons in the United States each year, but the majority of head injuries are determined to be TBI. A TBI is a nondegenerative and noncongenital hit to the head or an object that has caused piercing of the skull to the brain, possibly leading to permanent or temporary injury of cognitive, physical, and mental functions with an associated decreased or altered state of consciousness (Dawodu and Campagnolo 2011). It can result when the head suddenly hits an object or when an object penetrates the skull, entering the brain tissue. The amount of damage to the brain determines the severity of the condition. An estimated $60 billion is spent annually on brain injury treatment and rehabilitation (Bay 2011; Iavagnilia C, 2011). Severe sportrelated injuries of the head are many as there are several diagnoses, but a mild traumatic brain injury (MTBI) is a more common injury that causes difficulty in management. It becomes especially hard to manage when the decision of returning a player to the game is needed. With an epidural hematoma injury, a player can be initially stunned and appear to be doing well right after, but within the next 15-30 minutes, they may experience progressive neurological impairment. Observation and early recognition are essential during this period (Miele, Norwig, and Bailes 2006).
Traumatic brain injury has received limited national attention from various public agencies until recently. This condition has captured the attention of public policy makers, elected officials, and even among military officials. The is now readily available as research continues to formulate discoveries. What is needed and desired are policies, procedures, and of course, medical and nursing protocols for providing necessary treatments (Trudel, Scherer, and Elias 2011). Research findings have implicated consistent evidence that most children and adolescent children recuperate fully from a single straightforward MTBI. Prognosis has been determined well after MTBI (Kirkwood, Yeates, and Wilson 2006; Carroll, Cassidy, Peloso, Borg, Holst, Holm, Paniak, and Pepin 2004). It is, however, important that the healing process be allowed ample time to recover no matter how long it takes to reduce neurobehavioral problems, the same problems reported in adults (Kirkwood et al. 2006; Mittenberg, Wittner, and Miller l997).
Concussion
A concussion is a type of mild traumatic brain injury (MTBI) that occurs due to an impact or jolt to the head. The American Academy of Neurology clearly defines concussion as a “trauma-induced alteration in mental status that may or may not involve a loss of consciousness” (Kirkwood et al. 2006; Neurology 1997). Concussion is a functional, rather than a structural, injury that results from shear stress to brain tissue caused by rotational or angular forces. Many people believe that it is mandatory that the impact involves an injury directly to the head, but it does not. An impact can occur from other areas of the body. Initial assessment involves eliminating cervical spine injury and serious traumatic brain injury. The most common symptom of a concussion involves headaches, but symptoms can occur from other clinical domains (e.g., somatic, cognitive, affective). There is a range of assessment tools to assist with diagnosis, including symptoms checklists, neuropsychological and postural stability tests, and sideline assessment. Both cognitive and physical rest contributes to the initial management of this condition. There are no specific treatments for concussions.
The goal is to control symptoms and return the individual to play (Scorza, Raleigh, and O’Connor 2012). Children may need a longer recovery process due to the immature developed brain. Further study is needed in this area to determine the effects of impact on the immature brain. A concussion also disrupts cellular activity in the brain from functioning properly. Even though most individuals will recover wholly after a concussion, the signs and symptoms of this injury may last from several minutes to several months or even longer. Long-term effects from a concussion can alter thinking, memory, learning, language, and emotions (Samiento, Mitchko, Klein, and Wong 2010). There are many immediate signs and symptoms of a sport-related concussion, which are similar in younger and older athletes, as follows:
• A change in playing ability • A vacant stare • Fogginess • Confusion • Slowing • Memory disturbance • Loss of consciousness • Increased emotionality • Incoordination • Headache • Dizziness • Vomiting
It is highly recommended that a child who has suffered a single MTBI be allowed enough time to recover from the initial injury; if not, these children may encounter serious complications similar to the adult professional ball players as in a study performed on a professional football player that began organized football at age 18 and resulting in 14-year span of play (Omalu et al. 2006). Sportsmen that are subjected to recurring MTBI are also subjected to enduring neurodegenerative outcomes (Omalu et al. 2005).
Postconcussive Symptoms
The conditions that a child may now face will exhibit postconcussive symptoms (PCS) that are categorized into three different areas termed somatic, emotional/behavioral, and cognitive effects (Kirkwood et al. 2006). Even though children may respond to head injuries similar to that of the adult, there are some major differences. Some of the signs and symptoms of a serious concussion include the following:
• A headache that gets worse and will not go away • Muscular numbness and weakness including decreased coordination • Ongoing nausea and vomiting • Slurred speech patterns
New advancements have been made in protecting our youth participating in athletic activity for children between the ages of 11 and 18. As of January 2012, all coaches of any organized youth athletic activity will be required to take an online course for recognition of concussions (Castellanos and Oakes 2011).
Several key words were used to represent this research design and will be used to guide the information obtained. These key words are head injuries, head trauma, concussions, sport-related concussion, mild traumatic brain injuries (MTBI), multiple concussions, cerebral concussions, recurrent concussions, cognitive impairment, depression, sudden impact syndrome (SIS), mental impairment and mental disability, cumulative brain injury, postconcussive syndrome (PCS), chronic traumatic enceph4alopathy (CTE), school athletes, and school nurses.
Role of the School Nurse
The school nurse plays an important role when children are injured on the school site and should be called immediately to attend to the emergent needs along with the athletic trainer and coaches, which are also first responders. While research knowledge continues to grow in the area of concussions in athletic children, so must the knowledge base in our nursing and medical curriculum and within the profession. As one can see, the injured child will require collaboration among medical professionals, school officials, s, teachers, and counselors due to problems associated with cumulative effects. We all must learn to listen, observe, and watch for signs and symptoms of impending threats to the health and well-being of our children. Why listen? We listen because a child’s pain grows silent especially when they are eager and desire to continue to play in the games, and besides, in their eyesight, this outweighs sitting on the bench. We listen and observe closely because a child’s words need to be heard, and when they are quiet, we must be their voice while acting as advocates.
Education
The primary focus within this research design is to gain knowledge of what school nurses know about assessing head injuries in adolescent athletes. It is important for school nurses to gain current knowledge on how to assess and treat acute head injuries/concussions as it is common practice to notify nursing staff
of any impending emergencies or acute situation at the school site. The nurse is usually responsible for coordinating and managing quality care. Documentation is a must for future reference as well as a guide in managing second-impact injuries. Evaluation and recovery is essential for return-to-play guidelines. It is equally important for the nurse to collaborate with the family, physicians, school officials, trainers, coaches, and personnel as well so that the best education can be provided while the child is absent from school, returns to school half-day, and returns to school full time. The time of the healing process is varied and depends upon the type of injury and whether it is a second-impact injury. Most children who have sustained a sport concussion can recover fully with proper treatment. There are many reasons as one can see why the need is so great to provide the most current information for school nurses, officials, as well as the parents so that children can receive the most beneficial treatment toward the recovery process. Researching this area is necessary because the research in this area continues to make new discoveries, and as new information becomes available, it is also a necessity to alert and increase the knowledge of the school nurses as they are immediate responders. The results in this area will provide the researcher of which assessment areas need clarification, training, and/or more knowledge.
Current Best Practices
Head injuries and concussions occur on the school grounds more often than the media, medical personnel, school officials, and parents once believed due to the lack of knowledge by adults and the reluctance to report by children for fear of not being able to continue to play in the games. Now that there has been an increase in awareness of concussions, there are certain points that need clarity and addressing. School nurses play a very large role in the security of children while they are attending school, and it is necessary for the nurse to have a knowledge base that is current and accurate. Knowledge, assessment, and implementation of initial treatment are three components that the nurse must possess when responding to an injured child. Providing quality and effective care will promote the best
optimal level of well-being. Head injuries and concussions can no longer be considered as “just another bump on the head” as its long-term effects without treatment can be devastating, resulting in both cognitive and mental disabilities. Nursing management, collaboration with physicians along with other medical personnel professionals, school officials, coaches, trainers, and parents and psychologist will also equip the child with a good foundation to cope and begin the healing process. Nursing management should make sure that a head-injury protocol is in place at every school so that nurses will be knowledgeable of their duties and will be aware of designated responders during emergent situations (Pennington 2010). The CDC has taken a positive step in deg a tool kit for coaches of secondary school. It has information about concussions in youth. The CDC has also conducted a study to determine which items were helpful to the coaches in increasing their knowledge, practices, and prevention to safely manage sport concussions. The tool kit consists of facts about concussions and what to observe (Samiento, Mitchko, Klein, and Wong 2010).
Interventions for School Health
School professionals are extremely important and play a vital role in assisting a child’s return to school post concussion due to the need to limit activities during the recovery process. There are activities that can cause concussion symptoms to reemerge and degenerate; they include studying, working on the computer, and playing video games. These activities can lead to what is called cognitiveexertional effects (Samiento et al. 2010). Thinking and learning, which are both cognitive activities, must be monitored carefully to avoid this effect. It is extremely important for clinicians to be knowledgeable about the usual course of recovery and to recognize when recovery is not taking place as expected. Clinicians must be able to screen and seek out those persons appearing to have complications and those persons that are at the greatest risks for an optimal outcome (Carrol, Cassidy, Peloso, Borg, Hoist, Holm, Paniak, and Pepin 2004).
According to Samiento (2010), “Implications for School Health,” those children
returning to school must do the following:
• Take frequent rest breaks • Spend fewer hours at school • Be given extra time to take and complete assignments • Receive help with school work • Reduce time spent on the computer, reading, or writing
Students should not return to participate in recreational activities on the same day of injury unless cleared and evaluated by a health care professional that is experienced in the evaluation of concussions. A student must also show clearance of the injury from a medical professional stating that they are symptom-free, and they must not return to these following classes until medically cleared:
• Physical education (PE) class • Physical activity at recess • Sports practices or games
It is highly important and recommended that all school officials, medical personnel, coaches, parents, and students work in collaboration to benefit the child’s health and be aware for any of the following problems:
• Increased problems paying attention or concentrating
• Increased problems ing or learning new information • Longer time needed to complete tasks or assignments • Inappropriate or impulsive behavior during class • Greater irritability • Less able to cope with stress or is more emotional • Difficulty organizing tasks • Symptoms that get worse (headache, tiredness) when doing schoolwork
It becomes difficult for a child when he/she becomes injured because of the changes that occur with the physical, cognitive, and mental health. Their activities also become altered, and many times, they cannot comprehend the importance of resting, relaxing, and taking things slow. This is why it will take the entire teaming of professionals that are involved in the child’s care to give them the attention they so deserve. The team of school educators and school nurses will need to offer and encouragement to the saddened heart, to the child that feels discouraged, and to the child who has lost his/her concentration. Let’s not forget the child that feels frustrated with the sense of “I can’t go on.” Through collaboration and cooperation from the child’s team, the child will regain encouragement and a sense of self-worth with academic achievement.
Nursing Assessment, Intervention, and Evaluation
A concussion exists when the brain is jarred while in acceleration-deceleration, momentarily disturbing the functioning of the brain. There is no association between concussions having a visual structural abnormality on a CT scan. The management of concussions is geared by treating the symptoms. Experiencing headaches is one of the most frequent complaints.
Research by Zink and McQuillan (2011) and the CDC (2011) suggest that persons experiencing a concussion may exibit the following symptoms:
1. A period of unconsciousness 2. Unconsciousness lasting seconds to hours 3. Temporary loss of reflexes 4. Amnesia prior to and after the event 5. Headache or pressure in the head 6. Fatigue, feeling sluggish, hazy, foggy, or groggy 7. Dizziness or balance problems 8. Behavioral disorders 9. Double or blurry vision 10. Irritability 11. Memory problems 12. Difficulty concentrating and paying attention 13. Trouble sleeping and anxiety 14. Nausea or vomiting 15. Bothered by light or noise 16. Confusion
The above signs and symptoms may last for months post injury and is known as post-concussion syndrome (PCS). These symptoms do lessen, given time to
recuperate. Persons with concussions are usually seen in the emergency rooms but are usually discharged. It is up to clinicians to be educated and to document accordingly and especially when an injured child returns to school. Also, the need for accurate documentation of an initial injury will assist in providing pertinent information if a second impact occurs. Offering the assistance of groups and rehabilitation services will benefit the client. Advise the family of an injured child to refrain from activities that may lead to a repeat injury and to notify their physician of ongoing, persistent problems (Zink and McQuillan 2011). Keep in mind that treatment of concussions and head injuries vary depending on the injuries sustained. It will be necessary to follow the physician’s orders, making sure that the child seeks follow-up care, provide injury prevention information and other pertinent resources, and always be sure to obtain medical clearance from a physician prior to the child returning to play. Maintain good communication between school officials, coaches, trainers, parents, physicians, and medical professionals to return the child to an optimal level of function.
Danger Signs of a Concussion
The Centers for Disease Control and Prevention (CDC 2010) explains that, in rare cases, a blood clot may develop on the brain of a person with a concussion that crowds the brain against the skull. This is an emergent medical problem, and it is important to note danger signs and impending threats to a sports player’s well-being. A sports concussion is an injury that is blind to the eye but can be detrimental to the brain and to the quality of life. Concussions, therefore, should be managed carefully, and every injury, no matter how small or large, requires medical attention. Listed below is a danger sign chart developed by the Centers for Disease Control and Prevention (CDC 2010):
Table 1 Danger Signs of a Concussion
One pupil larger than the other Drowsy and unable to awaken A headache that does not go away but worsens Weakness, numbness, or decreased coordination Repeated vomiting or nausea Slurred speech Convulsions or seizures Cannot recognize people or places Becomes increasingly confused, restless, or agitated Has unusual behavior Loses consciousness (a brief loss of consciousness should be taken seriously)
The Glasgow Coma Scale
The Glasgow Coma Scale (GCS) has been used as a method to record level of consciousness in comatose patients and predominately used in hospitals. The GCS is not readily used with the very young child due to his/her inability to communicate well. There is a pediatric version similar to the adult version. The GCS can be used in the older child to assess eye-opening verbal and motor responses according to precise grading scales. Pediatric brain injuries are classified by severity using the same grading scales as adults and can determine long-term impairments. The GCS can be used as a prehospital predictor of outcome (Gabbe, Camaron, and Finch 2003).
Summary
This area of focus has extremely limited current research conducted in the area of prolonged effects of concussions on youth athletes although the problem has been identified, and this has caused the researcher to include areas of research conducted on adult athletes. There is more room for further research studies and the possibilities of teaching new knowledge of sport-related concussions in children because they suffer injuries like everyone else. This topic even appears to have more interest in male athletes, but a research study has determined that there are even sex differences in concussion symptoms of high school athletes. After a sport-related concussion, male and female high school athletes presented different types of symptoms. Males stated they had more cognitive problems whereas the girls complained of more neurobehavioral and somatic symptoms (Frommer, Gurka, Cross, Ingersoll, Comstock, and Saliba, 2011). As one can see, gender is now an issue of interest. There are many questions that arise concerning sport-related concussion/head injuries in athletic adolescent children as this topic needs continual interest. The literature review s the findings that concussions occur in athletic children as well as with professional athletes and that there are signs and
symptoms as well as potential prolonged effects (presently being investigated) that medical staff should be aware of, as the injured child may not discuss when they are injured because of the desire to continue to play in sport games as well as not wanting to let their teammates and coaches down. One important fact that everyone should keep in mind is that the professional and collegiate sports players that are now presenting with cognitive, psychological, and mental disabilities began playing sports as children. It is clear that school nurses need to be aware of all signs and symptoms of concussions and head injuries because medical research is discovering new findings.
Chapter 3
Methodology
Introduction
Chapter 3 describes the methodology and the research design for this study. The goal has been to address and answer the two following research questions:
1. What are school nurses’ current knowledge related to the assessment of head injuries in athletic children? 2. What additional knowledge do school nurses believe they need to adequately assess and manage head injuries in athletes?
Research Design
This research design used a qualitative approach that applied triangulation by way of questionnaires (one that was designed for the school nurses and one especially designed for the nurse educator/advanced practice nurse) and a structured interview with a cardiologist in California that addressed second impact and its relationship to head injury. The interview provided more in-depth information of data on second impact syndrome and revealed the importance of documenting every head injury as documentation provides medical clinicians and professionals with accurate information needed for future management of care. The researcher used a recording device to tape the interview, and the data
were immediately transcribed and stored in a secured safe along with the questionnaires in a locked room. In order to assess nurses’ knowledge, the data from the school nurses’ nonrandom questionnaire were categorized with summation of findings into narrative form. The key idea in this study was to identify common group items and key information with common factors into clusters of the same issues while applying a sincere understanding of what has occurred with the data received (Gay, Mills, and Airasian 2009).
Setting
This research has taken place within the state of California, located centrally and east of the San Francisco Bay Area. There are a total of three participating school district nurses that included licensed vocational nurses (LVNs) and ed nurses (RNs). The number of participating school nurses totaled 40 participants. Included in this study are a nurse educator and a physician that have provided information and expert advice of this research subject.
Description of Participants
The LVNs and RNs from ages 24-67 were of interest. Their experience within the nursing field is varied, ranging from 1 year to 44 years practicing. The total number of RNs participating within the 3 school districts total 34 RNs, and the total number of participating LVNs is 6. These nurses are school nurses possessing a variety of nationalities, varied educational backgrounds with the majority being RNs, and they are employees of one of three participating school districts. The role of the school nurse within these school districts is to provide school health services, promote health education, and coordinate health care. The researcher chose to include LVNs in the study as well as RNs because often they also respond to the urgent needs of the children and provide treatment. One interesting fact that most definitely is a requirement for the success of satisfying
the goals within this particular study is the collaboration of everyone involved with the care of children. The nurses have a personal interest to provide the best care possible and to collaborate with other school officials, counselors, and instructors on the medical needs of the students. The present problems that are arising in the topics of concussion/head injuries are presenting new as well as much needed information, and this is getting the attention of everyone; therefore, medical professionals need to be updated with the most current facts, treatment, and interventions. Current knowledge on the topic of head injuries and concussions among the student athlete in many school districts has not yet been addressed although the nurses have had previous schooling and knowledge of the assessment and treatment of head injuries in general. The nurses as well as school officials find this topic extremely interesting being that the media has shed new light on the current additional problems associated with head injuries as a result of discoveries by physicians and other medical professionals; even physicians find this topic challenging and fascinating. The number of participating nurses suggests their eagerness and willingness to participate and learn new treatment interventions and modalities. The school nurses within this research design work closely together among their peers and among school officials. This demographic region provides a healthy environment for the sake of children as the location is within the central valley versus being in a fastpaced city promoting a tranquil environment. Questionnaires and a personal interview have been conducted confidentially, and approval has been given per three separate school districts. The ethnic composition of the nurses is varied, and the surveys were open to any nurse who wished to participate within the specific age group stated. with a physician and a nurse educator was made as needed for clarifications on medical findings, to provide input and suggestions in the area of assessing head injuries in athletic children.
Description of Instruments
The researcher was the primary source as well as the primary instrument that collected pertinent data. The role of the researcher was to analyze, interpret, and categorize information from the questionnaires while utilizing common schemes
and patterns. The gathering of data from the interview, questionnaires, including all entries and notes, were interpreted to determine the meaning of the records and facts to the best ability of the researcher. Discovering the meaning of the outcome of data after examination and comparing previous data to the most recent data were also tasks of the researcher. The researcher continued to build upon new discoveries while trying to make logic of the data as a whole thus incorporating coding and categorizing skills. The data were tapered down and placed into less significant groups. The key idea in this study was to identify information with common factors while applying a sincere understanding of what had occurred with the data received. One of the instruments used to store and collect qualitative data was a Microsoft ® Tableau Spreadsheet. The function of the Microsoft ® Tableau Spreadsheet is to simplify information by formatting data into computerized tables by way of rows and columns. This method is able to demonstrate relationships in a simplified way. To further strengthen this study, the researcher utilized the ATLAS.ti ® software, which analyzes qualitative data using multiwindow frames while providing an overview of the findings. This feature is known to provide while working. This is a software program that was ed to clarify and substantiate the findings of this research project.
Data Collection and Analysis
The data-collection methods chosen for my project were a qualitative research design utilizing triangulation techniques to gather information regarding “School nurses’ current knowledge related to the assessment of head injuries in athletes” and “What additional knowledge do school nurses need to adequately assess and manage head injuries in athletes?” Data collection began in April 2012. Participants were instructed not to include identifiable data on the questionnaires. The researcher de-identified all personal data that were received on the questionnaires. Data received were identified by groups, and the information was transferred to the Microsoft ® Tableau Spreadsheets that showed relationships as it also simplified the data. The spreadsheet contains
different themes that arose from 40 responded RNs and LVNs. The three datacollection methods consisted of a questionnaire distribution among each participating school nurse, a questionnaire that was given to a nurse educator, and an interview/questionnaire with a cardiologist for discoveries of a hit or blow to the chest causing a second impact. The interview with the cardiologist was audiotape-recorded by the researcher and subsequently transcribed. The transcription was given to the cardiologist for review for further detail as needed. This procedure provided both clarity and accuracy. The cardiologist addressed three questions in regard to second impact syndrome and its relationship to cerebral injury, additional knowledge he felt would be beneficial to nurses in managing head trauma, as well as additional knowledge that he believes nurses needed to adequately document a second impact. These in-depth responses will increase pertinent knowledge and current practice guidelines for nurses and medical professionals in detecting and treating sports concussions and head injuries in children. The questionnaire for the nurse educator addressed current practice guidelines and additional knowledge that would benefit nurses in managing head injuries in young athletes within the emergency room and trauma units. The purpose of choosing this data-collection method was to provide comprehensive content as well as reveal a definite connection between the severely injured athlete and interventions of school nursing that continues into the ER and trauma centers. It will provide readers with content voiced directly from those treating children with concussions and head injuries and gain knowledge and insight of this newly and highly discussed growing problem in the area of public health nursing. A prearranged time was set to meet with the nurse educator to address the specific set of questions. The data obtained from the qualitative method by way of triangulation were then coded for recurring themes. The information was then explored for understanding and meaning within the data. Coding identified ideas, and this allowed grouping of the information into various categories. All data has been explored to promote clarity, ideas, and interpretation that have been received from the data within. Questionnaires and personal interviews have been conducted confidentially with consent from the school nurses, both licensed LVNs, RNs, and the nurse educator. The questionnaires for the nurses (RNs and LVNs) consisted of six open-ended questions that addressed issues within this research design that has
addressed what the nurses know about assessing head injuries in athletic children. Included within the questionnaire are four demographic questions that addressed the nurses’ type of licensure (RN or LVN), age, and number of years practicing as a licensed nurse. was also received about the use of the Glascow Coma Scale (GCS), which is a method to record the level of consciousness that is predominately used in the hospital system; the researcher has obtained consent per each school district’s research process prior to the implementation of this research project. After obtaining consent from each school district, the researcher met with nursing management to set up specific times to meet with the nurses and distribute the individual questionnaires. The participants were informed that their participation in this study was strictly voluntary and that all information collected is confidential. They were also told that their submissions are confidential, and they were advised not to write their names on the forms. The participants were well-informed that they will not be reprimanded, dismissed, discriminated against, or retaliated against for participating in this study. The participants were told that this research does not involve any risks, harm, or costs. The participants were aware that participation in this research project was at their free will thus providing informed consent. The participants were also given information for additional questions. The school districts strongly suggested that the time set for distributing questionnaires must not interfere and conflict with the times in which a nurse must be readily available for the management of providing health care to the children. It was most appropriate for this study to be conducted just prior to nurses’ meetings. This researcher distributed the questionnaires prior to nurses’ meetings at the specified times agreed upon with nursing management in each school district. The information received from both the nurse educator and the cardiologist was compared to the data received from the 40 respondent school nurses. The purpose of choosing this data-collection method was to provide comprehensive content. It provides readers with content voiced directly from those treating children with concussions and head injuries while gaining knowledge and insight of this newly and highly discussed growing problem in the area of public health nursing. The data collected were reviewed and have been put in a narrative form, yielding narrative data, common characteristics, common patterns, and themes.
Differences in responses have been noted, and the discoveries and findings have been summarized. The questionnaire for the nurse educator and the interview with the cardiologist is in narrative form.
Assumption and Limitations
The researcher has observed through this investigational study a need to update nurses’ current knowledge base on the problems associated with concussions and head trauma mainly due to the recent and current concerns of concussion/head trauma awareness in sports. What is equally important is to provide nurses with the information they feel will assist them with current assessments, interventions, and practices. This problem is worldwide, and current medical information is needed as research in this area continues to make new advancements. Nurses, both LVNs and RNs, must remain knowledgeable to reflect the current best practices due to the newly increase of concussion awareness.
Human Subjects Protection
The researcher has completed online training with the National Institute of Health and has received certification in Protecting Human Research Participants (see appendix D). The researcher has also taken several collaborative courses at Western Governors University, including instruction on values and ethics, all leading toward this potential research project. Consents to conduct research among three individual school districts has been obtained and forwarded to the chairperson. Participants have been told not to disclose their names, and identifiable markings have been removed. The data collected do not reveal any participant identifiable data, and it is stored in a secured combination safe that is known only to the researcher. Confidentiality will continue to be maintained. The safe itself is also secured in a locked room in which the researcher has possession of the key. The collected analyzed data is stored in a secured safe, and later, it will be destroyed upon permission by Western Governors University.
The participants have been informed that they have the right to participate or withdraw at any given time and that there are no potential risks or costs involved in this study; informed consent is not needed.
Summary
This qualitative research design utilizing triangulation identified pertinent data and assessed current nurses’ knowledge related to the assessment of head injuries in athletic children, and it gained knowledge on what the school nurses believe they need to adequately assess and manage head injuries in athletic children. Not only did this study seek nurses’ knowledge but it also gained knowledge from medical experts that assisted nurses to remain current on pertinent information that will benefit the health of the athletic child while promoting growth, knowledge, and collaboration in the public schools and in the public health arena. Chapter 4 presents the finding of this research study.
Chapter 4
Findings
Overview
After consent was given from each participating school district, a questionnaire that was developed by the researcher was distributed among three different school districts within the region of the San Francisco Bay Area in California. The questionnaire gathered demographic data and information about the nurses’ current knowledge in the assessment of head trauma in young athletes. Once this vital information had been collected and obtained from all three school districts, graphical analysis was used as a means to interpret the data by categorical organization (Gay et al. 2009).
Analysis of Data
The results from the nurses’ questionnaire were interpreted by the Microsoft ® Tableau and the ATLAS.ti ® software and then placed into figures 1 and 2 included in tables 2-9. The initial data from the spreadsheets included values of 1, which represented that the respondents mentioned it—any blank fields reflected that no comments/statements were made or observed. Concepts of nausea and vomiting and signs and symptoms were combined as one group. The total number of participants in the study was 40, which included 36 ed nurses (RNs) and 4 licensed vocational nurses (LVNs). The ages of the nurses ranged from 24 to 67, and a total of 5 nurses chose not to make an
entry in this category. The minimum age was 24 while the mean age was 52. The median age was 55, and the maximum age was 67. The minimum year of practice was 1 year with a mean practice of 24.22 years. The median number of years practice was 26 with a maximum number of years totaling 44. Table 2 summarizes the two types of nurses represented in this study, the total number of RNs, the total number of LVNs, and the sum of all nurses participating in this study. The total number of RNs that participated in this study was 36, and the total number of participating LVNs was 4. While there was 100% participation among the LVNs employed in the three school districts, they represented 10% of the participants in this study. There was also 100% participation among the RNs, and they represented 90% of the total participants in this study (see table 2).
Table 2: Number of Participants
ed Nurses (RNs) Licensed Vocational Nurses (LVNs) Total Number of Nurses 36
4
40
Table 3 represents how the participants responded to the age category in the questionnaire. The participants that voluntarily participated completed an informed consent form that included confidentiality, risks involved, agreement, researcher’s , and demographics that included licensure, age, and years practicing (see appendix A). Table 3 summarizes the minimum, mean, median, and maximum age of the participants.
Table 3: Age of the Participants
Minimum Age Mean Age
Median Age
Maximum Age
24
55
67
52
Table 4 represents the responded signs and symptoms (S/Sxs) of assessment mentioned by the nurses including the number and percentage of nurses that mentioned each symptom. The following responses were given in response to question 1: “What is the current practice for nurses assessing head injuries in children?” Table 4 demonstrates that 30% of the nurses would check the trauma site, and 22.5% would assess for changes in vision, and 35% would assess pupil size. The other assessments the nurses felt needed attention are listed in table 4 as well but shows an increase in what they felt is current practice in assessing head injuries in children.
Table 4: Nurses’ Responses to Question 1
Current Practice in Assessing Neurologi- cal Checks Observa- tion Check Trauma Site # of Nurse Responses 25 28 12 % of Nurse Responses 62.5 % 70.0% 30.0%
Table 5 represents the knowledge of the signs and symptoms (S/Sxs) the nurses would observe in the course of an acute concussion. The low value of percentages is in the areas of assessing for blurred vision, drowsiness, and pupil size, and their responses were 40%, 62.5%, 30%, and 27.5%, respectively. The highest responses stated by the nurses in observing for signs of an acute concussion were to observe for headaches and changes in level of consciousness (LOC) in which both ed for 70% of the responses. Observing for nausea was included at 65% of the responses by the nurses. Table 5 demonstrates their responses to question 2: “What are the signs and symptoms (S/Sxs) of an acute concussion?”
Table 5: Nurses’ Responses to Question 2
Nurses Reported S/Sxs
Blurred Vision Dizziness Drowsiness Headaches
# of Nurses Reported S/Sxs 16
25
12
28
% of Nurses Reported S/Sxs 40.0%
62.5%
30.0%
70.0%
Table 6 illustrates the results of question 3: “What signs should be observed in children with acute head injuries?” The nurses responded that they would assess for blurred vision in a child with an acute head injury at 32.5% and included drowsiness as part of the assessment ing for 45% of all responses. Assessing for blurred vision and drowsiness ed for less than half of the responses by the nurses. The nurses stated they would also observe for signs of dizziness and headaches in which both responses ed for over 50%. Observing for headaches received the highest percentage area mentioned for assessing children with an acute head injury as evidenced by 57.5% of the respondents.
Table 6: Nurses Responses to Question 3
Nurses Reported S/Sxs
Blurred Vision Dizziness Drowsiness Headache
# of S/Sxs Reported by Nurses 13
20
18
23
% of S/Sxs Reported by Nurses 32.5%
50.0%
45.0%
57.5%
Table 7 represents the nurses’ responses to question 4. There are several responses with low values in every area mentioned except assessing for headaches, which ed for 70% of the nurses’ responses. In table 7, the majority (70%) of the nurses reported that athletes will report headaches as a primary sign of a concussion/head injury while reports of dizziness, LOC, nausea, and pupil size ed for less than 40% of responses by the nurses. Table 7 includes the areas the nurses mentioned that they would assess for in regards to question 4: “What signs are usually reported by athletes with concussions/head injuries?” Their responses are as follows:
Table 7: Nurses’ Responses to Question 4
Nurses Reported S/Sxs
Drowsiness Headache LOC
Nausea Pupil Size
# of Nurses that Reported the S/Sxs 3
28
14
13
2
% of Nurses that Reported the S/Sxs 7.5%
70.0%
35.0% 32.5% 5.0%
Table 8 represents the responses from question 5: “When should athletes be cleared to return to play after receiving a concussion? Table 8 reveals that 75% of the nurses believed that an athlete should be able to return to play in the games post sustaining a concussion after the athlete has been seen and cleared by a physician. The responses demonstrate that 30 out of 40 nurses believed that an athlete’s clearance should be granted upon clearance from the medical doctor. Three nurses chose not to respond to this question while 7.5% of other nurses felt that an athlete can return to games of play when symptoms subside. There were 2.5% of nursing respondents that stated an athlete should be cleared post injury within several weeks while 2.5% stated within 15 minutes. Another 2.5% reported the athlete can return to play post assessment while another 2.5% reported an athlete should be cleared post injury in about 15 minutes.
Table 8: Nurses’ Responses to Question 5
Nurses’ Responses
Within several weeks After MD visit Within 15 min
# of Nurses Response to Each Category 1
30
1
Figure 1 and figure 2 clearly demonstrate the results of question 5. The majority of nurses (75%) believed that an athlete must be cleared by a physician before returning to the games post concussion/head injury. There were 7.5% of the participants that did not respond to this question. Figure 1 and 2 are additional figures and views that reveal how the nurses have responded to this question. These figures were adapted from the Microsoft ® Tableau software for qualitative data analysis.
Figure 1: Nurses’ Response to Question 5
Figure 2 is a bar graph that s the findings of question 5 and demonstrates the results in a different view and suggests that 75% of all nurses that participated in this study believed that an injured athlete’s clearance for returning to play is most definitely in the hands of the physician.
Figure 2: Nurses’ Response to Question 5
Table 9 represents the nurses’ responses to question 6: “Is the Glasgow Coma Scale utilized in the assessment of head injuries in children?” The answers varied in responses significantly, with 25% stating the GCS is not used in their school district, another 25% revealing yes, the GCS is used in their school district. Five percent of the participants chose not to answer while another 5% stated that they do not know if the GCS is used, and 7% stated the GCS is used in a modified version. Another 7% believed the GCS is to be utilized in the ER setting. There were 12.5% of nurses that stated the GCS is not used in a school setting and 7% stating the GCS is not utilized in the assessment of head injuries in children. Interestingly, 2% commented, “Why not?” Please see table 9.
Table 9: Nurses’ Response to Question 6
Nurse Responses to the Usage of the GCS in School Setting No Response Not in school sett The # of Reported Responses in Each Subdivision
2
5
The Nurse Educator
In addition to the six questions addressed to the three school district nurses, two additional questions were addressed to a nurse educator that is a professor currently practicing and teaching nursing students at the university level within the San Francisco Bay Area. The nurse educator has 30 years of experience as a nurse and has provided additional insight in the topic of head injuries in athletic children. Please see question 1 and question 2.
Question 1:
1. “What additional knowledge do you feel nurses need to adequately assess and manage head injuries in athletic children?”
Nurse Educator’s Response to Question 1:
The nurse educator stressed the importance that “Nurses need knowledge of actual and/or potential complications that result from repetitive sports injuries in children. Nurses also need knowledge of how head injuries in children sustained from sports differ from head injuries in adults sustained from sports.”
Question 2:
2. “What is the current practice and guidelines for assessing and evaluating acute concussions/head injuries in athletic children within the ER and trauma centers?”
Nurse Educator’s Response to Question 2:
“It has been discovered that in a major medical facility and its hospitals, there are no current practice and/or guidelines that exist for assessing and evaluating concussions/head injuries sustained from sports in children within the ER and trauma centers. The standards of practice include treating and monitoring the care of the patient with increased intracranial pressure.”
The Cardiologist
The following research questions address the same three specific interview questions asked of the cardiologist who is a well-qualified author, surgeon, and consultant for an NBA team. The cardiologist is board certified in internal medicine, cardiology, and advanced clinical training and education thus qualified to provide medical expertise.
Interview Question 1:
“What is second impact syndrome, and how does a blow to the chest affect a cerebral injury?”
Cardiologist Response to Question 1:
“Second impact syndrome [SIS] is a process whereby a second trauma to the brain soon after the first concussion can lead to a rapid and catastrophic brain
injury and death. The second trauma does not need to be a head trauma. It could happen with even a hard chest injury, which can in return propagate a shock wave to the head.”
Question 2:
“What additional knowledge do you feel nurses need to adequately assess and manage head trauma/concussions?”
Cardiologist Response to Question 2:
“The public and the nurses should be aware of patients showing up to the ER with head trauma post concussion and get a good history and note if this was a first or a second concussion, especially in teenagers. A second concussion should be evaluated for neurological deficits ASAP and given the proper management.”
Question 3:
“What additional knowledge do you feel nurses need to assess a second impact injury, and how would this relate to documentation?”
Cardiologist Response to Question 3:
“Additional factors that nurses should be aware of are the need for an immediate response if you detect a second head trauma injury. The more one delays, the
worse the outcome. On the exam, do a thorough evaluation of pupil reflexes and note any signs of confusion. More importantly, make sure that the athlete does not return to athletic activities for at least 6 weeks.”
Triangulation of Data
The findings of low percentage values in the assessment of visual changes in concussions or head injuries (see tables 4, 5, 6, and 7) the need for further education and also the cardiologist’s urge for nurses to include and incorporate visual assessment in the assessment of children with head injuries. The evaluation of headaches when an individual has sustained a concussion is one of the significant and accurate findings as represented by the nurses responding at 70%. Experiencing headaches is one of the most frequent complaints (Castellanos and Oakes 2011; Kirkwood et al. 2006; Zink and McQuillan 2011). The literature review also s the nurses’ percentage of 75% as well as s the cardiologist in that a child should not be allowed to return to game of play until he has been cleared by the physician. It is the goal of this qualitative triangulation study to educate medical professionals as well as encourage them to stay current in the areas of sports-related concussions and head injuries because the effects, if not treated, can be fatal. Triangulation in this study also reveals to be accurate and provide exceptional documentation as voiced by the cardiologist and verified in the literature review. A comprehensive literature review has been completed on the topic of head injuries and concussions. The usage of the Glasgow Coma Scale in the school setting has been ed by the literature review as needed, and it can be used as a prehospital tool evaluating the conscious state of a person (Gabbe et al. 2003). The literature review assesses the need for promoting safety to athletes, education, and health care maintenance. The questionnaires were completed by the participants with their consents and revealed their willingness to be proactive in the school setting in which they are so committed.
Results and Interpretation
The first four questions on the questionnaire that was distributed to the school nurses have similar types of observation that are required in the assessment of head injuries, and it is important to know that concussion and head trauma are used interchangeably as research continues. Table 4 in this study demonstrates that 30% of the nurses would check the trauma site, and only 22.5% would assess for changes in vision, and 35% would assess pupil size. The other assessments the nurses felt needed attention are listed in table 4 as well but shows an increase in what they felt is current practice in assessing head injuries in children. Recent data state the importance of assessing for a variety of neurological and cognitive problems including alterations in vision (Zink and McQuillan 2011). Table 5 illustrates the s/sxs the nurses would assess in an acute concussion. There were several signs mentioned, but 40% mentioned blurred vision, 30% said drowsiness, and 27% stated pupil size out of 40 respondents. According to the nurses’ responses for question 1, their answers reflect observation, neurological, and trauma checks. Observation would be changes in behavior, neuro, which is self-explanatory, and trauma checks being physical but visual around the site of impact. According to the percentages, there is a clear shift between the three areas even though the responses from questions 2-4 have common . The percentages from questions 2-4 have common theme . The difference in percentage from each theme for each question varies although the type of injury is the same (with different degree of severity); there is clear evidence of inconsistent treatment. In other words, practitioners who treat concussed children may not necessarily know what they are looking for as this area as a new research is presently ongoing with new discoveries. Question 4, however, addresses “What signs are usually reported by athletes with concussions and head injuries?” The areas mentioned by the nurses varied in small percentages, but 70% of the nurses revealed the need to assess subjective statements of headaches. According to the questionnaire from the nurse educator, there are no guidelines in place for children with head injuries in the ER and trauma rooms in some hospitals. In question 5, table 8 demonstrates that 75% of nurses believe a child should not be cleared to play post concussion until cleared by a physician. The usage of the Glasgow Coma Scale had a variety of responses. Table 9 represents the nurses’ responses to question 6: “Is the Glasgow Coma Scale utilized in the assessment of head injuries in children?” The answers varied in responses significantly, with 25% stating the GCS is not used in their school district; another 25% revealing, yes, the GCS is used; and 3 participants stating the GCS usage in a modified version. All other entries of
assessment are listed in table 9. The GCS has been found to be a tool used as a hospital precursor in the evaluation of the conscious state of a person (Gabbe et al. 2003). There were several findings in this study. The nurse educator discovered that there were no significant guidelines in the ER and trauma center at a major hospital and all its hospitals for the treatment of sports-related head injuries in children. The guidelines in place are for any persons presenting with increased intracranial pressure. The nurse educator proposed that the guidelines for children with concussions should be different than head injuries sustained from other causes. The nurse educator felt that nurses would benefit from additional knowledge provided in the areas of actual or potential complications that result from repetitive sports injuries in children. Additional knowledge needed would be how head injuries in children sustained from sports differ from head injuries in adults sustained from sports. The cardiologist interview suggests that the public and the nurses should be aware of patients showing up to the ER with head trauma post concussion and get a good history and note if this was a first or second concussion, especially in teenagers. The cardiologist was clearly stating that a second concussion should be evaluated for a neurological deficit as soon as possible (ASAP) and to give the proper treatment and management. The cardiologist also discussed second impact syndrome (SIS) and the need for immediate response and good documentation. It is important to know that the more delays, the worse the outcome. The cardiologist suggests an exam doing a thorough evaluation of the pupil reflexes and observing for any signs and symptoms of confusion. More importantly, make sure that the athlete does not return to athletic activities, which depends on severity, and at least six weeks.
Summary
This study examined demographic data that included the participants’ type of nursing licensure, their age, and their number of years practicing as a nurse. The questionnaire was designed to observe school nurses’ current knowledge and to identify what nurses feel they need to adequately assess head injuries in athletes. The results were based on the nurses’ responses to assessment questions with the identification of different themes, values, and responses. Certain concepts were combined and comparisons were made to the interview of a cardiologist that
provided knowledge necessary for nurses to adequately assess children with head injuries. Comparison was also made to a nurse educator’s questionnaire that provided areas of needed research and what knowledge nurses need to adequately assess head injuries in children. The purpose of this study was to assess school nurses’ current knowledge related to the assessment of concussions and head injuries in athletes as well as to obtain additional knowledge that nurses feel they need to adequately assess head injuries in athletes. The participants, along with their consents, revealed their willingness to be proactive in the school setting in which they are so committed. The data collection and analysis utilized in this study provided both tables and figures as measures to demonstrate responses from school nurses of multiple school districts. The information obtained will encourage education of head injuries and concussions in the public schools and public health arena as well as encourage new information into the ER and trauma centers. Additional information from this study will increase education among families, caregivers, and school officials. Further education is needed due to several inconsistencies in responses by the participants, especially since research in this area is ongoing and consistently making new advances, which is greatly needed and appreciated. Chapter 5 will present and discuss the implications, limitations, recommendations, and conclusions of this study in relation to its findings.
Chapter 5
Discussion and Conclusions
Overview
This final chapter discusses the findings, implications, and limitations of this study as interpreted by the researcher. Additional inclusions within this study will be suggestions and recommendations that will enhance assessment skills among those who treat persons with head injuries based on the results of this study and will be finalized in the conclusion.
Discussion
The research questions addressed in this study will be discussed individually and listed as follows:
1. What are school nurses’ current knowledge related to the assessment of head injuries in athletic children? 2. What additional knowledge do school nurses believe they need to adequately assess and manage head injuries in athletes?
Nurses Current Knowledge
This study did discover that most of the school nurse respondents recognized that the medical doctor is the key person to determine full recovery of an athlete that has suffered a concussion/head injury regardless of type. The physician, the ATC (certified athletic trainer), and other medical professionals work together to restore the athlete to preinjury status (Guskiewicz et al. 2004). This study has also identified three types of checks as mentioned by the nurses that they would observe for when assessing children with head injuries. The majority checks identified by the participants are neurological (neuro), observation, and trauma. Neurological checks are self-explanatory and observation checks, resulting in observing for changes in behavior while trauma is physical but visual damage around the region of impact. According to the percentages in the way the nurses responded, there is a definite clear shift between the three checks identified. It would seem that all medical practitioners would have mentioned these areas of assessment for head injuries regardless of training. It is important to note that initial assessment involves eliminating cervical spine injury and serious traumatic brain injury and that the most common symptoms of a concussion involve headaches (Scorza, Raleigh, and O’Connor 2012). In several questions regarding the signs and symptoms, observation and signs and symptoms reported by athletes, the majority of nurses recognized that assessing for headaches is a key assessment.
Additional Knowledge Needed
This study discovered that the response questions from 2-4 have common theme . The difference on percentage from each theme for each question varies although the type of injury is the same (with different degree of severity). There is clear evidence of inconsistent treatment, which may mean that practitioners may not necessarily know what they should be looking and observing for, as head injuries are of different degrees of severity, and the are presently used interchangeably while research in this area is continually advancing. Exposure may play a key role as those nurses and other practitioners that are more likely exposed are those more likely to assess the type of impact, regardless of the years of practice and age of the practitioner.
The use of the Glasgow Coma Scale has been used mostly in the hospital setting although its use in the school districts further creates ambiguity on what needs to be done. The responses from the nurses varied significantly in regards to the GCS’s usage in the school setting and suggest a need for knowledge in this area. Research has suggested that this tool would be beneficial (Gabbe et al. 2003). This is very interesting and opens the door to its usage as a hospital precursor within the school setting to record the conscious state of a person thus depending upon the severity of the injury. Yes, it is very important to know an athlete’s conscious state upon injury, but it is also important to know an athlete’s baseline neurological and cognitive status prior to games of play. Research has identified the necessity of obtaining neurocognitive, mental status, and postural stability (balance) tests prior to injury to serve as baseline data that can be compared to test results post injury. Therefore, knowing both the athlete’s preinjury status and postinjury status is beneficial for the athlete’s total well-being. There should also be a symptom scale or checklist in place (Guskiewicz et al. 2004; McCrory et al. 2009; Piebes et al. 2009). This additional knowledge will help nurses to manage and assess key factors in the identification of head injuries in athletes. The application of a symptom scale, checklist, and guidelines specific to concussions and head injuries in children will also serve as a reference guide and will further assist nurses in identifying key areas of assessment in injured athletes. This study discovered that assessing for problems with vision and pupil reflexes as suggested by the cardiologist was not a key assessment area with the nurses as identified by the low percentage rate of responses. Assessing for visual changes in head injuries has been a key factor in this study and throughout other research studies of this nature and is suggestive that all medical practitioners regardless of education should include this area of assessment. In this study, the nurses identified areas of assessment in the athletic child with a concussion/head injury and identified areas of self-reported symptoms by athletes. The responses from the nurses in regards to self-reported symptoms lacked several key assessment components that have been identified through previous research (Guskiewicz et al. 2004; Zink et al. 20011). Even though the nurses’ responses varied significantly, the total responses recorded were to assess the trauma site, check pupil size, check for blurred vision, headaches, drowsiness, dizziness, level of consciousness, nausea, and vomiting. Guskiewicz (2004) and Zink (2011) have identified the following areas to observe in both concussions and self-reported symptoms:
1. Assess cervical spine and cranial nerves recording the time of initial injury 2. Changes in level of consciousness (LOC) 3. Alterations in memory and concentration 4. Self-reported symptoms (headache, ringing in the ears, nausea/vomiting, feeling in a fog, problems sleeping, fatigue, drowsiness, sensitivity to light or noise, loss of balance, unsteadiness, double vision) 5. Check for alterations in vision 6. Balance problems 7. Check vital signs (v/s) and LOC every 5 minutes post concussion 8. Check for presence of amnesia
Scorza (2012) identifies that an initial assessment of a concussion involves the following:
1. Eliminating cervical spine injury and serious traumatic brain injury 2. Observing for signs and symptoms of a headache
The medical examiner in this study suggests assessing the following areas in second impact syndrome:
1. Do a thorough evaluation of the pupil reflexes. 2. Get a good history, noting if a second impact has occurred.
3. Check for neurological deficits as soon as possible (ASAP). 4. Do thorough documentation, recognizing this is an immediate response needing immediate attention by a physician.
An athlete can only return to full participation in the games once cleared by the medical physician or a trained expert in the field of concussion as long as there are no recurrent signs and symptoms present (Guskiewicz et al. 2004). This study has discovered that there is a major hospital along with all its d hospitals that do not have a guideline in effect for the treatment of children and athletic children with concussions and head injuries specifically. Without specific guidelines in place, certain areas of assessment will no doubt get missed, and the injuries occurring from a second impact without initial documentation, assessment, and the appropriate intervention can be fatal. This study has revealed that continuous education and training is critical, and the utility of the GCS is a good framework and tool for nurses to use in the school setting to further assist the emergency staff of a client’s initial conscious state and/or deterioration upon injury.
Implications
As a result of this study, several implications have been identified. The first implication would be that the most current knowledge of assessing, treating, and managing athletes with head injuries/concussions must be provided to school nurses and those who are involved in the care of the injured athlete by nursing supervisors and s. The second implication would be for nursing supervisors and nursing s to remain current with additional knowledge as new research progresses. The third implication would be for nursing supervisors and other staff to assist and provide concussion and head-injury awareness among school personnel,
coaches, athletic trainers, school s, parents, and all who are involved in the care of the injured athlete. The fourth implication would be for hospital s and supervisors to increase concussion awareness among the ER and trauma centers and implement guidelines specific to concussion/head injuries in children. These guidelines should be different than those for injuries sustained from other causes. The fifth implication would be for those persons involved in the individualized plan of care (IPC) of the athlete to incorporate the most updated information regarding current treatment modalities of concussions /head injuries in place upon the athlete’s return to school. The final implication would be for nursing supervisors and s to include the use of the Glasgow Coma Scale (GCS) into the policy and procedures for use in emergent situations. The GCS should be implemented in the school districts.
Limitations
This study did not take into consideration the length of time needed to incorporate three school districts along with the restrictions beyond the researcher’s control. The restrictions were necessary as this project was workable but around each school districts request to maintain their normal schedule upon each districts individual curriculum to avoid interruptions of the daily routines of the children, which is necessary. This was beyond the researcher’s control; however, it was the researcher’s choice to include three school districts versus one school district to increase the validity of the findings by going beyond the standard realm. The researcher views the findings of this study useful in incorporating a new area within the school system while increasing knowledge, assessment, needed interventions, and growth among not only school nurses but among all medical professionals and those persons involved in the plan of care with an injured athlete.
Recommendations
Based on the findings of this study, the following recommendations are made:
1. To provide the most current and up-to-date facts of assessment and treatment modalities surrounding head injuries and concussions of athletes to the school nurses by way of literature, fact sheets, current research studies, and in-services thus reviewing the school districts policies and procedures noting changes 2. For nursing supervisors, s, and those who are in leadership positions to remain current with new research findings specific to head injuries in athletes and incorporate new information into policies and procedures 3. To promote concussion awareness to school officials, coaches, athletic trainers, school staff, and parents through literature, fact sheets, and providing resources that are specific to each profession. Coaches and ATCs (certified athletic trainers) have specific new requirements and guidelines pertinent to their profession and should follow accordingly. Parents need to be provided with resources and information as well on what to look for in their child who has suffered a head injury and how to manage the athlete child in the home 4. To create concussion and head trauma guidelines, policies, and procedures within the emergency room (ER) and trauma centers specifically for injured athletic adolescent children by nursing s acting as patient and political advocates influencing decisions and actions 5. To have a concussion/head-injury guideline in place for the injured child upon the return to the school environment as part of the IEP (individualized education program) 6. To have nursing supervisors, s, educators, and public health include usage of the Glascow Coma Scale (GCS) into the policy and procedures
Conclusions
The findings of this research study s that there is a need to incorporate new research findings of concussions and head injuries into the school system. The information within this research design and the data discovered should be used to encourage knowledge among nurses, other medical professionals, coaches, certified athletic trainers (ATCs), school officials, instructors, and parents. The data should be used by nurses to enhance their assessment and observation skills to return the injured child to his/her preinjury status. The data should promote concussion and head-injury awareness by assisting medical professionals to remain current in treatment interventions and modalities, encourage supervisors and nurse educators to remain current in new research findings. The data should also encourage nursing supervisors to include guidelines of concussion and head injuries in the IEP (individualized education plan) and have it enforced upon the return of the athlete into the school environment. The data discovered suggests that nurse supervisors and educator include the Glasgow Coma Scale as a tool and hospital precursor to determine the conscious state of the injured for the ER and trauma centers. It is imperative that nurse educators study and address new research findings while taking into consideration that research in this area is ongoing. Nursing supervisors, public health nurses, and nurse educators must increase knowledge in this area of study by providing the community and nurses with facts, guidelines, continuous education, training, information, and referrals, thus encouraging nursing staff to provide the most optimal care in the concussed athlete. The data should be used to increase competency, confidence, and satisfaction of care within the nurses themselves while demonstrating their effectiveness in a job so rewarding.
Appendix A
Your participation in this study is voluntary and all information will be confidential. Entries and submissions are confidential. You will not be retaliated against, reprimanded, or dismissed for your participation, and there are no risks or costs involved. If you agree to participate in this study, it will be acknowledged by completing this questionnaire. Your input will provide information of your knowledge of assessment in athletes with head injuries and will provide knowledge to further assist children with brain trauma. Should you have any questions concerning this questionnaire, please Sandra Merriweather, RN, BSN, PHN, MSN, student at Western Governors University.
*Please do not write your name on this form.
ed Nurse _________ or Licensed Vocational Nurse _________
*Please check one of the above
Your age: ____
Number of years practicing nursing: ____
1. What is the current practice for nurses assessing head injuries in children?
2. What are the signs and symptoms of an acute concussion?
3. What signs should be observed in children with acute head injuries? 4. What signs are usually reported by athletes with concussions/head injuries?
5. When should athletes be cleared to return to play after receiving a concussion?
6. Is the Glasgow Coma Scale utilized in the assessment of head injuries of children?
Appendix B
Your participation in this study is voluntary and all information will be confidential. Entries and submissions are confidential. You will not be retaliated against, reprimanded, or dismissed for your participation. There are no risks and no costs involved. If you agree to participate in this study, it will be acknowledged by completing this questionnaire. Your input will provide information of your knowledge of assessment in athletes with head injuries and will provide knowledge to further assist children with brain trauma. Should you have any questions concerning this questionnaire, please Sandra Merriweather, RN, BSN, PHN, MSN, candidate at Western Governors University.
*Please do not write your name on this form.
Nurse Educator _________ or Advanced Practiced Nurse _________
*Please check one of the above
Your age: ____
Number of years practicing nursing: ____
1. What additional knowledge do you feel nurses need to adequately assess and manage head injuries in athletic children?
2. What is the current practice and guidelines for assessing and evaluating acute concussions/head injuries in athletic children within the ER and trauma centers?
Appendix C
Your participation in this study is voluntary and all information will be confidential. Entries and submissions are confidential unless otherwise stated by entry checked below. You will not be retaliated against, reprimanded, or dismissed for your participation and there are no risks or costs involved. If you agree to participate in this study, it will be acknowledged by completing this questionnaire. Your input will provide information of your knowledge of assessment in athletes with head injuries and will provide knowledge to further assist children with brain trauma. Should you have any questions concerning this questionnaire, please Sandra Merriweather, RN, BSN, PHN, MSN, candidate at Western Governors University.
Physician: Yes/No (circle) and Physician Specialty:
______________________________________
*Please check one of the above
Your age: ____
Number of years practicing: ____
Do you agree to discuss findings of researcher’s study if requested?
YES or NO (please circle)
1. What is second impact syndrome, and how does a blow to the chest affect a cerebral injury?
2. What additional knowledge do you feel nurses need to adequately assess and manage head trauma/concussions?
3. What additional knowledge do you feel nurses would need to assess a secondimpact injury, and how would this relate to documentation?
Appendix D
Reference
Bay, E. (2011). Mild traumatic brain injury: a Midwest survey about the assessment and documentation practices of emergency department nurses. Advanced Emergency Nursing Journal, 33, 1, 71-83. Carroll L. J., Cassidy J. D., Peloso P. M., et al. (2004). Prognosis for mild traumatic brain Injury. Results of the Who Collaborating Centre Task Force on mild traumatic brain injury. Journal of Rehabilitation Med, 43, 84-105. Castellanos, S., Oakes, C. (2011). Jantz hopeful for lasting legacy to grow from tragedy. The Aurora Sentinel, 4, 7. Centers for Disease Control and Prevention. Sport-related injuries among high school athletes-United States, 2005-2006 school year. MMWR Morb Wkly Rep. 55, 38: 1037-1040. Centers for Disease Control and Prevention. (2011). Heads Up: concussion in high school sports-fact sheet for athletes. http://www.cdc.gov/concusiion/pdf/AthletesFact_Sheet_a.pdf. Cook R. S., Schweer, L., Shebesta K. F., et al. (2006). Mild traumatic brain injury in children: Just another bump on the head? Journal of Trauma Nursing, 13, 2, 58-65. Frommer L. J., Gurka K. K., Cross K. M., et al. (2011). Sex differences in concussion symptoms of high school athletes. Journal of Athletic Training, 46, 1, 76-84. doi: 10.4085/1062-6050-46.1.76. Gabbe B. J., Cameron P. A., Finch C. (2003). The status of the glascow coma scale. Emergency Medicine, 15, 353-360. Gavett B. E., Stem R. A., McKee A. C. (2011). Chronic traumatic encephalopathy: a potential late effect of sport-related and subconcussive head trauma. Clin Sports Med., 1, 30, 1, 179-188.
Gay L. R., Mills G. E., Airasian P. (2009). Educational research: competencies for analysis and applications. Upper Saddle River, New Jersey: Pearson Education, Inc. Gessel L. M., Fields S. K., Collins C. L., Dick R. W., Comstock R. D. (2007). Concussion among United States high school and collegiate athletes. Journal of Athletic Training, 42, 495-503. Guskiewicz K. M., Bruce S. L., Cantu R. C., Ferrara M. S., Kelly J. P., McCrea M., et al. (2004). National Athletic Trainers’ Association Position Statement: Management of sport-related concussion. Journal of Athletic Training, 39, 280297. Guskiewicz K. M., Marshall S. W., Bailes J., et al. (2005). Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery, 57, 4, 719-26. doi: 10.1227/01.NEU.0000175725.75780.DD. http://www.wikipedia.org/ http://www.nflevolution.com/—Safety for your kids Kelly J. P., Rosenberg J. H. (1997). Diagnosis and management of concussion in sports. Neurology 48, 575-580. Kirkwood M. W., Yeates K. O., Wilson P. E. (2006). Pediatric sport-related concussion: A review of the clinical management of an oft-neglected population. Pediatrics, 117, 1359. Iavagnilio C. (2011). Traumatic brain injury: Improving the patient’s outcome demands timely and accurate diagnosis. Journal of Legal Nurse Consulting 22, 3, 3-10. McCrory P., Meeuwisse W., Johnston K., Dvorak J, et al. (2008). Consensus Statement on concussion in sport-the 3rd international conference on concussion in sport held in Zunich November 2008. Journal of Science and Medicine in Sport, 12, 340-351. Miele V. J., Norwig J. A., Bailes J. E. (2006). Sideline and ringside evaluation for brain and spinal injuries. Neurosurgery Focus, 21.
Mittenberg W., Wittner M. S., Miller L. J. (1997). Post concussion syndrome occurs in children. Neuropsychology, 11, 447-452. Moser R. S., Shatz P., Barry D. (2005). Prolonged effects of concussion in youth athletes. Neurosurgery, 57(2), 300-306. Needle & Ellenberg, P. A. (2011). Football player who killed himself did have serious brain injury. Brain Injuries, May 3, 2011. Omalu B. I., Fitzsimmons R. P., Hammers J., Bailes J., (2010). Chronic traumatic encephalopathy in a professional American wrestler. Journal of Forensic Nursing, 130-136. doi: 10.1111/j.1939-3938.2010.01078x. Omaulu B. I, Bailes J. E., Fitzsimmons R. P., Hammers J. L., et al. (2010). Chronic traumatic encephalopathy, suicides and parasuicides in professional American athletes. Am Forensic Med Pathology, 31, 2, 130-132. Omalu B. I., DeKosky S. T., Hamilton R. L., et al. (2005). Chronic traumatic Encephalopathy in a national football league player. Neurosurgery, 57, 1, 12834. Omalu B. I., Dekosky S. T., Hamilton R. L., et. al. (2006). Chronic traumatic encephalopathy in a national football league player: part II. Neurosurgery 59, 5, 1086-92. Omalu B. I., Hamilton, et al. (2010). Chronic traumatic encephalopathy (CTE) in a national football league player: Case report and emerging medical questions. Forensic Nurse, 6, 1, 40-6. doi:10.1111/j.1939-3938.2009.01064.x. Omalu B. I., Hamilton R. L., Kamboh M. I., Dekosky S. T., Bailes J. (2010). Chronic traumatic encephalopathy (CTE) in a national football league player: Case report and emerging medicolegal practice questions. Journal of Forensic Nursing, 40-46. Pennington N. (2010). Head injuries in children. The Journal of School Nursing, 26,1, 26-32. Piebes S. K., Gourley M., Valovich MCleod T. C. (2009). Caring for studentathletes following a concussion. The Journal of School Nursing, 25, 270. doi: 10.1177/1059840509339782.
Sarmiento K., Mitchko J., Klein C., Wong S. (2010). Evaluation of the centers for disease control and prevention’s concussion initiative for high school coaches: “Heads up concussion in High School Sports.” J School Health, 80, 112-118. Scorza K. A., Raleigh M. F., O’Connor F. G, (2012). Current concepts in concussion: evaluation and management. Am Family Physician, 82, 2, 123-32. Trudel T., Tina M., Scherer M., Elias E. (2011). Understanding traumatic brain injury: An introduction. Exceptional Parent, 41, 7, 33-7. Virginia Brain Injury Lawyers (2011). Duerson suicide due to repeated traumatic brain injuries. Brain Injury Law Center, 6, 11. Retrieved from: //http://www.brain-injury-law-center.com/2011/06/11/duerson-suicide-due-torepeated-traumatic-brain-injuries/. www.cdc.gov/concussion/headsup/high_school.htm Zink E. K., McQuillan K. (2005). Managing traumatic brain injury. Nursing 35, 9, 36-44. Retrieved from http://www.nursing2005.com/.
Recommendation Blurps
“This is an excellent and worth while project. I thought the two research questions posed are q
“Many professional football players sustain concussions that can result in long-term damage o
“. . . you are obviously ionate about this medical condition and the need to educate medic
“Unbelievable, unbelievable! What a great purpose and overlooked issue. You’ve explained ev
“This is a fascinating research study that reveals far reaching and serious implications for our
Sandra Merriweather has wrapped her arms around our children and has told significant facts
Book Summary
This research study book was designed not only to increase concussion and head injury awareness, but for the researcher to do something about it that would be creative and unique to the medical field, trainers, coaches, school personnel, officials and families. It was necessary to include school nurses as they are always called to the scene of injury along with the coaches and trainers in a school setting and mostly, they are advocates for children and adults alike in any environment surrounding health issues. The results of this study revealed pertinent information that needs further intervention to increase medical knowledge in various areas of health treatment. This book can be used as a quick reference guide for assessing the athletic child with a head injury but as in all emergency cases, seek medical attention as time and documentation are key factors. The ion for this area of study involves being safe and attentive to the signs and symptoms of head injuries. It is necessary to encourage families of children to continue practicing safety measures (Resources: www.nflevolution.com—Safety for your kids; www.cdc.gov/concussion/headsup/high_school.htm.), to be active and healthy while participating in sports and to exercise regularly in avoidance of injuries and sedentary lifestyles, other medical conditions and obesity. It is important to be educated on current facts, while observing, listening and learning from coaches and trainers in the correct training procedures and aspects of a game to be the best one can be. Be knowledgeable and seek information from our current and former athletes. We are all in this together. If any of you have a dream to play in a professional sport or know someone who does, focus on academics, obtain good grades in school, play by the rules, be observant, eat healthy, obtain plenty of rest listen to your trainers and coaches and just maybe we all will see you in the games we all so love!
Sandra’s Bio
Sandra Merriweather is the wife of Former Linebacker Michael Merriweather for the Pittsburgh Steelers, Minnesota Vikings, Jets and Packers. Even though they have a busy lifestyle, Sandra believes in finding time to service communities. She is a member of Off the Field Player’s Wives Assoc., SBNA Nurses Assoc., and she is a member of the CSNO (CA School Nurse Organization) and the NASN (Natl’ Assoc. for School Nurses), Calif. State Sherriff’s Assoc. and the NAA/ Los Angeles Chapter. She is also a ed nurse whose medical career began at age 15. It was during this time that she decided to become a “Candy Striper” and senior volunteer at Kaiser Permenente Hospital in Vallejo, CA while attending Hogan Senior High School. Upon completion of High School she received her AS degree and graduated from Bay City College as a Respiratory Therapist and EKG Technician and became so interested in the medical field that she decided to continue her education in nursing and psychology. Sandra has obtained multiple degrees and certifications in a wide range of medical professions that demonstrates her interest in promoting health awareness. She also attended Dominican University in San Rafael, CA. Sandra received her LVN (Licensed Vocational Nurse) license as well as her BSN degree in nursing. As both a LVN and RN (ed Nurse), she serviced major hospitals in the San Francisco Bay Area and San Joaquin County area through nursing registries and hospital employment. She received her MSN (Masters’ of Science) degree from Western Govenors University with a Specialty in Nursing Education and Research. The hospitals serviced by Sandra were St. Lukes Hospital, Mt. Zion Hospital, UCSF Medical Center of San Francisco, CA., St. Joseph’s Hospital in San Joaquin County and Seton Medical Center in Daly City, CA. where her specialty was in Neurology, outpatient clinics and pediatric services for many years. She has also worked for California Forensic Medical Group servicing Sonoma, Napa, Solano, Yolo and Stanislaus County Sherriff’s Departments attending to both adults and children in the Juvenile System. Her enthusiasm, dedication and charisma to provide positive effective care has led to contracted positions within California’s State Facilities as well. Sandra has also been employed for St. Joseph’s Hospital in the Rapid Care Center and currently holds PHN (Public Health Nurse) Certification. She is presently employed with Lodi Unified School District as a School Nurse/ School
Mental Health Nurse Educator servicing many schools and attending to the wellbeing of childrens’ mental and medical health. Sandra’s comion for both children and adult health care services came from assisting her parents raise 41 foster siblings and helping her parents in their Care Home and Williams Preschool and Kiddie Kare Facility in American Canyon, CA. Her drive is ambition, her talent is varied, her ion is endless and her desire is to promote positive health care is everlasting and most definitely a dream come true.
Mr. and Mrs. Michael Merriweather and Kevin Johnson (Former NBA Basketball Player for the Cleveland Cavaliers and Phoenix Suns; Mayor of Sacramento, CA.
Michael Merriweather with Ray Lewis (Current NFL Player with Baltimore Ravens)
Far Left: Evander Holyfield (Former Undisputed World Champion for both Cruiserweight and Heavyweight.
Sandra Merriweather with Hines Ward (Former NFL’s Wide Receiver of the Pittsburgh Steelers)
Far Left: Dwayne Woodruff (Former Pittsburgh Steelers) Middle: Calvin Sweeney (Former Pittsburgh Steelers) Far Right: Michael Merriweather (Former Pittsburgh Steelers, Minnesota Vikings)
Left: Dwayne Woodruff (Former Pittsburgh Steelers and Common Pleas Court Judge) Middle: Mayor Luke Ravenstahl of Pittsburgh Pennsylvania Right: Michael Merriweather (Former Pittsburgh Steeler and Minnesota Vikings
Far left: John Madden (Former NFL Player, highly Succesful Coach and Sports Announcer) Far Right: Michael Merriweather (Former NFL Player with wife Sandra.
Left: Michael Merriweather (Former Pittsburgh Steelers, Minnesota Vikings, Jets, Packers) Middle: “Bubba” Paris (Former San Francisco 49ers) Right: Jeff Barnes (Former Oakland Raiders)
Left: Kevin Geene (Retired NFL Linebacker and Outside Linebackers Coach for the Green Bay Packers; Los Angeles Rams, Pittsburgh Steelers, & Carolina Panthers Linebacker) 2nd Left: Dennis “Dirt” Winston (Former NFL Linebacker-Pittsburgh Steelers) Middle: Craig Bingham (Former NFL Linebacker-Pittsburgh Steelers/Oakland Raiders) Right: Robin Cole (Retired NFL Linebacker and Pro Bowler-Pittsburgh Steelers; Owner of Robin Cole’s Unforgettable Sweets in Pittsburgh, PA 2nd Right: Michael Merriweather (Retired NFL Linebacker, 3 time Pro Bowler, Steelers MVP-Pittsburgh Steelers, Minnesota Vikings, Jets and Packers)
Right: Ray Lewis Current NFL Player and Linebacker for the Baltimore Ravens; selected to 13 Pro Bowls; Superbowl XLV11
Mrs. Merriweather with NFL current players John Jacoby and Darrius HeywardBey/Oakland Raiders.
Far Right: Nesby Glascow, Former NFL Safety—Baltimore Ravens, Indianapolis Colts, Seattle Seahawks
Right: Rocky Bleier Retired NFL Halfback/Pittsburgh Steelers—Played in the first four Steelers Super Bowl Victories.
Left: Terry Bradshaw Retired NFL Player, TV Host, Actor and Author—Pittsburgh Steelers, MVP and NFL Player of the Year, Quarterback of the Steelers.
“Tony the Tiger” Lopez Boxer.
Michael Merriweather and the Terrible Towel
Left: Brent Jones (Former NFL Player for the SF 49ers) Right: Michael Merriweather—Pittsburgh Steelers, Minnesota Vikings…
Left: Chris Webber (Retired NBA Player)
The Merriweathers enjoying vacationing.
Jerome Bettis (Retired NFL Player/LA Rams and Pittsburgh Steelers)
Left: Michael Merriweather and Midback—Eric Wright with Dave Casper (Tight End Hall of Famer—Oakland Raiders)
Right: Vlade Divac (Retired Yugoslav and Serbian Professional Basketball player, NBA Player and Hall of the Famer—Los Angeles Lakers, Charlotte Hornets and Sacramento Kings.
Mrs. Sandra Merriweather and Fred Biletnikoff (Former NFL wide receiver, coach, and Hall of Famer.
Mr. and Mrs. Michael Merriweather at Mel Blount’s ALL-STAR Celebrity Roast
Left: Calvin Sweeney (Former NFL Wide Receiver—Pittsburgh Steelers) 2nd Left: Louis Lipps with wife (Retired NFL Wide Receiver—Pittsburgh Steelers and New Orleans Saints. MVP Steelers 1985 Right: Mr. and Mrs. Michael Merriweather.
Middle: Dennis Rodman (Retired NBA Player and Hall of Famer/Detroit Pistions, San Antonio Spurs, Dallas Mavericks, LA Lakers.
The Merriweathers with current NFL Players/Oakland Raider’s John Jacoby and Darrius Heyward-Bey.
Left: Mr. and Mrs. Michael Merriweather with Right: Mr. and Mrs. Dwayne Woodruff (Pittsburgh Steelers)
Far Left: Michael Merriweather Pittsburgh Steelers; Minnesota Vikings… Right: Tony Dungy (Former Tampa Bay Buccaneers Head Coach and Former Pittsburgh Steelers
Far Left: Ken Clark (Former Minnesota Vikings) Far Right: Michael Merriweather (Former Pittsburgh Steelers, Minnesota Vikings, New York Jets and Green Bay Packers)
Left: Evander Holyfield—Boxer
Right Back: Ken Clark—Former NFL Player, Minnesota Vikings.
NFL Players and Friends
Right: Wade Phillips—Former Dallas Cowboys Head Coach/Houston Texans Defensive Coordinator.
Former NFL Players for the Pittsburgh Steelers at Mel Blount’s ALL Star Celebrity Roast
Michael Merriweather and Right: Brett Favre (Retired NFL Quarter Back; Green Bay Packers, Atlanta Falcons, NY Jets, Minnesota Vikings.
Left: Adrian Peterson—Current NFL RB for the Minnesota Vikings Middle: Mike Merriweather (Retired NFL Linebacker/Minnesota Vikings, Pittsburgh Steelers, Jets, Packers Right: Brad Childress (Former Minnesota Vikings Coach)
Pittsburgh Steelers Stadium—Heinz Field
Right: Rob Woodson (Retired NFL Cornerback and Safety/Pittsburgh Steelers, Baltimore Ravens, San Francisco 49ers and Oakland Raiders, Hall of Famer.
Left: Robin Cole—Retired NFL Linebacker & Pro Bowler/Pittsburgh Steelers Right: Mike Merriweather—Retired NFL Linebacker & 3 time Pro Bowler/Pittsburgh Steelers, Minnesota Vikings…
Mrs. Sandra Merriweather at Pittsburgh Steelers Stadium Heinz Field.
Michael Merriweather Minnesota Vikings.
Michael Merriweather #57 NFL Linebacker standing beneath picture at Heinz Field of the Pittsburgh Steelers.
Right: Stephone Paige—Retired NFL Player/Kansas City Chiefs and Minnesota Vikings with fan Ray Talley.
Pittsburgh Steelers’ Great Hall at Heinz Field including Michael Merriweather #57.
Michael Merriweather of the Pittsburgh Steelers AKA “Sack Man” - 11 years as a NFL Linebacker - Three time consecutive Pro Bowler (1984-1986) out of the University of the Pacific in the 1982 NFL Draft; 6 seasons as a “Pittsburgh Steelers.” - Named “All Pro” three times (1984, 1986, 1987). - Set a 1984 Steelers’ record for sacks (15) which was 5th best in the NFL - Career Sacks with the Steelers totaled 31 and currently tied 14th on the all-time Steelers’ Sack list; 11 interceptions; 2 defensive TD’s; Steelers’ MVP 1987 - 1989 draft-day trade to Minnesota Vikings 1st-round pick - Led the Minnesota Vikings in tackles in 1990 and 1991 ranking #2 on the team in 1992. - Minnesota Vikings’ 1989 career-high with 189 tackles, scored a TD on an interception return against Detroit making NFL history when he blocked a punt out of the end zone for a safety against the LA Rams in overtime to win the game; the first time an NFL game ended on a safety in overtime. His tackles still rank as the 9th-best mark in team history and no Viking has had as many tackles in a season since. *Merriweather started all 63 games he played for the Vikings. He was named NFC Defensive Player of the Week twice during his Vikings’ Career. - He played on NFC Central Championship teams in 1989 and 1992 advancing to the playoffs both seasons. - Merriweather finished his career playing for the New York Jets and Green Bay Packers both in 1993 and 1994. - Career Sacks: 41 - Interceptions: 18 - Defensive Touchdowns: 4
Left: Michael Merriweather, Retired NFL Linebacker—Pittsburgh Steelers, Minnesota Vikings, Jets and Packers; 3 time Pro Bowler, 5th in the NFL in Sacks; known to fans as “Sack Man”; the first player in NFL history to score the winning points after a game went into overtime with a safety when he blocked a punt out of the end zone. Right: “Ben” Roethlisberger, Current NFL Quarterback—Pittsburgh Steelers. He is the Youngest quarterback in NFL history to win Superbowls. He was only 23 years old when he and the Steelers obtained their second Super Bowl title. He is also known as one of the great ers in NFL history ranking number 10 alltime.
Right: “Ben” Roethlisberger, Pittsburgh Steelers’ Quarterback with Coach Tomlin.
Current Head Coach of the Pittsburgh Steelers: Coach Tomlin
THE NFL GAMES IN ACTION!
“Highlights of the Game!”
Mr. and Mrs. Michael Merriweather showing a little “Steeler Spirit in Pittsburgh Style”
Left: Jerome Bettis, AKA: “The Bus” Retired NFL Halfback-Los Angeles/St. Louis Rams and Pittsburgh Steelers
Left: Maurkice Pouncey #53, Current Lineman-Pittsburgh Steelers
Left: Hines Ward, Retired NFL’s Wide Receiver—Pittsburgh Steelers
Former Pittsburgh Steelers, Mike Merriweather and Jerome Bettis having a good time!
Right: Jerry Rice, Retired NFL’s Wide Receiver: S.F. 49ers, AFC Championship with Oakland Raiders, HOF.
A little action between Merriweather’s former team, “The Jets and San Francisco 49ers”
“Get Ready, Get Set, Let’s Go!”
“Bubba” Paris: Former NFL Offensive Lineman—San Francisco 49ers
Right: Marcus Allen, NFL’s Running Back and Football Analyst—Los Angeles Raiders, Kansas City Chiefs, 6 time Pro Bowler.
Right: Larry Fitzerald, Current Wide Receiver—Arizona Cardinals
“The Merriweathers enjoying their vacation”
Northern California Chapter NFL Alumni Helping Children Succeed!
…and they truly care for kids across the country!
The NFL Alumni ing football camps as they sign autographs,
and teach education along with life skills and ethics.
Merriweather teaching safety precautions, procedures and proper body mechanics
NFL Alumni working with children in sports individually while teaching skills and techniques.
“Teamwork is very important and everyone plays an important role.”
Left: Adrian Peterson, Current NFL Running Back—Minnesota Vikings Right: Michael Merriweather, Retired Linebacker—Pittsburgh Steelers and Minnesota Vikings v
ing the fans and charities by participating in Celebrity Basketball Players.
Celebrity Basketball Players
NFL Alumni with right: Mel Blount, Retired NFL Cornerback, NFL Defensive MVP, 5 time Pro Bowler, HOF
Middle: Hines Ward, Retired NFL’s Wide Receiver—Pittsburgh Steelers
Left: Jerome Bettis, Retired NFL Halfback—Los Angeles/St. Louis Rams and Pittsburgh Steeler with Mr. and Mrs. Michael Merriweather
My Cousins “Mookie” Jones, Charles Jones Former Wide Receiver—San Diego Chargers
Mr. and Mrs. Michael Merriweather
Left: Peja Stojakovic, Retired Professional Basketball Player—Sacramento Kings #16
Right: Ed “Too Tall” Jones, Retired NFL Player—Dallas Cowboys Defensive Lineman
Middle Back: Larry Fitzgerald, Current Wide Receiver—Arizona Cardinals
Right: Barry Sanders, Former NFL Running Back, HOF—Detroit Lions
….and some Steeler Wife Spirit!
Left: Billy “White Shoes” Johnson, Former Kickoff Returner—Houston Oilers Middle: Michael Merriweather, Former Linebacker—Pittsburgh Steelers, Minnesota Vikings, New York Jets and Green Bay New York Jets. Right: Erik McMillan, Former NFL Player—Philadelphia Eagles, NYJ, Cleveland Browns, Kansas City Chiefs.
I am blessed to be around people who enjoy giving and helping others. My contribution is to say, “Thank you Celebrity Ball Players and your families for all that you do and have done to our youth and those in need and may God forever bless you!”
…We are grateful to the Celebrity Players for working with our children, ing charities, sponsoring football camps, golf tournaments….
Left: Michael Merriweather Middle: “Mean Joe” Greene, Former NFL Defensive Tackle—Pittsburgh Steelers, HOF, 4x Superbowl Champion Right: Mel Blount
Michael and Coach Tomlin of the Pittsburgh Steelers
Left: Evander Holyfield (Boxer)
Left: Rob Woodson (Retired Cornerback and Safety—Pittsburgh Steelers, Baltimore Ravens, HOF
A Little Viking Spirit
Right: Larry Fitzgerald-WR for Arizona Cardinals. Left: Michael Merriweather
Left: Mike Ditka-Former NFL Player, TV Commentator and Coach for the Chicago Bears and New Orleans Saints totaling 13 years. Right: Michael Merriweather
Left: Donald Driver-Winner of Dancing with the Stars in 2012, Former NFL WR for the Green Bay Packers and Children’s Author. Right: Michael Merriweather)
Left: Drew Brees-Current New Orleans Saints Quarterback, selected to Pro Bowl 7x’s, NFL’s Comeback Player of the year in 2004… Right: Michael Merriweather
Left: Atiim Kiambu Hakeem-Ah (“Tiki” Barber)-Former NFL Runningback, NY Giants all-time rushing and reception leader post 2006 NFL post season… Right: Michael Merriweather
Right: Gary Weaver NFL Linebacker/Oakland Raiders
AutographsAutographs