Diabetic Foot - Case Presentation 4y2t3o
This document was ed by and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this report form. Report 3b7i
Overview 3e4r5l
& View Diabetic Foot - Case Presentation as PDF for free.
More details w3441
- Words: 2,020
- Pages: 54
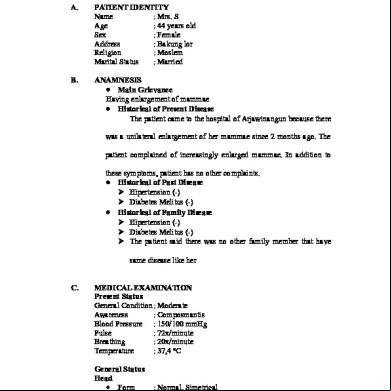
CASE PRESENTATION OF
DIABETIC FOOT By: Sharma
Dr. Siddhartha Under the guidance of
Dr. P.S. Lamba
History Pt. Abdul Sattar S/o Abdul Karim, 50 yrs. Muslim,. R/o Karoli itted on 22/10/11
Chief complaints# Pins and needle sensation × 1 year # Ulcer left foot × 1 month # Discharge from ulcer × 15 days
History HOPI Pins & needle sensation Left foot both feet ( Associated heaviness) Ulcer following trauma Papule pustule ulcer Discharge: yellow, foul smelling, blood stained No cough / coryza / burning micturition / Diarrhea / fainting episodes
Past history
K/c of NIDDM Diagnosed 6 yrs back
Taking treatment for past 4 years OHG drugs than switched to insulin and has stopped insulin from last 7-8 months
No H/o HT, TB
No H/o Surgery/ drug allergy
Nonsmoker, nonalcoholic
Examination
Awake, conscious, oriented, restless & anxious
Pallor++, Icterus -, clubbing -,cyanosis - , edema +
Left inguinal lymph nodes - 3×2 cm in size discrete, firm, mobile, tender, erythematous
Examination
PR - 100/min Regular Normal volume, character All peripheral pulses palpable including dorsalis pedis on affected side, No radio-femoral delay
BP – 130/70 mm Hg
Temperature afebrile
RR – 18/min
Local examination-Ulcer
Inspection- Single irregular ulcer,4-5 cm in size, extending from base of 2 nd metatarsal to 5 th metatarsal, inflamed, edematous, sloping edge, red floor with granulation tissue
Palpation- Tender, sloping edges with irregular margins, indurated base, depth 3mm, not bleeding on touch, mobile, warm surrounding skin , peripheral pulses palpable
Investigations Hb- 8.1mg/dl FBS- 142mg/dl,
PP BS- 220 mg/dl
Blood urea- 97 mg/dl
S creatinine- 3.1 mg/dl
Na+ : 130 meq/l
K+ : 3.7meq/l
ECG-TWNL X-ray Chest- NAD Xray cervical spine- NAD Fundus examination -
Cl- : 104meq/l
Provisional diagnosis
DIABETIC FOOT WITH
NEPHROPATHY
www.plymouthdiabetes.org.uk/
Changes in the vasonervorum with resulting ischemia ? cause Increased sorbitol in feeding vessels block flow and causes nerve ischemia Intraneural acculmulation of advanced products of glycosylation
Abnormalities of all three neurologic systems contribute to ulceration
Autonomic system regulates sweating and perfusion to the limb
Loss of autonomic control inhibits thermoregulatory function and sweating
Result is dry, scaly and stiff skin that is prone to cracking and allows a portal of entry for bacteria leading to ulcer.
www.plymouthdiabetes.org.uk/
Wagner’s Classification 0 – Intact skin (impending ulcer) 1 – Superficial 2 – Deep to tendon, bone or ligament 3- Osteomyelitis 4 – Gangrene of toes or forefoot 5 – Gangrene of entire foot
Control of diabetes Education
Ambulation Shoe ware Skin and nail care Avoiding injury with F.B’s and Hot water
Local padding and dressing Antibiotics if infected Excision of infected bone Amputation
Diabetes
Clinical syndrome characterized by deficiency of insulin accompanied by hyperglycemia due to absolute or relative excess of glucagon.
DM in India
INDIA : Diabetic CAPITAL of the world 4 crore diabetics in India (19% of world’s diabetic population)
2.5% of India’s urban population is diabetic DIABETIC FOOT is most devastating with > 50,000 leg amputations/ every yr. due to D.M. in India
Diagnosis Plasma glucose Random
Fasting*
>11.1 mmol/l (200 mg/dl) >7.0 mmol/l (126 mg/dl)
Fasting*
6.1-7.0 mmol/l
(110- 126 mg/dl)
Blood glucose
Diagnosis
>10.0 mmol/l (180 mg/dl)
DM
>6.1 mmol/l
DM
(110 mg/dl) 5.6- 6.1 mmol/l
(101-110 mg/dl)
Impaired fasting glycemia -IFG
Fasting* no calorie intake for last 8 hours
Relation between whole blood and plasma glucose
Blood glucose + 15 % = Plasma glucose
1 m mol = 18.0 mg glucose 1 m mol/l = 18.0 mg glucose/dl
Oral glucose tolerance test 75 gms of oral glucose after adequate fasting B. sugar levels after 2 hrs of ingestion
Normal
mmol/l
mg/dl)
7.8 mmol/l
(140 mg/dl)
IFG 7.8-11.1 mmol/l
(140-200 mg/dl)
DM >11.1
(200
Glycated Haemoglobin (HbA1c)
Standard. method for assessment of long term glycemic control
When B glucose consistently
Reflects glycemic history over previous 2 to 3 months
Performed by HPLC
non-enzymatic glycation of Hb
Interpretation
<6.2% - normal
< 7 % - effectively normal
>9% - things begin to go wrong, development of osmotic diuresis & water & electrolyte loss
12-15% - verge of DKA
Problems due to disease Cardiovascular system
Premature atheroma formation
Chances of CAD (Male-double risk ; female-triple)
Incidence of silent MI
HT and its sequelae
Threshhold for arrhythmias
Cardiac dysautonomia may present with :
Sudden hypotension on induction Absence of tachy. and HT with intubation
Diabetic cardiomyopathy Sudden death
Problems due to disease
Renal system
More chances of ARF in perioperative period, due to - Intrinsic renal disease. - Hemodynamic impairment -Urosepsis
UTI-most common post op complication in diabetics undergoing surgery
Renal failure- incidence 7%, most common major complication
Problems due to disease CNS and PNS
Chances of CVA Peripheral Neuropathy - incidence of N. Injury & N ischemia ANS Dysfunction -Postural hypotension -Gastroparesis -Loss of signs of Hypoglycemia -Blunted Response to atropine & beta-blockers -Urinary stasis-
Problems due to disease Respiratory system 1 Ventilatory response to PaCo2
& PaO2
2 More chances of Respiratory tract infections 3 susceptibility to ventilatory depressant drugs 4
FVC and FEV( Due to glycosylation of tissue proteins in connective tissues)
5
2,3 DPG
release of O2 to tissues
Airway
Stiff t syndrome- restricted neck movements
Scleroderma of diabetes
Firm, woody, nonpitting edema of posterior neck and upper back
The prayer sign
Patient is unable to approximate the palmar surfaces of the phalangeal ts despite maximal effort
Palm print test Degree of interphalangeal t involvement can also be assessed by the ink impression made by the palm of dominant hand
Problems due to disease Other
Proliferative retinopathy- Vitreous H’mge on laryngoscopy and intubation Infection – poor wound healing – trophic ulcers – More chances of aspiration
Associated acute complications -DKA -NKHS -Hypoglycemia
Increased risk for intra-operative HYPOTHERMIA
Anaesthetic considerations
Anaesthetic management goals 1 To maintain glycaemic control 2 To avoid further deterioration of pre-existing end organ damage 3 To shift patient soon on pre op glycaemic control - drugs
Preoperative assessment -Aims
23% of diabetics diagnosed prior to surgery Type of DM & its duration Pre op evaluation and treatment of end organ damage which is responsible for 5-fold increase in perioperative mortality associated with D.M. Assessment of B. sugar control and to obtain a reasonable control with change to short acting drugs Limit hospital stay and decrease cost Quantification of risk
PAC To assess
Investigations
1 B sugar Control
BS- F &PP Hb1 A C
2 Nephropathy
Urine R/M, albumin microalbuminuria Kidney function tests
PAC To assess Investigations 3
Cardiac status
4
PVD
5 Retinopathy
ECG Chest X ray ECHO H/o intermittent claudication Blanching of feet Non healing ulcers Fundus exam
PAC To assess Investigations
Stiff t syndrome 6
7 Metabolic & electrolyte
X ray Cervical spine (lateral)
ABG S electrolytes Ketones-urine Postural changes in BP
PAC orders
Consent
NPO orders
Anxiolytic
Aspiration prophylaxis
Stop long acting insulin night before surgery
Monitoring IV fluids
Morning sample of blood sugar, serum electrolytes to be test
No insulin on morning of surgery
To arrange for dextrostix, insulin, glucometer etc.
Gentle transfer of patient
To be taken up as 1 st case
Problems due to surgery and anesthesia
Greater concern for aseptic precautions
Prevention of acute complications
Estimation of end organ damage
More chances of sepsis
Appropriate fluid and electrolyte maintenance
Intensive monitoring
Stress response due to surgery
Regional anaesthesia
Regional anaesthesia
No absolute indication for spinal or epidural anesthesia
May improve outcome in selected situations
Decrease M&M in high risk patients
Extend analgesia into postoperative period
Advantages of regional anaesthesia in diabetics
Awake pt, intraop hypoglycemia (early recognition of hypoglycemia) can be noticed
Risk of aspiration, PONV chances
Blunt stress response to surgical stimulation
Avoidance of endotracheal intubation { stiff t syndrome & Gastroparesis}
Metabolic effects of anaesthetic agents avoided
Advantages of regional anaesthesia in diabetics
Lower the incidence of postoperative thromboembolic events
Decrease intraoperative blood loss
Epidural anaesthesia block catecholamine release irrespective of the segmental level
Rapid return to diet and insulin/ OHA
Disadvantages of Regional Anaesthesia in Diabetic patients
Risk of nerve injuries, higher adrenaline use increases risk of ischemic injury
LA requirement is low - sensitivity
Risk of infection
Epidural abscess
Contraindicated in presence of peripheral neuropathy
General Anaesthesia
Should be considered in -Presence of cardiovascular or renal disease -Prevension of intraoperative hypoglycemia and hypotension -Autonomic neuropathy( as it can mask hypoglycemia and may exacerbate respiratory depression with opioids) -Protection of pressure sores
General Anaesthesia
Anaesthesia - if gastric stasis a rapid sequence induction should be used. A nasogastric tube can be used to empty the stomach and allow a safer awakening..
Treat hypotension promptly. Hartmanns solution (Ringers lactate) should not be used in diabetic patients as the lactate it contains may be converted to glucose by the liver and cause hyperglycaemia.
Sudden bradycardias should respond to atropine 0.3mg iv, repeated as necessary (maximum 2 mg). Tachycardias, if not due to light anaesthesia or pain, may respond to gentle massage on one side of the neck over the carotid artery. If not then consider a beta-blocker (propanolol 1mg increments: max 10mg total or labetalol 5mg increments: max 200mg in total).
General Anaesthesia
IV induction agents normally cause hypotension on injection due to vasodilatation. If a patient has a damaged autonomic nervous system (and many diabetics do), then they cannot compensate by vasoconstricting, and the hypotension is worsened. Reducing the dose of drug and giving it slowly helps to minimise this effect.
Stress response and glucose metabolism
Glucagon, epinephrine, GH, steroids, Insulin Insulin resistance in post operative period Consequences - Osmolar diuresis-dehydration -disrupts autoregulation of vascular beds -impaired wound healing -decreased chemotaxis and impaired phagocytosis -more acute complications
Etomidate : Inhibitory effect on adrenal steroid genesis & glycaemic response to surgery
Midazolam : ACTH & cortisol secretion symapthoadrenal activity; but stimulates GH secretion
Net effect is ed glycaemic response to surgery
α-2 adrenergic agonists (Clonidine & Dexmedetomidine )sympathetic outflow from hypothalamus, inhibits release of ACTH with stimulation of GH release
Glycaemic control improved as a result of ed sympathoadrenal activity
-ing plasma C peptide concentarion indicating in endogenous insulin secretion
Propofol infusion in diabetic patients
“Lipid load resulting from propofol infusion may further lead to impairment of metabolism in diabetic patients.
Unlikely to be relevant during short anaesthesia / induction
Important if prolonged ICU sedation
Diabetes & Emergency Surgery
Usually infected
Usually uncontrolled
Dehydration
Metabolic decompensation
Resistance to insulin
Check blood glucose 1. <250 mg / dl, iv insulin – glucose, delay surgery till hydrated and electrolytes corrected 2. >250 mg /dl, check ketones, arterial blood gas, anion gap. If DKA present Large volume of normal saline iv Regular insulin 0.1U/ Kg/h after initial bolus of 0.15 U/Kg. Blood glucose monitoring 1 hourly Potassium, magnesium and phosphate monitored 2 hourly and replaced accordingly Blood glucose < 250 g/dl start 5% dextrose with insulin. Once acidosis corrected, blood glucose < 200 mg/dl, patient may be taken for surgery
51
Postoperative Complications
Hypoglycemia
Hyperglycemia – DKA, NKHC
Infections
Delayed wound healing
Periop MI risk
Problems due to autonomic neuropathy, postural
hypotension, atonic bleeding, urinary retention
PONV
Pain
watch till 72 hrs
Hypoglycemia Most frequent and dangerous complication of Insulin therapy Exacerbated by simultaneous istration of alcohol, OHA, ACE inhibitors, MAO inhibitors, and nonselective beta blockers Plasma glucose level less than 50 mg/dL If unconscious: 50 ml of 50% dextrose (D50) which increases glucose 100 mg/dLor 2 mg/dL/mL Insulin
Thanks
DIABETIC FOOT By: Sharma
Dr. Siddhartha Under the guidance of
Dr. P.S. Lamba
History Pt. Abdul Sattar S/o Abdul Karim, 50 yrs. Muslim,. R/o Karoli itted on 22/10/11
Chief complaints# Pins and needle sensation × 1 year # Ulcer left foot × 1 month # Discharge from ulcer × 15 days
History HOPI Pins & needle sensation Left foot both feet ( Associated heaviness) Ulcer following trauma Papule pustule ulcer Discharge: yellow, foul smelling, blood stained No cough / coryza / burning micturition / Diarrhea / fainting episodes
Past history
K/c of NIDDM Diagnosed 6 yrs back
Taking treatment for past 4 years OHG drugs than switched to insulin and has stopped insulin from last 7-8 months
No H/o HT, TB
No H/o Surgery/ drug allergy
Nonsmoker, nonalcoholic
Examination
Awake, conscious, oriented, restless & anxious
Pallor++, Icterus -, clubbing -,cyanosis - , edema +
Left inguinal lymph nodes - 3×2 cm in size discrete, firm, mobile, tender, erythematous
Examination
PR - 100/min Regular Normal volume, character All peripheral pulses palpable including dorsalis pedis on affected side, No radio-femoral delay
BP – 130/70 mm Hg
Temperature afebrile
RR – 18/min
Local examination-Ulcer
Inspection- Single irregular ulcer,4-5 cm in size, extending from base of 2 nd metatarsal to 5 th metatarsal, inflamed, edematous, sloping edge, red floor with granulation tissue
Palpation- Tender, sloping edges with irregular margins, indurated base, depth 3mm, not bleeding on touch, mobile, warm surrounding skin , peripheral pulses palpable
Investigations Hb- 8.1mg/dl FBS- 142mg/dl,
PP BS- 220 mg/dl
Blood urea- 97 mg/dl
S creatinine- 3.1 mg/dl
Na+ : 130 meq/l
K+ : 3.7meq/l
ECG-TWNL X-ray Chest- NAD Xray cervical spine- NAD Fundus examination -
Cl- : 104meq/l
Provisional diagnosis
DIABETIC FOOT WITH
NEPHROPATHY
www.plymouthdiabetes.org.uk/
Changes in the vasonervorum with resulting ischemia ? cause Increased sorbitol in feeding vessels block flow and causes nerve ischemia Intraneural acculmulation of advanced products of glycosylation
Abnormalities of all three neurologic systems contribute to ulceration
Autonomic system regulates sweating and perfusion to the limb
Loss of autonomic control inhibits thermoregulatory function and sweating
Result is dry, scaly and stiff skin that is prone to cracking and allows a portal of entry for bacteria leading to ulcer.
www.plymouthdiabetes.org.uk/
Wagner’s Classification 0 – Intact skin (impending ulcer) 1 – Superficial 2 – Deep to tendon, bone or ligament 3- Osteomyelitis 4 – Gangrene of toes or forefoot 5 – Gangrene of entire foot
Control of diabetes Education
Ambulation Shoe ware Skin and nail care Avoiding injury with F.B’s and Hot water
Local padding and dressing Antibiotics if infected Excision of infected bone Amputation
Diabetes
Clinical syndrome characterized by deficiency of insulin accompanied by hyperglycemia due to absolute or relative excess of glucagon.
DM in India
INDIA : Diabetic CAPITAL of the world 4 crore diabetics in India (19% of world’s diabetic population)
2.5% of India’s urban population is diabetic DIABETIC FOOT is most devastating with > 50,000 leg amputations/ every yr. due to D.M. in India
Diagnosis Plasma glucose Random
Fasting*
>11.1 mmol/l (200 mg/dl) >7.0 mmol/l (126 mg/dl)
Fasting*
6.1-7.0 mmol/l
(110- 126 mg/dl)
Blood glucose
Diagnosis
>10.0 mmol/l (180 mg/dl)
DM
>6.1 mmol/l
DM
(110 mg/dl) 5.6- 6.1 mmol/l
(101-110 mg/dl)
Impaired fasting glycemia -IFG
Fasting* no calorie intake for last 8 hours
Relation between whole blood and plasma glucose
Blood glucose + 15 % = Plasma glucose
1 m mol = 18.0 mg glucose 1 m mol/l = 18.0 mg glucose/dl
Oral glucose tolerance test 75 gms of oral glucose after adequate fasting B. sugar levels after 2 hrs of ingestion
Normal
mmol/l
mg/dl)
7.8 mmol/l
(140 mg/dl)
IFG 7.8-11.1 mmol/l
(140-200 mg/dl)
DM >11.1
(200
Glycated Haemoglobin (HbA1c)
Standard. method for assessment of long term glycemic control
When B glucose consistently
Reflects glycemic history over previous 2 to 3 months
Performed by HPLC
non-enzymatic glycation of Hb
Interpretation
<6.2% - normal
< 7 % - effectively normal
>9% - things begin to go wrong, development of osmotic diuresis & water & electrolyte loss
12-15% - verge of DKA
Problems due to disease Cardiovascular system
Premature atheroma formation
Chances of CAD (Male-double risk ; female-triple)
Incidence of silent MI
HT and its sequelae
Threshhold for arrhythmias
Cardiac dysautonomia may present with :
Sudden hypotension on induction Absence of tachy. and HT with intubation
Diabetic cardiomyopathy Sudden death
Problems due to disease
Renal system
More chances of ARF in perioperative period, due to - Intrinsic renal disease. - Hemodynamic impairment -Urosepsis
UTI-most common post op complication in diabetics undergoing surgery
Renal failure- incidence 7%, most common major complication
Problems due to disease CNS and PNS
Chances of CVA Peripheral Neuropathy - incidence of N. Injury & N ischemia ANS Dysfunction -Postural hypotension -Gastroparesis -Loss of signs of Hypoglycemia -Blunted Response to atropine & beta-blockers -Urinary stasis-
Problems due to disease Respiratory system 1 Ventilatory response to PaCo2
& PaO2
2 More chances of Respiratory tract infections 3 susceptibility to ventilatory depressant drugs 4
FVC and FEV( Due to glycosylation of tissue proteins in connective tissues)
5
2,3 DPG
release of O2 to tissues
Airway
Stiff t syndrome- restricted neck movements
Scleroderma of diabetes
Firm, woody, nonpitting edema of posterior neck and upper back
The prayer sign
Patient is unable to approximate the palmar surfaces of the phalangeal ts despite maximal effort
Palm print test Degree of interphalangeal t involvement can also be assessed by the ink impression made by the palm of dominant hand
Problems due to disease Other
Proliferative retinopathy- Vitreous H’mge on laryngoscopy and intubation Infection – poor wound healing – trophic ulcers – More chances of aspiration
Associated acute complications -DKA -NKHS -Hypoglycemia
Increased risk for intra-operative HYPOTHERMIA
Anaesthetic considerations
Anaesthetic management goals 1 To maintain glycaemic control 2 To avoid further deterioration of pre-existing end organ damage 3 To shift patient soon on pre op glycaemic control - drugs
Preoperative assessment -Aims
23% of diabetics diagnosed prior to surgery Type of DM & its duration Pre op evaluation and treatment of end organ damage which is responsible for 5-fold increase in perioperative mortality associated with D.M. Assessment of B. sugar control and to obtain a reasonable control with change to short acting drugs Limit hospital stay and decrease cost Quantification of risk
PAC To assess
Investigations
1 B sugar Control
BS- F &PP Hb1 A C
2 Nephropathy
Urine R/M, albumin microalbuminuria Kidney function tests
PAC To assess Investigations 3
Cardiac status
4
PVD
5 Retinopathy
ECG Chest X ray ECHO H/o intermittent claudication Blanching of feet Non healing ulcers Fundus exam
PAC To assess Investigations
Stiff t syndrome 6
7 Metabolic & electrolyte
X ray Cervical spine (lateral)
ABG S electrolytes Ketones-urine Postural changes in BP
PAC orders
Consent
NPO orders
Anxiolytic
Aspiration prophylaxis
Stop long acting insulin night before surgery
Monitoring IV fluids
Morning sample of blood sugar, serum electrolytes to be test
No insulin on morning of surgery
To arrange for dextrostix, insulin, glucometer etc.
Gentle transfer of patient
To be taken up as 1 st case
Problems due to surgery and anesthesia
Greater concern for aseptic precautions
Prevention of acute complications
Estimation of end organ damage
More chances of sepsis
Appropriate fluid and electrolyte maintenance
Intensive monitoring
Stress response due to surgery
Regional anaesthesia
Regional anaesthesia
No absolute indication for spinal or epidural anesthesia
May improve outcome in selected situations
Decrease M&M in high risk patients
Extend analgesia into postoperative period
Advantages of regional anaesthesia in diabetics
Awake pt, intraop hypoglycemia (early recognition of hypoglycemia) can be noticed
Risk of aspiration, PONV chances
Blunt stress response to surgical stimulation
Avoidance of endotracheal intubation { stiff t syndrome & Gastroparesis}
Metabolic effects of anaesthetic agents avoided
Advantages of regional anaesthesia in diabetics
Lower the incidence of postoperative thromboembolic events
Decrease intraoperative blood loss
Epidural anaesthesia block catecholamine release irrespective of the segmental level
Rapid return to diet and insulin/ OHA
Disadvantages of Regional Anaesthesia in Diabetic patients
Risk of nerve injuries, higher adrenaline use increases risk of ischemic injury
LA requirement is low - sensitivity
Risk of infection
Epidural abscess
Contraindicated in presence of peripheral neuropathy
General Anaesthesia
Should be considered in -Presence of cardiovascular or renal disease -Prevension of intraoperative hypoglycemia and hypotension -Autonomic neuropathy( as it can mask hypoglycemia and may exacerbate respiratory depression with opioids) -Protection of pressure sores
General Anaesthesia
Anaesthesia - if gastric stasis a rapid sequence induction should be used. A nasogastric tube can be used to empty the stomach and allow a safer awakening..
Treat hypotension promptly. Hartmanns solution (Ringers lactate) should not be used in diabetic patients as the lactate it contains may be converted to glucose by the liver and cause hyperglycaemia.
Sudden bradycardias should respond to atropine 0.3mg iv, repeated as necessary (maximum 2 mg). Tachycardias, if not due to light anaesthesia or pain, may respond to gentle massage on one side of the neck over the carotid artery. If not then consider a beta-blocker (propanolol 1mg increments: max 10mg total or labetalol 5mg increments: max 200mg in total).
General Anaesthesia
IV induction agents normally cause hypotension on injection due to vasodilatation. If a patient has a damaged autonomic nervous system (and many diabetics do), then they cannot compensate by vasoconstricting, and the hypotension is worsened. Reducing the dose of drug and giving it slowly helps to minimise this effect.
Stress response and glucose metabolism
Glucagon, epinephrine, GH, steroids, Insulin Insulin resistance in post operative period Consequences - Osmolar diuresis-dehydration -disrupts autoregulation of vascular beds -impaired wound healing -decreased chemotaxis and impaired phagocytosis -more acute complications
Etomidate : Inhibitory effect on adrenal steroid genesis & glycaemic response to surgery
Midazolam : ACTH & cortisol secretion symapthoadrenal activity; but stimulates GH secretion
Net effect is ed glycaemic response to surgery
α-2 adrenergic agonists (Clonidine & Dexmedetomidine )sympathetic outflow from hypothalamus, inhibits release of ACTH with stimulation of GH release
Glycaemic control improved as a result of ed sympathoadrenal activity
-ing plasma C peptide concentarion indicating in endogenous insulin secretion
Propofol infusion in diabetic patients
“Lipid load resulting from propofol infusion may further lead to impairment of metabolism in diabetic patients.
Unlikely to be relevant during short anaesthesia / induction
Important if prolonged ICU sedation
Diabetes & Emergency Surgery
Usually infected
Usually uncontrolled
Dehydration
Metabolic decompensation
Resistance to insulin
Check blood glucose 1. <250 mg / dl, iv insulin – glucose, delay surgery till hydrated and electrolytes corrected 2. >250 mg /dl, check ketones, arterial blood gas, anion gap. If DKA present Large volume of normal saline iv Regular insulin 0.1U/ Kg/h after initial bolus of 0.15 U/Kg. Blood glucose monitoring 1 hourly Potassium, magnesium and phosphate monitored 2 hourly and replaced accordingly Blood glucose < 250 g/dl start 5% dextrose with insulin. Once acidosis corrected, blood glucose < 200 mg/dl, patient may be taken for surgery
51
Postoperative Complications
Hypoglycemia
Hyperglycemia – DKA, NKHC
Infections
Delayed wound healing
Periop MI risk
Problems due to autonomic neuropathy, postural
hypotension, atonic bleeding, urinary retention
PONV
Pain
watch till 72 hrs
Hypoglycemia Most frequent and dangerous complication of Insulin therapy Exacerbated by simultaneous istration of alcohol, OHA, ACE inhibitors, MAO inhibitors, and nonselective beta blockers Plasma glucose level less than 50 mg/dL If unconscious: 50 ml of 50% dextrose (D50) which increases glucose 100 mg/dLor 2 mg/dL/mL Insulin
Thanks