Nclex Drug Cards 2t3p5g
This document was ed by and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this report form. Report 3b7i
Overview 3e4r5l
& View Nclex Drug Cards as PDF for free.
More details w3441
- Words: 19,883
- Pages: 136
Drug Med Cards
Drug Med Cards
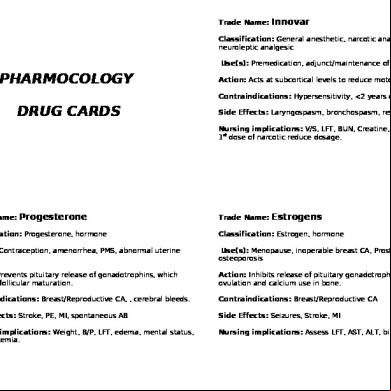
Table of Contents 1. Anti-Viral ........................................................................................................................................... 5 2. Benzodiazepenes .............................................................................................................................. 6 3. Diuretics ............................................................................................................................................ 8 4. Antiseizure Meds .............................................................................................................................. 9 5. Vitamins and Minerals .................................................................................................................... 13 6. Steroid ............................................................................................................................................. 14 7. Opiod............................................................................................................................................... 15 8. Opiod Antagonists........................................................................................................................... 17 9. NSAIDS ............................................................................................................................................ 18 10. Analgesic, Antipyretic ..................................................................................................................... 19 11. Anticholinergic ................................................................................................................................ 20 12. Bronchodilator ................................................................................................................................ 21 13. Thyroid Hormone Replacement ...................................................................................................... 22 14. Alpha Adronergic Receptor Antagonist .......................................................................................... 23 15. Antiparkinson (Cholinergic Receptor Antagonist............................................................................ 24 16. Fluid and Electrolytes ...................................................................................................................... 26 17. Antibiotics ....................................................................................................................................... 28 18. Cholesterol Lowering Agents .......................................................................................................... 32 19. Laxatives/ Stool Softeners............................................................................................................... 34 20. Anti-Diarrheal.................................................................................................................................. 36 21. Beta-Blockers .................................................................................................................................. 37 22. Nitrates ........................................................................................................................................... 39 23. ACE-Inhibitors ................................................................................................................................. 40 24. Calcium Channel Blockers ............................................................................................................... 41 25. Central Acting Antihypertensive ..................................................................................................... 42 26. Antihypertensives ........................................................................................................................... 43 27. Antipsychotics ................................................................................................................................. 44 28. Anti-Coagulants ............................................................................................................................... 50 29. Antiplatelets .................................................................................................................................... 51 30. Proton Pump Inhibitor .................................................................................................................... 52 31. H2- Receptor Antagonist ................................................................................................................. 53 32. Cerebral Stimulant .......................................................................................................................... 54 33. Antihistamines ................................................................................................................................ 55 34. Antidiabetic ..................................................................................................................................... 57 35. Antihypoglycemic ............................................................................................................................ 60 36. Anti-fungal....................................................................................................................................... 61 37. Eye Drops ........................................................................................................................................ 62 38. Antidepressant ................................................................................................................................ 63 39. Tricyclic Antidepressants ................................................................................................................ 65 40. Selective Serotonin Reuptake Inhibitor (SSRI) ................................................................................ 67 41. Monoamine Oxidase Inhibitors (MAOIs) ........................................................................................ 69 42. Anti-Emetic...................................................................................................................................... 70 43. Antituberculosis .............................................................................................................................. 71 44. Substance Abuse Deterrent ............................................................................................................ 72 45. Bone Metabolism Regulatory ......................................................................................................... 73 46. Bacterial Collagenase Enzyme......................................................................................................... 74 Bibliography ................................................................................................................................................ 75
Page 2 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards With over 8 years in the medical field, Mike Linares has worked both out in the field on an Ambulance in the dangerous streets of Los Angeles County and the in crazy busy the Emergency Rooms. Coupled with his ion for teaching & desire to help other students and mixed with his chronic typpos and bad grammmer, SIMPLEnursing.com was born to not only help his fellow RN students, but nursing students worldwide. "I hope you enjoy the valuable jewels that Simplenursing.com has to offer. If so please let me know! I am a real person & I´d love to hear your thoughts good or bad on Face book, Twitter, or Youtube." Committed to Your Success, Mike P.S.Feel free to Face book, Twitter, or Youtube me!!
Mike Linares Student Nurse Mentor & Certified EKG Instructor
HOW THIS WHOLE THING CAME TO BE... Before Helping Multiple Successful Nursing Students Excel I Was The "Drone" Nursing Student Working Too Hard & Eventually I FAILED OUT of Nursing School.
Before Helping Hundreds of Struggling Nursing Students Reach Graduation Day & Before Becoming a Student Nurse Mentor & Certified EKG Instructor, I Myself Was A Struggling "At Risk" Student Nurse Drowning In My Books & Lost In Clinical. I was that struggling student working full time in the Emergency Room at one of those MEGA hospitals in Orange, California. I worked as an EMT aka a "medic" for 8 years prior to failing out. I knew how to take care patients, I knew the basics of the ABCs of basic life , I knew how to take vital signs and how to fix minor injuries. I thought I had enough experience to skate right through nursing school, I thinking "how hard can it be" right? After two semesters, I FAILED out of the Program. I felt defeated, depressed and like a loser. It was one of the lowest points of my life. Sitting in my room practically bawling my eyes out, I quotes my mom and dad used to encourage me with, "son, whatever doesn´t kill you, Makes you Stronger" & " Failing is Not a Bad Thing, As long as learn, become better, and NEVER EVER QUIT"
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 3 of 75
Drug Med Cards My Clinial FAILURE form had bold red letters stating: LACK In Prepared LACK Organizational Skills LACK Critical Thinking with Nursing Process Ending with: "able to return next semester contingent upon demonstrating INCREASED COMPETANCIES in these core areas." "NEVER GIVE UP!!" my mom & dad used to tell me, so I set out on a Quest to develop a system to make Simplify Nursing School! What Happened Next Might Surprise you, In a systematic way to put all the "core competencies" of nursing school that instructors look for to students. My quest was to make it SIMPLE first and foremost, by cutting out the fluff and getting down to the nitty critty making it easier. The Goal Was To Make A Simple System... And the best part is it was really helping myself and other students in my class their tests when I would share with them my strategies and systems to help them their tests without having to memorize everything in the book!
This is where my mentoring for student nurses began. That's when something clicked and everything changed for me. It was like I had an Ah - HA moment! At that moment I realized there are better, more predictable, and more low cost ways to get higher test scores and have more critical thinking skills than the money I had been spending on dead end study books that claimed to help but really just confuse me more. I needed simplicity!!! Within the next six months I had created over 27 different student help systems, strategies and tactics that produced better results for me - some better than others. Then over the next few semesters I tracked, tested, and tweaked each system until my students were ing with a 82% or better on each and every test, 2 students being out of School for over 25 years & coming back to score 94% on their EKG cardiac test! Truly amazing & truly making me proud to be their mentor.
Page 4 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.
Anti-Viral
1.1. Acyclovir (Zovirax) Class: Antiviral Actions: reduces viral shedding and formation of new lesions and speeds healing time. Peak: 1.5-2hr. Half-life: 2.5-5hr. Indications: (IV treatment) viral encephalitis, herpes simplex, varicella-zoster virus (shingles/chickpox); (orally) herpes simplex, varicella-zoster virus; (topically) herpes labialis (cold sores) and initial episodes of herpes gentitalis Norm. Dosage, Freq, Route, Range: PO 400mg bid Max: 800mg/day Side Effects: headache, nausea, vomiting, diarrhea Nursing Considerations: Monitor I&O & hydration status. Lab tests: baseline and periodic renal function tests
1.2. Amantadine HCl (Symmetrel) Class: Antiviral; Central-Acting Cholinergic Receptor Antagonist; Antiparkinson Actions: Because Amantadine does not suppress antibody formation, it can be istered for interim protection in combination w/ influenza. Onset: w/in 48hrs. Peak: 1-4hrs Indications: Influenza A Treatment; Influenza A Preventative; Parkinsonism; Drug-Induced Extrapyramidal Symptoms (EPS) Norm. Dosage, Freq, Route, Range: PO 100mg 1-2times/day Side Effects: dizziness, light-headedness, difficulty in concentrating, insomnia, leukopenia Nursing Considerations: Lab tests: pH and serum electrolytes; monitor and report mental status changes, nervousness, difficulty concentrating, or insomnia, loss of seizure control, S&S of toxicity, especially in doses over 200mg/day
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 5 of 75
Drug Med Cards
2.
Benzodiazepenes
1.3. Alprazolam (Xanax) Class: Anxiolytic; Sedative-Hypnotic; Benzodiazepine Actions: A CNS depressant that appears to act at the limbic, thalamic, and hypothalamic levels of the CNS. Has antianxiety and sedative effects w/ addictive potential. Peak: 1-2 hr. Halh-life: 12-15 hr. Indications: Anxiety Disorders, Panic Attacks Norm. Dosage, Freq, Route, Range: PO 0.25-5 mg tid Max: 4 mg/day Side Effects: Drowsiness, sedation Nursing Considerations: Monitor S&S of drowsiness and sedation, especially in older adults or the debilitated, Lab tests: CBC, urinalysis and blood chemistry studies particularly during continuing therapy
1.4. Diazepam (Diastat, Valium) Class: Benzodiazepine Anticonvulsant; Anxiolytic Actions: Long-acting benzodiazepine psychotherapeutic agent. Benzodiazepines act at the limbic. Thalamic, and hypothalamic regions of the CNS and produce CNS depression resulting in sedation, and anticonvulsant activity dependent on the dosage. Onset: PO 30-60 min Peak: PO 1-2 hr Duration: IV 15 min-1 hr PO up to 3 hr Indications: Status Epilepticus, Muscle Spasm, Anxiety, Alcohol Withdrawal, Pre-op Norm. Dosage, Freq, Route, Range: IV/IM 5-10 m, repeat if needed at 10-15 min intervals up to 30 mg, then repeat if needed q2-4hr Side Effects: Drowsiness, fatigue, confusion, vivid dreams, headache Nursing Considerations: Monitor for adverse reactions, Monitor for therapeutic effectiveness-max effect may require 1-2 week, monitor for and report promptly signs of suicidal ideation especially in those treated for anxiety states accompanied by depression, observe patient closely and monitor vital signs when diazepam is given parentally; hypotension, muscular weakness, tachycardia, and respiratory depression may occur, Lab tests: periodic CBC and LFTs.
1.5. Lorazepam (Ativan) Class: Anxioltic; Sedative-Hypnotic; Benzodiazepine Actions: most potent of the available benzodiazepine. Effects (antianxiety, sedative, hypnotic, and skeletal muscle relaxant) are mediated by the inhibition neurotransmitter GABA. Action sites are thalamic, hypothalamic, and limbic levels of CNS. Onset: IV 1-5 min. IM 15-30 min. Peak: IM 60-9 min. PO 2 hr Duration 12-24 hr Indications: Antianxiety, Insomnia, Premedication, Status Epilepticus Norm. Dosage, Freq, Route, Range: PO 2-6 mg/day in divided doses Max: 10 mg/day Side Effects: drowsiness, sedation, dizziness, weakness Nursing Considerations: Supervise ambulation, Lab tests: Assess CBC and LFTs periodically
Page 6 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.6. Temazepam (Restoril) Class: Benzodiazepine, Anxiolytic, Sedative-Hypnotic Actions: reduces night awakenings and early morning awakenings; increases total sleep times, absence of rebound effects. Onset: 30-50 min. Peak: 2-3hr. Duration: 10-12hr. Half-life: 8-24hr Indications: to relieve insomnia Norm. Dosage, Freq, Route, Range: PO 7.5-30mg at bedtime Max: 30mg/night Side Effects: drowsiness, dizziness, lethargy Nursing Considerations: hypersensitivity, Lab tests: LFTs and kidney function tests during long-term use, be aware of S&S of overdose: weakness, confusion, slurred speech, ataxia, coma w/ reduced or absent reflexes, hypertension and respiratory depression
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 7 of 75
Drug Med Cards
3.
Diuretics
1.7. Furosemide (Lasix) Class: Loop diruetic Actions: Inhibits NA & Cl reabsorption, ↑ urine, ↓ edema & intravascular volume. Onset: PO 30-60min. IV 5 min Peak: PO 60-70min IV 20-60min. Duration: 2hr. Indications: promote urine output & decrease edema associated w/ CHF, cirrhosis of liver & kidney disease, decrease CHF, decrease hypertension Norm. Dosage, Freq, Route, Range: (Edema) PO: 20-80 mg in 1 or more divided doses Max: 600 mg/day (Hypertension) PO: 10-40 mg/kg bid Max: 480 mg/day Side Effects: Circulatory collapse, hypokalemia, aplastic anemia, agranulocytosis (rare) Nursing Considerations: check K+ levels prior to ., monitor I&O closely, rapid acting doses to prevent sleep disturbance, Potassium rich foods: bananas, oranges, dried dates, etc., CBC, serum and urine electrolytes, CO2 BUN, Blood Sugar, Uric Acid, Urine and Blood Glucose, HbA1C in diabetic patients w/ decompensated hepatic cirrhosis, may cause hyperglycemia
1.8. Hydrochlorothiazide (Microzide, Oretic) Class: Electrolytic and Water Balance; Thiazide Diuretic Actions: Therapeutic effectiveness is measured by decrease in edema and lowering of blood pressure. Onset: 2hr. Peak: 4hr. Duration: 6-12hr. Half-life: 45-120min. Indications: adjunct treatment of edema associated with CHF, hepatic cirrhosis, renal failure, and in the management of hypertension Norm. Dosage, Freq, Route, Range: PO 25-100mg/day in 1-3 divided doses Max: 200mg/day Side Effects: Hyperglycemia, hyperuricemia, hypokalemia Nursing Considerations: Check BP, monitor I&O and check for edema, Lab tests: baseline and periodic determinations of serum electrolytes, blood counts, BUN, blood glucose, uric acid, CO2, are recommended.
1.9. Spironolactone (Aldactone) Class: Electrolytic and water balance; Aldosterone Antagonist; Potassium-Sparing Diuretic Actions: A diuretic agent that promotes sodium and chloride excretion w/o concomitant loss of potassium. Lowers systolic and diastolic pressures in hypertensive patients. Effective in treatment of primary aldosteronism. Onset: gradual Peak: 2-3days; Max effect may take up to 2 weeks Duration: 2-3 days or longer Indications: Edema due to CHF, Hypertension, Primary Aldosteronism, Hypokalemia Norm. Dosage, Freq, Route, Range: PO 25-400mg/day in divided doses Max: 400mg/day Side Effects: fluid and electrolyte imbalance, nausea, vomiting Nursing Considerations: check BP, lab tests: monitor serum electrolytes (Na and K), assess for signs and symptoms of fluid and electrolyte imbalance, monitor daily I&O and check for edema
Page 8 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
4.
Antiseizure Meds
1.10. Carbamazepine (Carbatrol, Tegretol, Epitol, Equetro, Mazepine) Class: Anticonvulsant tricyclic Actions: effective anticonvulsant for a range of seizure disorders and as an adjuvant reduces depressive S&S and stabilizes mood. Peak: 2-8hr. Half-life: variable due to autoinduction 25-65hr. than 14-16he with repeated use Indications: Seizures; Trigeminal Neuralgia; Bipolar Disorder (Equetro) Norm. Dosage, Freq, Route, Range: PO 200mg bid, gradually increase to 800-1200mg/day in 3-4 divided doses Max: 1200mg/day Side Effects: leukopenia, confusion, headache, dizziness Nursing Considerations: Lab tests: baseline and periodic CBCs including platelets, reticulocytes, serum electrolytes and serum iron, LFTs, BUN and complete urinalysis, attempt a dosage reduction after 3 months, monitor for toxicity, I&O and vital signs
1.11. Clonazepam (Klonopin) Class: Anticonvulsant; Benzodiazepine Actions: Suppresses spike and wave discharge (petitmal) and decreases amplitude, frequency, duration, and spread of discharge in minor motor seizures. Onset: 60 min Peak: 1-2 hr Duration up to 12 hr in adults; 6-8 hr in children Indications: Seizures, Panic Disorders Norm. Dosage, Freq, Route, Range: PO 1.5mg/day in 3 divided doses, increased by 0.5-1 q3days until seizures are controlled or until intolerable adverse effects Max: 20 mg/day Side Effects: Drowsiness, sedation, ataxia Nursing Considerations: Monitor for signs of suicidal ideation in depressive individuals, Lab tests: periodic LFTs, platelet counts, blood counts, and renal function tests, Monitor for S&S of overdose, including somnolence, confusion, irritability, sweating, muscle and abdominal cramps, diminished reflexes, coma.
1.12. Gabapentin (Neurontin) Class: Anticonvulsant; Gaba Analog Actions: Used in conjunction with other anticonvulsants to control types of seizure in patients with epilepsy. Effective in controlling painful neuropathies Indications: Seizure disorder, Past-Herpetic Neuralgia, Restless Leg Syndrome Norm. Dosage, Freq, Route, Range: start at 300mg may slowly increase Max: 1,200mg/day Side Effects: drowsiness, fatigue Nursing Considerations: monitor for therapeutic effectiveness, may not occur until several weeks following initiation of therapy, monitor for and report dizziness, somnolence, or other sign of CNS depression
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 9 of 75
Drug Med Cards
1.13. Lamotrigine (Lamictal) Class: Anticonvulsant Actions: may act by inhibiting the release of glutamate and aspartate, excitatory neurotransmitters at voltage-sensitive sodium channels, resulting in decreased seizure activity in the brain. Onset: 12wks. Peak: 1-4hr. Indications: Seizures; Bipolar disorder Norm. Dosage, Freq, Route, Range: PO start w/ 25mg daily for 2 wks, then 50mg daily for 2 wks, then 100mg daily for 1 wk, then 200mg daily (low and slow) Side Effects: dizziness, ataxia, somnolence, headache, nausea, diplopia, blurred vision, Stevens-Johnson syndrome, toxic epidermal necrolysis, rhinitis Nursing Considerations: do not take med if skin rash develops, monitor pts. w/ bipolar disorder for worsening of their symptoms and suicidal ideation, use protection from sunlight or ultraviolet light until tolerance is known
1.14. Levetiracetam (Keppra) Class: Anticonvulsant Actions: The precise mechanism of antiepileptic effects is unknown. Peak: 1hr. Indications: Partial onset Seizures; Tonic Clonic Seizures; Myoclonic Seizures Norm. Dosage, Freq, Route, Range: 3,000mg/day or 1,000 mg/day ER tablet
PO/IV 500mg bid may increase by 500mg bid q2wks. Max:
Side Effects: Asthenia, headache, infection, somnolence, suicidal ideation Nursing Considerations: Lab tests: periodic CBC w/ diff, Hct, and Hgb, LFTs; monitor individuals w/ a history of psychosis or depression for S&S of suicidal tendencies, suicidal ideation, and suicidality
1.15. Oxcarbazepine (Trileptal) Class: Anticonvulsant Actions: Anticonvulsant properties may result from blockage of voltage-sensitive sodium channels, which results in stabilization of hyper-excited neural membranes. Peak: steady-state level reached in 2-3 days Indications: Partial Seizures Norm. Dosage, Freq, Route, Range: PO start w/ 300mg bid and increase by 600mg/day qwk. To 2,400mg/day in 2 divided doses for monotherapy or 1,22mg/day as adjunctive therapy Side Effects: fatigue, nausea, vomiting, abdominal pain, headache, dizziness, somnolence, ataxia, nystagmus, abnormal gait, Stevens-Johnson syndrome, toxic epidermal necrolysis, diplopia, vertigo, abnormal vision Nursing Considerations: Monitor for & report S&S of hyponatremia or CNS impairment; monitor phenytoin levels; Lab tests: periodic serum sodium, T4 level; monitor plasma level
Page 10 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.16. Phenobarbital (Solfoton) Class: Anticonvulsant; Sedative-Hypnotic; Barbiturate Actions: have anticonvulsant properties. Sedative and hypnotic effects appear to be due primarily to interference w/ impulse transmission of cerebral cortex by inhibition of reticular activating system. Limiting the spread of seizure activity results by increasing the threshold of motor cortex stimulation. Peak: PO 812 hr, IV 30 min Duration: IV 4-6 hr Indications: Anticonvulsant, Status Epilepticus, Sedative/Hypmotic Norm. Dosage, Freq, Route, Range: PO/IV 1-3 mg/kg/day in divided doses Side Effects: Somnolence, nightmares, insomnia, “hangover”, headache, anxiety Nursing Considerations: Observe patients receiving large doses for at least 30 min to ensure that sedation is not excessive, keep under observation, check IV site frequently, monitor serum drug levelsgreater than 50 mcg/mL may cause coma, expect restlessness
1.17. Phenytoin (Dilantin) Class: Anticonvulsant; Hydantoin Actions: Anticonvulsant action elevates the seizure threshold and/or limits the spread of seizure discharge. Accompanied by reduced voltage, frequency, and spread of electrical discharges w/in the motor cortex. Peak: Prompt Release: 1.5-3 hr Sustained Release: 4-12 hr Indications: To control tonic-clonic (grand mal) seizures, psychomotor and nonepileptic seizures (ex: Reye’s syndrome). Used to prevent or treat seizures occurring during or after neurosurgery. Not effective for absence seizures. Norm. Dosage, Freq, Route, Range: PO 15-20 mg/kg loading dose than 300 mg/day in 1-3 divided doses, may be gradually increased by 100 mg/week until seizures are controlled IV: 10-15 mg/kg then 300 mg/day in divided doses Side Effects: drowsiness, gingival hyperplasia, thrombocytopenia, leukopenia Nursing Considerations: Monitor Vital signs, Lab tests: periodic serum phenytoin concent., CBC w/ differential, platelet count, Hct, Hgb, serum glucose, serum calcium, serum magnesium, and LFTs
1.18. Pregabalin (Lyrica) Class: Anticonvulsant; Gaba-analog; Analgesic/Miscellaneous; Anxiolytic Actions: an analog of GABA that increases GABA levels and reduces calcium currents in the calcium channels of neurons. Peak: 1.5hr. Half-life:6hr. Indications: management of neuropathic pain associated with diabetic peripheral neuropathy or spinal cord injury, adjunctive therapy for adult patietns w/ partial-onset seizures, management of postherpetic neuralgia, fibromyalgia Norm. Dosage, Freq, Route, Range: PO 50-100mg tid Max: 300mg/day Side Effects: accidental injury, ataxia, dizziness, somnlonce, peripheral edema, weight gain, diplopia, blurry vision Nursing Considerations: Monitor for and report promptly mental status or behavior changes (e.g., anxiety, panic attacks, restlessness, irritability, depression, suicidal thoughts). Monitor for weight gain, peripheral edema and S&S of heart failure. Monitor diabetics for increased incidences of hypoglycemia.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 11 of 75
Drug Med Cards
1.19. Primidone (Mysoline) Class: Anticonvulsant; Barbiturate Actions: effective as an anticonvulsant in all types of seizure disorders except absent seizure. Peak: 4hr Half-life: 3-24hr Indications: management of complex partial and generalized tonic-clonic seizure Norm. Dosage, Freq, Route, Range: PO 250mg/day increased by 250mg/wk Max: 2g/day in 2-4 divided doses Side Effects: drowsiness, sedation, vertigo, ataxia, headache, nausea, vomiting, anorexia, leukopenia, thrombocytopenia Nursing Considerations: Lab tests: baseline and periodic CBC, complete blood chemistry (q6mo), and primidone blood levels (Therapeutic blood levels 5-10 mcg/mL). Monitor primidone plasma levels (concentrations greater than 10mcg/mL are usually associated w/ significant ataxia and lethargy). Observe for S&S of folic acid deficiency: mental dysfunction, psychiatric disorders, neuropathy, and megaloblastic anemia.
1.20. Valproic Acid (Depakote, Depacon, Depakene) Class: Anticonvulsant; GABA inhibitor Actions: Anticonvulsant w/ increased bioavailability of the inhibitory neurotransmitter GABA to brain neurons. Peak: 1-4hrs. Indications: Management of seizures; Migraine headache prophylaxis; Mania Norm. Dosage, Freq, Route, Range: (seizures) PO/IV: 10-15mg/kg/day in divided doses when total is greater than 25mg. increase at 1wk. intervals bu 5-10mg/kg/day until seizures are controlled Max: 60mg/kg/day (Mania) PO: 750mg/day istered in divided doses Side Effects: sedation, drowsiness, deep coma, death (w/ overdose), nausea, vomiting, indigestion, liver failure, pancreatitis, prolonged bleeding time, bone marrow depression Nursing Considerations: Lab tests: baseline platelet count, bleeding time, coagulation, parameters, and serum ammonia, LFTs, then repeat at least q2months of therapy, avoid alcohol
Page 12 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
5.
Vitamins and Minerals
1.21. Multivitamin (One-A-Day) Class: Vitamins Actions: Contain fat-soluble vitamins (A, D and E) and most water-soluble vitamins (B-Complex vitamins B1, B2, B3, B5, B6, B12, Vitamin C, Biotin, and Folic Acid). These vitamins are a diverse group of compounds necessary for growth and development. May act as coenzymes or catalysts in numerous metabolic processes. Onset, Peak, Duration: Unknown Indications: Treatment and prevention of vitamin deficiencies. Norm. Dosage, Freq, Route, Range: recommended by individual manufacturer
1 dose unit (capsule, tablet, dropperful)/day or amount
Side Effects: Urine discoloration, allergic reactions to preservatives, additives, or colorants Nursing Considerations: Asses patient for signs of nutritional deficiency before and throughout therapy.
1.22. Omega-3 Fatty Acids (Fish Oil, Omega-3 Fatty Acids) Class: Nutritional Supplement, Omega-3 Fatty Acids Actions: is not completely understood. May include inhibition of acetyl-CoA and increased peroxisomal beta-oxidation in the liver. Indications: Hypertriglyceridemia Norm. Dosage, Freq, Route, Range: PO 4 g daily as single or divided doses Max: 4 g/day Side Effects: Back pain, flu syndrome, unspecified pain Nursing Considerations: Monitor for S&S of hypersensitivity in those w/ known allergy to fish, Lab tests: baseline and periodic lipid profile
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 13 of 75
Drug Med Cards
6.
Steroid
1.23. Dexamethasone Sodium Phosphate (Baycadron, Decadron, Dexamethasone) Class: Adrenal Corticosteroid; Glucocorticoid Actions: Long-acting synthetic adrenocorticoid with intense anti-inflammatory activity and minimal mineralocorticoid activity. Onset: Rapid Peak: PO 1-2 hr IM 8 hr Duration: PO 2.75 days IM 6 days Intra lesional Intra-articular 1-3 weeks Indications: Allergies, Inflammation, Neoplasias, Adrenocorticol Function Abnormalities, Cerebral Edema, Shock Norm. Dosage, Freq, Route, Range: PO 0.25-4mg bid to qid IM 8-16mg q1-3weeks IV 0.75-0.9mg/kg/day divided q6-12hr. Max: 16mg/day Side Effects: Nasal Irritation, edema, hyperglycemia, impaired wound healing, subacapsular cataract, oral candidiasis Nursing Considerations: take drug exactly as prescribed, report lack ir response to med or malaise, orthostatic hypotension, muscular weakness and pain, nausea, vomiting, anorexia, hypoglycemic reaction, or mental depression to prescriber, report any changes in appearance and easy bruising
1.24. Fluticasone (Flonase, Flovent) Class: Synthetic steroids of glucocorticoid family of drugs Actions: Fluticasone mimics the naturally-occurring hormone produced by the adrenal glands, cortisol or hydrocortisone. The exact mechanism of action of fluticasone is unknown. Fluticasone has potent antiinflammatory actions. Onset: 1-3 wk. Peak: 4-8hr. Indications: Seasonal allergy rhinitis Norm. Dosage, Freq, Route, Range: Intranasal 100 mcg (1 inhalation) per nostril 1-2 times daily Max: 4 times daily Side Effects: transient nasal irritation, burning, sneezing, epitaxis, bloody mucous, nasopharyngeal itching, dryness, crusting, and ulceration, headache, nausea, vomiting Nursing Considerations: oral and nasal inhalers are not to be used interchangeably, use of oral and nasal inhaler provided by manufacturer should be carefully reviewed with patient
1.25. Triamcinolone Acetonide (Nasacort HFA) Class: Adrenal Corticosteroid, Glucocorticoid Actions: Anti-inflammatory and immunosuppressant drug that is effective in the treatment of bronchial asthma. Onset: PO & IM 24-48hr. Peak: PO 1-2hr. IM 8-10hr. Duration: PO 2.25 days IM 1-6wks. Indications: Anti-inflammatory or immunosuppressant agent. Orally inhaled: Bronchial asthma in patient who has responded to conventional inhalation treatment. Does not suppress hypothalamic-pituitaryadrenal axis Norm. Dosage, Freq, Route, Range: Inhaled 2-4 inhalations
IM/SQ/Intra-auricle/Intradermal 4-48 mg/day in divided doses
Side Effects: headache, nausea, vomiting, insomnia, confusion, peptic ulcer Nursing Considerations: notify prescriber if wheezing occurs immediately following a dose, monitor for signs of negative nitrogen balance, lab tests: periodic serum electrolytes and blood glucose
Page 14 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
7.
Opiod
1.26. Fentanyl (Duragesic) Class: Opioid Analgesic Actions: Binds to opiate receptors in the CNS, alters response and perception of pain. Onset: IV immediate, IM min. Transdermal: 12-24hr. Peak: IV 3-5min. Transdermal: 24-72hrs. Duration: IV 30-60min IM 1-2hr. Transdermal 72hrs. Indications: For moderate to severe chronic pain requiring continuous opioid analgesic therapy. Norm. Dosage, Freq, Route, Range: 25-100mcg/hr. for 72hr. transdermal patch Side Effects: CNS depression, do not drink or eat grapefruit, polypharmacy Nursing Considerations: BP, Pulse, Respirations <6 need Narcan
1.27. Hydrocodone Bitartrate (Mycodone) Class: Narcotic (Opiate Agonist) Analgesic; Antitussive Actions: CNS suppressant with moderate to severe pain relief of pain. Suppress cough reflex by direct action on cough center in medulla. Onset: 10-20 min Duration: 3-6 hr Indications: Mild to Moderate pain, Cough Norm. Dosage, Freq, Route, Range: 5-10 mg q4-6hr PRN Max: 60 mg/day Side Effects: constipation, nausea, drowsiness, respiratory depression Nursing Considerations: Monitor for effectiveness of drug for pain relief, nausea and vomiting, respiratory status and bowel elimination
1.28. Hydromorphone (Dilaudid) Class: Narcotic, Analgesic Actions: Potent opiate receptor agonist that does not alter pain threshold but changes the perception of pain in CNS. An effective narcotic analgesic that controls mild to moderate pain; has antitussive properties. Onset: IV 15min., PO 30min. Peak: 30-90min. Duration: 3-4hrs. Indications: Relief of moderate to severe pain Norm. Dosage, Freq, Route, Range: PO 2.5-10 mg q4-6hr Max: 60mg/day SQ/IM/IV 0.75-2 mg q4-6hr Max: 12 mg/day Side Effects: depression
Nausea, vomiting, constipation, drowsiness, hypotension, tachycardia, respiratory
Nursing Considerations: Baseline respiratory rate, rhythm, and depth & size of pupils;; respirations ↓ 12/min. or less & mitosis are signs of toxicity, monitor vital signs at reg. intervals, monitor I&O ratio & pattern for urinary retention, monitor bowel pattern, √ for nausea/vomiting and orthostatic hypotension.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 15 of 75
Drug Med Cards
1.29. Morphine Sulfate (Astramorph PF, Avinza, Depo-Dur, Duromorph) Class: Analgesic, Narcotic (opiate agonist) Actions: Controls severe pain, also used as an adjunct to anesthesia. Peak: PO 60min. PR 20-60min. SQ 30-60min. IM 30-60min. IV 20min. Duration: 7hr. Indications: Pain relief Norm. Dosage, Freq, Route, Range: PO 10-30 mg q4hr or 15-30 mg sustained release q8-12hr Max: 180 mg/day IV 2.5-15 mg/70kg q2-4hr or 0.8-10 mg/hr by continuous infusion, may increase PRN to control pain or 5-10 mg given epidurally q24hr IM/SQ 5-20 mg q4hr PRN Max: 120 mg/day PR10-20 mg q4hr PRN Max: 120 mg/day Side Effects: hypersensitivity, nausea, vomiting, constipation, urinary retention Nursing Considerations: Baseline respiratory rate, rhythm and depth and size of pupils, respirations 12/min and ↓and miosis are signs of toxicity, assess vital signs at regular intervals, encourage changes in positions, deep breathing, and coughing at regular intervals, Monitor I&O, √ for nausea and orthostatic hypotension
1.30. Oxycontin Class: Narcotic (opiate agonist); Analgesic Actions: Semisynthetic derivative of an opium agonist the binds with stereo-specific receptors in various sites of CNS to alter both perception of pain and emotional response to pain. Onset: 10-15 min. Peak: 3060 min. Duration: 4-5 hr. Indications: Moderate to severe pain Norm. Dosage, Freq, Route, Range: PO 5-10 mg q6hr (may titrate up to 10-30 mg q4hr PRN) Immediaterelease 10 mg q12hr (may titrate up) Max: 180 mg/day Side Effects: sedation, constipation, light-headedness, dizziness, fainting, hepatotoxicity Nursing Considerations: Monitor patient’s response closely, especially to sustained-release preparations, Lab tests: monitor LFTs and hematologic status periodically in patients on high dose, evaluate patients continued need
Page 16 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
8.
Opiod Antagonists
1.31. Naloxone (Narcan) Class: Opioid Antagonist Actions: A potent narcotic antagonist, essentially free of agonistic (morphine-like) properties. Reverses the effects of opiates, including respiratory depression, sedation, and hypotension. Onset: 2 min Duration: 45 min Indications: Opiate Overdose Norm. Dosage, Freq, Route, Range: IV 0.4-2mg, may repeat q2-3min up to 10mg if necessary Max: 10mg Side Effects: increased BP, tachycardia, nausea, vomiting Nursing Considerations: Observe patient closely; duration of action of some narcotics may exceed that of naloxone. Keep prescriber informed
1.32. Naltrexone HCL (Vivitrol) Class: Narcotic (opiate Antagonist) Actions: Weakens or completely and reversibly blocks the subjective effects (the “high”) of IV opioids and analgesics possessing both agonist and antagonist activity. Onset: 15-30min Peak: 1hr. Duration: PO 2472hr. IM 4wk. Indications: Opioid Dependence; Alcohol Dependence Norm. Dosage, Freq, Route, Range: PO 25mg followed by another 25mg in 1hr. if no withdrawal response; maintenance regimen of 50-150mg/day is individualized Max: 800mg/day IM 380mg q4wk Side Effects: nausea, vomiting, abdominal cramps/pain, hepatotoxicity, muscle & t pains, difficulty sleeping, anxiety, headache, nervousness Nursing Considerations: Lab tests: check LFTs before the treatment is started, at monthly intervals for 6 months, and then periodically as indicated; do not self-medicate w/ OTC drugs; report promptly onset of signs of hepatic toxicity to prescriber
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 17 of 75
Drug Med Cards
9.
NSAIDS
1.33. Celecoxib (Celebrex) Class: Analgesic; NSAID; Cyclooxygenase-2 (Cox-2) Inhibitor; Anti-inflammatory Actions: Exhibits anti-inflammatory; analgesic, and antipyretic activities. Reduces or eliminates the pain of rheumatoid and osteoarthritis. Peak: 3 hr Indications: Osteoarthritis/Arthritis/Ankylosing Spondylitis, Rheumatoid Arthritis Norm. Dosage, Freq, Route, Range: PO 100mg bid Max: 200mg Side Effects: back pain, dizziness, headache, insomnia, diarrhea, abdominal pain Nursing Considerations: Lab tests: periodically monitor Hct and Hgb, Lfts, BUN, and Creatinine and serum electrolytes, monitor closely lithium levels, monitor closely PT/INR, monitor for fluid retention and edema
1.34. Indomethacin (Indocin) Class: Analgesic, Non-steroidal Anti-inflammatory (NSAID) Actions: It is a potent analgesic, anti-inflammatory, and antipyretic agent. Promotes closure of persistent patent ductus arteriosus. Onset 1-2 hr. Peak: 3 hr. Duration: 4-6 hr. Indications: palliative treatment in active stages of moderate to severe rheumatoid arthritis, ankylosing rheumatoid spondylitis, acute gouty arthritis, and osteoarthritis of hip in patients intolerant to or unresponsive to adequate trials with salicylates and other therapy. Also used IV to close patent ducus arteriosus in the premature infant. Norm. Dosage, Freq, Route, Range: PO/PR: 50 mg tid until pain is tolerable, then rapidly taper Max: 150 mg/day Side Effects: dizziness, tinnitus, nausea, vomiting Nursing Considerations: Monitor for effectiveness, question patient carefully regarding aspirin sensitivity before initiation of therapy, observe patients carefully, Lab tests: monitor renal function, LFTs, CBC w/ differential, BP and HR, visual and hearing acuity periodically
1.35. Ketorolac (Acular, Acuvail, SPRIX) Class: Analgesic, NSAID, Anti-inflammatory, Antipyretic Actions: It inhibits synthesis of prostaglandins by inhibiting both COX-1 and COX-2 enzymes. Is a peripherally acting analgesic. It inhibits platelet aggregation and prolongs bleeding time. Peak: 46-60 min Indications: Pain Norm. Dosage, Freq, Route, Range: IV loading dose 30mg Max: 150mg/day on the first day then 120mg/day subsequent days Side Effects: drowsiness, nausea Nursing Considerations: Lab tests: periodic serum electrolytes and LFTs; urinalysis (for hematuria and proteinuria) with long-term use, monitor urine output, monitor for S&S of GI distress or bleeding including nausea, GI pain, diarrhea, melena, or hematemesis, GI ulceration with perforation can occur anytime during treatment
Page 18 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
10. Analgesic, Antipyretic 1.36. Acetominophen (Tylenol) Class: Nonnarcotic analgesic, Antipyretic Actions: provides temp. relief for mild to mod. pain, ↓ body temp. in indiv. w/ fever. Peak: 0.5-2 hr. Duration: 3-4 hr. Indications: Fever Reduction. Temporary relief of mild to moderate pain. Generally as substitute for aspirin when the latter is not tolerated or is contraindicated Norm. Dosage, Freq, Route, Range: PO: 325-650 mg q4h Max: 4 g/day PR: 650 mg q4h Max: 4 g/day Side Effects: Hepatotoxicity, hepatic coma, acute renal failure Nursing Considerations: Hepatotoxicity, even w/ mod. acetaminophen doses, especially in individuals with poor nutrition or who have ingested alcohol (3+ drinks daily) over prolonged periods; poisoning, usually from accidental ingestion or suicide attempts; potential abuse from psychological depend., do not take other meds containing acetaminophen, do not self-medicate adults for pain more than 10 days w/o consulting a doctor, do not use this med w/o medical direction for: fever persisting longer than 3 days, fever over 103, or recurrent fever
1.37. Acetaminophen Suppository (Tylenol Suppository) Class: Antipyretic, Non-opioid Analgesic Actions: Analgesic; Antipyresis. Peak: 0.5-2hrs. Duration: 3-4hrs. Indications: Mild pain, fever Norm. Dosage, Freq, Route, Range: PR 325-650mg q4-6hr. or 1gram 3xday Side Effects: Hepatic failure, renal failure, neutropenia, rash urticaria Nursing Considerations: Polypharmacy, renal-liver function, pain level, toxicity
1.38. Aspirin (ASA) Class: Non-narcotic, Antiplatelet, Antipyretic Actions: inhibiting the formation of prostaglandins involved in the production of inflammation, pain and fever, powerfully inhibits platelet aggregation. High serum salicylate concentrations can impair hepatic synthesis of blood coagulation factors VII, IX, X. Peak: 15min-2hr. Indications: Anti-inflammatory action, pain, fever reducer, antiplatelet Norm. Dosage, Freq, Route, Range: PO: 350-650 mg q4h Max: 4 g/day Side Effects: Bronchospasm, anaphylactic shock (laryngeal edema), nausea, heartburn, stomach pains, thrombocytopenia, hemolytic anemia Nursing Considerations: Allergy to any ASA, monitor for salicylate toxicity. In adults, a sensation of fullness in the ears, tinnitus, and decreased or muffled hearing are the most frequent symptoms.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 19 of 75
Drug Med Cards
11. Anticholinergic 1.39. Oxybutynin Cl (Anutrol, Ditropan, Gelnique, Oxytrol) Class: Anticholinergic; Antimuscaring; GU Antispasmodic Actions: Synthetic tertiary amine that exerts direct antispasmodic action and inhibits muscarinic effects of acetylcholine on smooth muscle of the urinary muscle. Onset: 0.5-1hr. Peak: 3-6hrs. Duration: 6-10hrs. Indications: Overactive Bladder Norm. Dosage, Freq, Route, Range: PO 5mg 2-4x/day Max: 20mg/day Side Effects: drowsiness, blurred vision, dry mouth, constipation, pruritus at application site (topical) Nursing Considerations: periodic interruptions of therapy are recommended to determine pt.’s need for continued treatment, tolerance has occurred in some pt.’s;; keep prescriber informed of expected responses to drug therapy (e.g., effect on urinary frequency, urgency, urge incontinence, nocturia, completeness of bladder emptying)
1.40. Glycopyrrolate (Robinul, Robinul Forte) Class: Anticholinergic, Antimuscarinic, Antipasmodic Actions: Inhibits motility of GI and genitourinary tract, it also decreases volume of gastric and pancreatic secretions, saliva, and perspiration. Onset: PO: 1 hr., IV: 1 min., IM/SQ: 15-30 min Peak: PO: 1 hr., IM/SQ: 30-45 min. Duration: PO: 8/12 hr., IM/SQ: 2-7 hr. Indications: Adjunctive management of peptic ulcer and other GI disorders associated with hyperacidity Norm. Dosage, Freq, Route, Range: PO: 1 mg tid or 2 mg bid or tid in equally divided intervals Max; 8 mg/day Side Effects: Decreased sweating, Xerostomia, Urinary hesitancy or retention Nursing Considerations: Monitor I&O ratio and pattern particularly in older adults, Monitor vital signs, especially when drug is given parenterally. Report any changes in heart rate and rhythym.
Page 20 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
12. Bronchodilator 1.41. Albuterol (Proventil, Ventolin) Class: Bronchodilator (Resp. Smooth Muscle Relaxant); Beta-Adrenergic Agonist Actions: Bronchodilation decreased airway resistance; facilitates mucous drainage, and increases vital capacity. Onset: Inhaled 5-15 min PO 30 min Peak: 0.5-2 hr PO 2.5 hr Duration: inhaled3-6 hr PO 4-6 hr (8-12hr w/ sustained release) Indications: Bronchospasm Norm. Dosage, Freq, Route, Range: PO 2-4 times/day, 4-8 mg sustained release 2 times/day Inhaled: 1-2 inhalations q4-6hr Side Effects: Tremor, anxiety, nervousness, headache, restlessness Nursing Considerations: Monitor effectiveness, Monitor S&S of fine tremor in fingers, Lab Tests: periodic ABGs, PFTs, pulse oximetry
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 21 of 75
Drug Med Cards
13. Thyroid Hormone Replacement 1.42. Levothyroxine (Synthroid) Class: Thyroid Hormone Replacement Actions: Raises T3 and T4 levels, Normal levels: 0.3-3, Restores metabolic rate. Peak: 3-4wks. Duration: 1-3wks. Indications: Specific replacement therapy for diminished or absent thyroid function Norm. Dosage, Freq, Route, Range: PO 25-50 mcg/day Max: 400 mcg/day Side Effects: insomnia, headache, irritability, nervousness, palpitations Nursing Considerations: monitor T3, & T4 levels, H.R., B.P., PT/INR
Page 22 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
14. Alpha Adronergic Receptor Antagonist 1.43. Tamsulosin HCL (Flomax) Class: Alpha Adrenergic Receptor Antagonist Actions: effectiveness is indicated by improved voiding. Improves symptoms related to BPH related to bladder outlet obstruction. Peak: 4-5hr. fasting 6-7hr. fed Half-life: 14-15hr. Indications: BPH Norm. Dosage, Freq, Route, Range: PO 0.4mg daily 30 min after meal Max 0.8mg/day Side Effects: headache, dizziness, orthostatic hypotension, rhinitis, abnormal ejaculation Nursing Considerations: Monitor for signs of orthostatic hypotension
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 23 of 75
Drug Med Cards
15. Antiparkinson (Cholinergic Receptor Antagonist 1.44. Benztropine Mesylate (Cogentin) Class: Centrally Acting Cholinergic Receptor Antagonist; Antiparkinson Actions: Synthetic centrally acting anticholinergic agent that acts by diminishing excess cholinergic effects associated w/ dopamine deficiency. Onset: IM/IV 15min. PO 1hr. Duration: 6-10hrs. Indications: Parkinsonism; Extrapyramidal reactions; Acute Dystonia Norm. Dosage, Freq, Route, Range: PO/IM 0.5-1mg/day may gradually increase as needed up to 6mg/day Side Effects: sedation, constipation, dry mouth, paralytic ileus Nursing Considerations: Monitor I&O ratio and pattern, monitor HR, monitor and report for muscle weakness
1.45. Donepezil (Aricept) Class: Central Acting Cholinergic; Cholinesterase Inhibitor Actions: improves global function, cognition, and behavior of patients with mild to moderate Alzheimer’s. Peak: 3-4hr. Half-life: 70hr. Indications: mild, moderate, or severe dementia of Alzheimer’s type. Norm. Dosage, Freq, Route, Range: PO 5-10mg at bedtime Max: 10mg/day Side Effects: headache, insomnia, nausea, diarrhea, vomiting, muscle cramps, anorexia Nursing Considerations: Monitor closely for S&S of GI ulceration and bleeding, monitor cardiovascular status, exercise caution
1.46. Ropinirole HCL (Requip) Class: Dopamine Receptor Agonist; Antiparkinson Actions: effectiveness indicated by improvement in idiopathic Parkinson’s disease. Peak: 1-2hr. Half-life: 6hr. Indications: Idiopathic Parkinson’s disease, restless leg syndrome Norm. Dosage, Freq, Route, Range: PO 0.25-4mg Max: 4mg Side Effects: fatigue, viral infection, dizziness, somnolence, sudden sleep attacks, syncope, nausea, vomiting, dyspepsia Nursing Considerations: Lab tests: periodically monitor BUN and creatinine, hepatic function and cardiac status
Page 24 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.47. Trihexyphenidyl HCL (Artane) Class: Centrally Acting Cholinergic Receptor Antagonist; Antiparkinson Agent; Antispasmodic Actions: thought to act by blocking excess of acetylcholine at certain cerebral synaptic sites. Relaxes smooth muscle by direct effect and by atropinelike blocking action on the PNS. Onset: w/in 1 hr. Peak: 23hr. Duration: 6-12hrs. Indications: Parkinsonism; Extrapyramidal reactions Norm. Dosage, Freq, Route, Range: PO 1mg day 1, 2mg day 2 then increased 2mgq3-5days up to 610mg/day in 3 or more divided doses Max: 15mg/day Side Effects: dry mouth, nausea, blurred vision, dizziness, nervousness Nursing Considerations: Monitor vital signs, assess and report severe CNS stimulation, monitor daily I&O if pt. develops urinary hesitancy
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 25 of 75
Drug Med Cards
16. Fluid and Electrolytes 1.48. Calcium Acetate (Norvasc) Class: Calcium Channel Blocker; Antihypertenive Actions: reduces systolic, diastolic, and mean arterial blood pressure. It also decreases pain due to angina. Peak: 6-9hr. Duration: 24hr. Half-life: less than 45yrs: 28-69hr. greater than 60yrs: 40-120hr. Indications: treatment of mild to moderate hypertension and stable angina Norm. Dosage, Freq, Route, Range: PO 5-10mg once daily Max: 10mg Side Effects: peripheral or facial edema, headache, abdominal pain, nausea Nursing Considerations: Monitor BP& HR, monitor for S&S of dose-related peripheral or facial edema, monitor BP w/ postural changes
1.49. Dextrose 50% (Dextrose, D50, D50W, Glucose) Class: Monosaccharide, principal form of charbohydrate used in the body Actions: Increase blood serum glucose levels. Onset: 5-20min Indications: hypoglycemia, coma or seizure of unknown etiology, refractory cardiac arrest Norm. Dosage, Freq, Route, Range: ½ to 1 full amp slow IV (25-100mL of 50% solution) Side Effects: pain, warmth, burning upon , phlebitis, sclerosis, thrombosis, Nursing Considerations: if smaller veins are used, local venous irritation may occur, infiltration may cause necrosis
1.50. Ergocalciferol (Calcidol, D-ViSol, Vitamin D2) Class: Vitamin D Analog Actions: distributed through the circulation and plays a major regulatory role. Responsible for regulation of serum calcium level. Indications: Nutritional Rickets, Osteomalacia, Hypoparathyroidism Norm. Dosage, Freq, Route, Range: PO 25-125 mcg/day for 6-12 weeks; may need to increase to 7.5 mg/day in patients w/ malabsorption. Peak: after 4 weeks Duration: 2 months or more. Side Effects: fatigue, weakness, vertigo, tinnitus, ataxia, muscle and t pain Nursing Considerations: Monitor closely patients receiving therapeutic doses of Vitamin D, must remain under close medical supervision, Lab tests: Serum calcium, phosphorus, magnesium, alkaline, phosphatase, BUN, periodic urine calcium, casts, albumin, and RBC, Monitor for hypercalcemia
Page 26 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.51. Ferrous Sulfate (Feosol) Class: Iron prepartion Actions: Standard iron preparation that corrects erythropoietic abnormalities induced by iron deficiency but does not stimulate erythropoiesis. Absorption: 5-10% absorbed in healthy individuals; 10-30% absorbed in iron deficiency; food decreases amount absorbed Indications: Iron deficiency, Iron supplement Norm. Dosage, Freq, Route, Range: PO 750-1500 mg/day in 1-3 divided doses Max: 1500 mg Side Effects: nausea, heartburn, constipation, black stools Nursing Considerations: Lab tests: monitor Hgb and reticulocyte values during therapy, continue iron therapy for 2-3 months after the hemoglobin level has returned to normal, monitor bowel movements as constipation is common
1.52. Magnesium Hydroxide (Magnesia, Magnesia Magna, Milk of Magnesia, M.O.M.) Class: Saline Cathartic; Antaid Actions: Aqueous suspension of magnesium hydroxide w/ rapid and long-acting neutralizing action. Causes osmotic retention of fluid, which distends colon, resulting in mechanical stimulation of peristaltic activity. Onset: 3-6hrs. Indications: Laxative Norm. Dosage, Freq, Route, Range: PO 2.4-4.8g/day (30-60mL) in 1 or more divided doses. Side Effects: nausea, diarrhea, complete heart block, other ECG abnormalities, respiratory depression, coma Nursing Considerations: Lab tests: monitor serum magnesium w/ signs of hypermagnesemia such as bradycardia, especially w/ frequent use of any degree of renal impairment
1.53. Potassium Chloride (KCl) Class: Electrolytes replacement solution Actions: For maintenance of intracellular isotonicity, transmission of nerve impulses, contraction of cardiac, skeletal and smooth muscles, normal kidney function and enzyme activity Indications: Potassium replacement Norm. Dosage, Freq, Route, Range: PO 10-100 mEq/day in divided doses Max: 100 mEq/day in divided doses Side Effects: Bacteremia, dizziness, edema, fatigue, fever, headache, infection, insomnia, rigors, hypertension, hypotension, tachycardia, abdominal pain, anorexia, constipation, diarrhea, dyspepsia, mucositis, nausea, anemia, febrile neutropenia, neutropenia, petechiae, thrombocytopenia, bilirubinemia, hyperglycemia, hypokalemia, hypomagnesemia, arthralgia, back pain, musculoskeletal pain, cough, dyspnea, epistaxis, pharyngitis, pruritus, rash, vaginal hemorrhage Nursing Considerations: Check serum K+ level, Normal level: 3.5-5.0, monitor I&O renal function
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 27 of 75
Drug Med Cards
17. Antibiotics 1.54. Amoxicillin & Clavulanic Acid (Augmentin) Class: Beta-Lactam, Antibiotic, Aminopenicillin Actions: Inhibits the final stage of bacterial cell wall synthesis , which leads to cell lysis and death. Peak: 1-2hrs. Indications: Infections caused by susceptible beta-lactamase-producing organisms, lower respiratory tract infections, acute bacterial sinusitis, community acquired pneumonia, otitis media, sinusitis, skin and skin structure infections, UTI Norm. Dosage, Freq, Route, Range: PO: 250-500 mg tablet Max:1500 mg/day Side Effects: Diarrhea, agranulocytosis (rare) Nursing Considerations: determine previous hypersensitivity reactions to penicillins, cephalosporins and other allergens prior to therapy, Lab tests: baseline C&S prior to initiation of therapy; start drug pending results, monitor for S&S of an urticarial rash (usually occurring within a few days after start of drug) suggestive of a hypersensitivity reaction, monitor for and report diarrhea which may indicate pseudomembranous colitis
1.55. Amoxicillin (Amoxil) Class: Antibiotic, Aminopenicillin Actions: Inhibits the final stage of bacterial cell wall synthesis, which results in bacterial cell lysis and death. Active against both aerobic gram-positive & aerobic gram negative bacteria. Onset: 1-2hr. Duration: 1-1.3hr. Indications: mild to moderate infections of ear, nose, throat, GU tract, skin, and soft tissue caused by susceptible bacteria, used in uncomplicated Gonorrhea Norm. Dosage, Freq, Route, Range: PO 250-500 mg q8h Max: 60-80 mg/kg/day Side Effects: Anaphaylaxis, pseudomembranous colitis (rare), agranulocytosis (rare), hypersensitivity Nursing Considerations: determine previous hypersensitivity reactions to penicillins, cephalosporins and other allergens prior to therapy, Lab tests: Baseline C&S tests prior to initiation of therapy; start drug pending results, periodic assessment of renal, hepatic and hematologic functions w/ prolonged therapy.
1.56. Ampicillin (Principen) Class: Antibiotic; Aminopenicillin Actions: A broad-spectrum, semi synthetic aminopenicillin that is bactericidal but is inactivated by penicillinase. Inhibits final stage of bacterial cell wall synthesis by binding to specific penicillin-binding proteins located inside the bacteria cell wall resulting in lysis and death of bacteria. Peak: Immed. After IV Duration: 6-8hrs. Indications: Infections of the GU, respiratory and GI tracts, and skin and soft tissues; gonococcal infections, bacterial meningitis, otitis media, sinusitis and septicemia and for prophylaxis of bacterial endocarditis. Used parentally only for moderately severe to severe infections. Norm. Dosage, Freq, Route, Range: PO/IV/IM 250-500 mg q6hr Max: 2000 mg/day Side Effects: Diarrhea, nausea, vomiting, rash
Page 28 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards Nursing Considerations: √ for allergies to penicillin’s, cephalosporin’s and other allergens prior to therapy, monitor closely for signs of hypersensitivity during the first 30 min. after ., Lab tests: baseline C&S prior to ., baseline & periodic renal assessment, monitor for diarrhea (may indicate pseudomembranous colitis)
1.57. Ceftriaxone Sodium (Rocephin) Class: Antibiotic, 3rd generation Cephalosporin Actions: preferentially binds to one or more of the penicillin-binding proteins located on the cell walls on susceptible organisms. Peak: 1.5-4hr after IM, immediately after IV Half-life: 5-10hr Indications: infections in lower respiratory tract, skin and skin structures, urinary tract, bones and ts, intra-abdominal infections, pelvic inflammatory disease, uncomplicated gonorrhea, meningitis, and surgical prophylaxis Norm. Dosage, Freq, Route, Range: IV/IM: 1-2g q12hr x 4-14days Max: 4g/day Side Effects: diarrhea, abdominal cramps Nursing Considerations: hypersensitivity, Lab tests: culture & sensitivity before initiation of therapy, periodic PT & INR, report diarrhea promptly
1.58. Clindamycin HCL (Cleocin) Class: Lincosamide Antibiotic Actions: Semisynthetic derivative if lincomycin that suppresses protein synthesis by binding to 50 S subunits of bacterial ribosomes, and, therefore, inhibits other antibiotics (ex: erythromycin) that act at this site. Peak: PO 45-60 min IM 3 hr Duration: PO 6 hr IM 8-12 hr Indications: Moderate to severe infections, Acne Vulgaris, Bacterial Vaginosis Norm. Dosage, Freq, Route, Range: PO 150-450 mg q6hr IM/IV 600-1,200 mg/day in divided doses Max: 2,700 mg/day Side Effects: Diarrhea, nausea, vomiting, skin rashes Nursing Considerations: Lab tests: C&S susceptibility testing should be performed initially, periodic CBC with differential, liver and kidney function tests, monitor BP and pulse in patients receiving drug parenterally, report diarrhea immediately with or w/o fever, be alert for signs of superinfection and anaphylactoid reactions
1.59. Cortisporin gtts (Cortisporin-TC) Class: Ophthalmic steroid, antibiotic (Suspension Only) Actions: Ear drops used to treat outer ear infections caused by bacteria (aka swimmer's ear). Contains neomycin and colistin, which are antibiotics that work by stopping the growth of bacteria. Also contains hydrocortisone, which is an anti-inflammatory corticosteroid that works by reducing ear swelling and discomfort, and thonzonium, which helps this med through dead cells and pus inside the ear. Indications: Only works for bacterial ear indications Norm. Dosage, Freq, Route, Range: 4 drops in affected ear 3-4 times daily Max: 16 drops/day Side Effects: This medication may temporarily sting or burn your ear for a minute or two when applied. Hearing problems, rash, itching/swelling, redness of the ears, dizziness Nursing Considerations: √ for allergies, rash, redness, itching or swelling to the ears, or any hearing problems
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 29 of 75
Drug Med Cards
1.60. Doxycycline Hyclate (Doryx, Doxy) Class: Antibiotic; Tetracycline Actions: blocks the binding of transfer RNA to the messenger RNA of bacteria, resulting in inhibition of bacterial protein synthesis. Peak: 1.5-4hr Half-life 14-24hr Indications: treatment of chlamydial and mycoplamal infections, gonorrhea, syphilis in penicillin-allergic patients, rickettsial diseases, acute exacerbations of chronic bronchitis Norm. Dosage, Freq, Route, Range: PO/IV 100mg q12hr on day 1, than 100mg/day as single dose Max: 100mg/q12hr Side Effects: nausea, vomiting, diarrhea Nursing Considerations: superinfections
report sudden onset of painful or difficult swallowing and evidence of
1.61. Gentamicin Ointment (Garamycin Ophthalmic) Class: Aminoglycoside Antibiotic Actions: Active against a wide variety of aerobic gram-negative but not anaerobic gram-negative bacteria. Also effective against certain gram-positive organisms, particularly penicillin-sensitive bacteria Indications: Moderate to Severe Infection Norm. Dosage, Freq, Route, Range: Topical 1-2 drops of solution in eye q4hr up to 2 drops q1hr or small amount of ointment bid or tid Side Effects: decreased creatinine clearance Nursing Considerations: Lab tests: perform C&S and renal function prior to first dose and periodically during therapy, watch Creatinine clearance levels, report S&S of ototoxic effect
1.62. Levofloxacin (Levaquin, Iquix, Quixin) Class: Quinolone Antibiotic Actions: A broad-spectum fluoroquinolone antibiotic that inhibits DNA-gyrase, an enzyme necessary for bacterial replication, transcription, repair, and recombination. Peak: PO 1-2 hr. Half-life: 6-8 hr. Indications: treatment of maxillary sinusitis, acute exacerbations of bacterial bronchitis, communityacquired pneumonia, uncomplicated skin/skin structure infections, UTI, acute pyelonephritis caused by susceptible bacteria, acute bacterial sinusitis, chronic bacterial prostatitis, nd bacterial conjunctivitis, treatment of pneumonic and septicemic plague. Norm. Dosage, Freq, Route, Range: PO: 500 mg q24hr x 10 days Side Effects: abdominal pain, nausea, headache, depression Nursing Considerations: Monitor for decreases pulse, perspiration, or pallor during insertion. Keep patient supine until these signs disappear, Monitor BP
Page 30 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.63. Linezolid (Zyvox) Class: Oxazolidinone Antibiotic Actions: Synthetic antibiotic that binds to a site on the 23S ribosomal RNA of bacteria, which prevents the bacterial RNA translation process, thus preventing further growth. Peak: PO 1-2 hr. Half-life: 6-7 hr. Indications: Vancomycin-Resistant Enterococcus faecium, pneumonia, complicated and uncomplicated skin infections
Nosocomial
or
community-acquired
Norm. Dosage, Freq, Route, Range: PO/IV: 600 mg q12hr x 14-28 days Max: 1,200 mg/day Side Effects: diarrhea, nausea, vomiting, constipation, taste alteration Nursing Considerations: Monitor S&S of bleeding, hypertension, or pseudomembranous colitis that begins w/ diarrhea, Lab tests: CBC, platelet count, Hgb, and Hct
1.64. Ofloxacin (Floxin) Class: Quinolone Antibiotic Actions: Inhibits DNA gyrase, an enzyme needed for bacterial DNA replication, broad spectrum against gram +&- most effective against gram – aerobic and anaerobic bacteria. Peak 1-2hr. Half-life: 5-7.5hr. Indications: Gonorrhea; Prosistitis; RTI (PO) OTIC (Tympanic) and Ocular; PID Norm. Dosage, Freq, Route, Range: 0.3% Opthalmic solution 1-2GTTs q2-4hr, qid 0.3% Otic solution GTTS q12hr. x days Side Effects: Dizziness, N&V, DTS menorrhea, menorrhagia, dysuria, urinary frequency Nursing Considerations: C&S, tendon PN, rash, seizures, S&S super infection
1.65. Vancomycin (Vancocin) Class: Antibiotic, Bacteriocidal Actions: Active against many gram-positive organisms. Inhibits cell-wall biosynthesis and alteration of bacterial cell-membrane permeability and RNA synthesis. Peak: 30min after end of infusion Half-life: 4-8hr. Indications: Infections Norm. Dosage, Freq, Route, Range: (C. Diff.) PO 125-500 mg q6h (Staph) PO 500 mg-2 g in 3-4 divided doses x 7-10 days Max: 2 g/day Side Effects: Nephrotoxicity leading to uremia, shock-like state, anaphylactoid reaction w/ vascular collapse, leukopenia, hypotension accompanied by flushing and erythematous rash on face and upper body (red-man syndrome) following rapid IV infusion Nursing Considerations: Allergy, monitor BP and HR, take peak & trough levels, assess hearing. Be aware that serum levels of 60-80 mcg/ml are associated w/ ototoxicity, monitor I&O. Oliguria or cloudy or pink urine may be a sign of nephrotoxicity
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 31 of 75
Drug Med Cards
18. Cholesterol Lowering Agents 1.66. Atorvastatin (Lipitor) Class: Anti-lipemic, HMG-COA, Reductase Inhibitor (statin) Actions: Adjunct to diet for reduction of LDL cholesterol and triglycerides in patients with primary hypercholesterolemia and mixed dyslipidemia, prevention of cardiovascular disease in patients with multiple risk factors. Onset: 2 wk. Peak: Plasma concentration 1-2 hr. effect 2-4 wk. Indications: Lowers LDL cholesterol, prevention of cardiovascular disease Norm. Dosage, Freq, Route, Range: PO start w/ 10-40 mg daily may increase up to 80 mg/day Max: 80 mg/day Side Effects: Back pain, hypersensitivity reaction, headache, abd. pain, constipation, diarrhea, flatulence, increased liver function tests, sinusitis, pharyngitis, rash Nursing Considerations: Lab tests: monitor lipid levels within 2-4 weeks after initiation of therapy or upon change in dosage, assess muscle pain, tenderness or weakness and if present, monitor K level (d/c drug with marked elevations of K or if myopathy is suspected, monitor carefully for digoxin toxicity with concurrent digoxin use, monitor prediabetics and diabetics for loss of glycemia.
1.67. Cholestyramine (Questrane, Prevalite) Class: Antilipemic; Bile Acid Sequestrant Actions: increase fecal loss of bile acids, which leads to lowered serum total cholesterol by decreasing LDL cholesterol, and reducing bile acid deposit in dermal tissues. Indications: as adjunct to diet therapy in management of patients w/ primary hypercholesterolemia w/ a significant risk of atherosclerotic heart disease and MI; for relief of pruritus secondary to partial biliary stasis Norm. Dosage, Freq, Route, Range: PO 4-8g bid to qid and before meals and at bedtime Max: 32g/day Side Effects: constipation, flatulence, abdominal pain Nursing Considerations: membranes, tarry stools
Monitor for petechiae, ecchymoses, abnormal bleeding from mucous
1.68. Fenofibrate (Tricor) Class: Antilipemic; Fibrate Actions: Fibric acid derivative w/ lipid-regulating properties. Lowers plasma triglycerides by inhibiting triglycerides synthesis and, as a result, lowers VLDL production as well as stimulates the catabolism of triglyceride-rich lipoprotein. Produces a moderate increase of HDL cholesterol levels in most patients. Peak: 6-8 hr. Half-life: 20 hr. Indications: Hypertriglyceridemia Norm. Dosage, Freq, Route, Range: PO 43-200 mg/day depending on product Max: 200 mg/day Side Effects: fatigue, headache, nausea, vomiting, flatulence, constipation Nursing Considerations: La tests: periodically monitor lipid levels, LFTs, and CBC w/ differential, assess for muscle pain, tenderness or weakness and if present monitor K level.
Page 32 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.69. Niacin (Niacor, Niaspan) Class: Vitamin B3; Antilipemic Actions: produces vasodilation by direct action on vascular smooth muscles. Inhibits hepatic synthesis of VLDL, cholesterol, and triglyceride, and indirectly LDL. Peak: 20-70 min. Half-life: 45 min. Indications: Niacin deficiency, Pellagra, Hyperlipidemia Norm. Dosage, Freq, Route, Range: PO 10-20 mg/day (Niacin Deficiency) 1.5-3g/day in divided doses, may increase up to 6 g/day if necessary (Hyperlipidemia) Max: 6 g/day Side Effects: headache, tingling, flushing with sensation of warmth, bloating, flatulence, itchy palms Nursing Considerations: monitor therapeutic effectiveness, Lab tests: obtain baseline and periodic blood glucose and LFTs in patients receiving prolonged high dose therapy, monitor diabetics, and monitor closely for evidence of liver dysfunction
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 33 of 75
Drug Med Cards
19. Laxatives/ Stool Softeners 1.70. Bisacodyl Suppository (Dulcolax) Class: Stimulant Laxative Actions: Expands intestinal fluid volume by increasing epithelial permeability. Induces peristaltic contractions by direct stimulation of sensory nerve endings in the colonic wall. Onset: PO 6-8hrs. PR 1560min. Indications: Temporary relief of acute constipation and for evacuation of colon before GI procedures. Norm. Dosage, Freq, Route, Range: PO 5-15 mg PRN Max: 30 mg for special procedures PR 10 mg PRN Side Effects: Mild cramping, nausea, vomiting, diarrhea, fluid and electrolyte disturbances (especially potassium and calcium) Nursing Considerations: evaluate periodically patient’s need for continued use of drug, add high-fiber foods slowly to regular diet to avoid gas and diarrhea, adequate fluid intake includes at least 6-8 glasses/day, use of laxatives results in ↓ absorption of Vitamin K
1.71. Docusate Sodium (Colace) Class: Stool softener Actions: detergent action lowers surface tension, permitting water and fats to penetrate and soften stools for easier age Indications: prophylactically in patients who should avoid straining during defecation and for treatment for constipation Norm. Dosage, Freq, Route, Range: PO 50-500mg/day PR 50-100mg added to enema fluid Max: 500mg/day Side Effects: diarrhea, nausea, bitter taste, abdominal cramps Nursing Considerations: Withhold if diarrhea develops and notify prescriber. Take sufficient liquid with each dose. So not take for prolonged periods (causes slowed bowel mobility).
1.72. Lactulose (Cephulac; Chronulac) Class: Hyperosmotic Laxative; Neurologic Actions: Osmotic effect on lactulose moves water from plasma to intestines, softening stools, and stimulates peristalsis by pressure from water content of stool. Indications: Chronic Constipation, prevention and treatment of portal-systemic encephalopathy (PSE) including stages of hepatic precoma and come Norm. Dosage, Freq, Route, Range: PO 30-60mL/day PRN Max: 60mL/day Side Effects: diarrhea, nausea, vomiting, flatulence Nursing Considerations: promote fluid intake (1,500-2,000mL/day or greater) during drug therapy for constipation
Page 34 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.73. Metoclopramide (Metozolv, Reglan) Class: GI Stimulant; Prokinetic agent Actions: potent central dopamine receptor antagonist that increases resting tone of esophageal sphincter, and tone and amplitude of upper GI contractions. Thus gastric emptying and intestinal transit are accelerated. Antiemetic action results from druf-induced elevation of CTZ threshold and enhanced gastric emptying. Onset: 30-60 min. Peak: 1-2 hr.Duration: 1-3 hr. Indications: GERD, Diabetic gastroparesis, Small –bowel intubation/Radiologic Exam, ChemotherapyInduced Emesis, Postoperative Nausea/ Vomiting Norm. Dosage, Freq, Route, Range: PO 10-15 mg qid before meals and at bedtime IM/IV 10 mg qid Max: 60 mg Side Effects: mild sedation, fatigue, restlessness, diarrhea Nursing Considerations: report S&S immediately, lab tests: periodic serum electrolytes, monitor for possible hypernatremia and hypokalemia, avoid alcohol and other CNS depressants, avoid driving for a few hours after drug .
1.74. Polyethylene Glycol (Miralax) Class: Laxatives, Osmotics Actions: Acts as an osmotic agent, drawing water into the lumen of the GI Tract. Peak: 2-4days Indications: Indicated for evacuation of GI Tract w/o water or electrolyte imbalance. Norm. Dosage, Freq, Route, Range: 17g w/ 8oz of water Side Effects: abdominal bloating, cramping, flatulence, nausea Nursing Considerations: GI obstruction, gastric retention, toxic colitis, megacolon, use cautiously in patients w/ abdominal pain of uncertain cause, particularly if accompanied w/ fever.
1.75. Sennosides (Senokot) Class: Stimulant Laxative Actions: Peristalsis stimulated by conversion of drug to active chemical. Onset: 6-10hr; may take up to 24hr. Indications: Acute constipation and preoperative and preradiographic bowel evacuation Norm. Dosage, Freq, Route, Range: PO 1-2 tabs at bedtime Max 4 tabs Side Effects: nausea, abdominal cramps, flatulence, watery diarrhea Nursing Considerations: Reduce dose in patients who experience considerable abdominal cramping
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 35 of 75
Drug Med Cards
20. Anti-Diarrheal 1.76. Diphenoxylate (Diphenatol, Lofene, Lomanate) Class: Antidiarrheal Actions: reduces GI motility. Onset: 45-60 min Peak: 2hr. Duration: 3-4hr. Indications: management of diarrhea Norm. Dosage, Freq, Route, Range: PO 5-10mL 3-4 times daily Max: 40mL/day Side Effects: hypersensitivity, flushing, palpitation, headache, dizziness Nursing Considerations: Assess GI function, monitor for S&S of dehydration, frequency and consistency of stools
1.77. Loperamide (Maalox, Imodium, Kaopectate, Pepto) Class: Antidiarrheal Actions: Inhibits GI peristaltic activity by direct action on circular and longitudinal intestinal muscles. Prolongs transit time of intestinal contents, increases consistency of stools, and reduces fluid and electrolyte loss. Onset: 30-60min. Peak: 2.5hrs (solution), 4-5hrs. (Capsules) Duration: 4-5hrs. Indications: Acute Diarrhea; Chronic Diarrhea Norm. Dosage, Freq, Route, Range: PO 4mg followed by 2mg after each unformed stool Max: 16mg/day Side Effects: Toxic megacolon, abdominal pain or discomfort, constipation Nursing Considerations: monitor fluid and electrolyte balance, record number and consistency of stools
Page 36 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
21. Beta-Blockers 1.78. Atenolol (Tenormin) Class: Beta-Adrenergic Antagonist; Antihypertensive Actions: reduces rate & force of cardiac contractions (negative inotropic action); cardiac output is reduced as well as systolic and diastolic BP. Decreases peripheral vascular resistance both at rest and with exercise. Peak: 2-4hr. Duration: 24hr. Half-life: 6-7hr. Indications: management of hypertension as a single agent or concomitantly w/ other antihypertensive agents, especially a diuretic, and in treatment of stable angina pectoris, MI Norm. Dosage, Freq, Route, Range: PO 25-50mg/day, may increase to 100mg/day Max: 100mg/day Side Effects: Bradycardia, hypotension, CHF, pulmonary edema, nausea, vomiting Nursing Considerations: Measure trough BP, check apical pulse before ., monitor BP, monitor diabetics for loss of glycemic control
1.79. Carvedilol (Coreg, Coreg CR) Class: Alpha and Beta Adrenergic Antagonist; Antihypertensive Actions: An effective antihypertensive agent reducing BP to normotensive range and useful in managing some angina, dysrhythmias, and CHF by decreasing myocardial oxygen demand and lowering cardiac workload. Peak: Antihypertensive effect 7-14 days Indications: CHF, Left Ventricular Dysfunction, Post MI, Hypertension Norm. Dosage, Freq, Route, Range: PO start w/ 3.125mg bid Max: 50mg/day Side Effects: Dizziness Nursing Considerations: Monitor for therapeutic effectiveness, lab tests: LFTs and digoxin levels w/ concurrent use, monitor for worsening of symptoms in patients w/ PVD
1.80. Metoprolol Tartrate (Lopressor) Class: Cardioselective; Beta-adrenergic antagonist; Antihypertensive; Antianginal Actions: produces a decrease in the systolic and diastolic BPs, and reduces edema in CHF and kidney failure patients. Onset: 15min. Peak: PO 1.5hr. IV 20min. Duration: 13-19hr. Indications: management of hypertension Norm. Dosage, Freq, Route, Range: PO 50-100mg/day in 1-2 divided doses, may increase weekly up to 100-450mg/day Max: 450mg/day Side Effects: fatigue, insomnia, bradycardia, heartburn, shortness of breath Nursing Considerations: Take apical pulse and BP before istering drug. Monitor BP q12hr
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 37 of 75
Drug Med Cards
1.81. Propanolol (Inderal, InnoPran XL) Class: Beta-Adrenergic Receptor Antagonist; Antihypertensive; Class II Antiarrhythmic Actions: Nonselective beta-blocker of both cardiac and bronchial adrenoreceptors that competes w/ epinephrine and norepinephrine for available beta receptor sites. In higher doses, it depresses cardiac function including contractility and arrhythmias. Lowers both supine and standing BP in hypertensive patients. Peak: 60-90 min immediate release, 6 hr sustained release, IV 5 min Indications: Hypertension, Angina, Arrhythmias, Acute MI, Migraine Prophylaxis Norm. Dosage, Freq, Route, Range: PO 40 mg bid, usually need 160-480 mg/day Max: 480 mg/day Side Effects: confusion, fatigue, drowsiness, bradycardia, paresthesia of hands Nursing Considerations: Monitor apical pulse, respirations, BP and circulation to extremities. Be aware of adverse reactions, Lab tests: periodic hematologic, kidney, liver, and cardiac functions, monitor I&O
1.82. Sotalol (Betapace) Class: Beta-Adrenergic Antagonist; Class II and III Antiarrhythmic Actions: slows heart rate, decreases AV nodal conduction, and increases AV nodal refractoriness. Produces significant reduction in both systolic and diastolic blood pressure. Peak: 2-3 hr Duration: 24 hr Indications: Ventricular Arrhythmias, Atrial Fibrillation/Flutter Norm. Dosage, Freq, Route, Range: PO initial dose of 80 mg bid or 160 mg daily taken prior to meals, may increase every 3-4 days in 40-160 mg increments Max: 240 mg/day in 1-2 divided doses Side Effects: bradycardia, dyspnea, chest pain, palpation, fatigue, dizziness Nursing Considerations: Monitor ECG baseline and periodically, Lab tests: baseline serum electrolytes, monitor cardiac status throughout therapy, monitor patients w/ bronchospastic disease (ex: bronchitis, emphysema) for inhibition of bronchodilation, monitor diabetics for loss of glycemic control.
Page 38 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
22. Nitrates 1.83. Isosorbide Dinitrate (Dilatrate-SR, IsoBid) Class: Nitrate Vasodilator (prototype: Nitroglycerin) Actions: has an anti-anginal effect as a result of vasodilation of the coronary arteries. Onset: SL 2-5min. w/in 1hr. reg. tabs w/in 3 min. chewable tabs 30 min. sustained release tabs Duration: SL 1-2hr. Chewable tabs: 1.5-2hrs. Sustained release tabs: 6-8hrs. Indications: relief of acute anginal attacks and for management of long-term angina pectoris Norm. Dosage, Freq, Route, Range: 5-30mg q2-3hr. Max: 360mg/day Side Effects: light-headedness, flushing, headache, pallor Nursing Considerations: Monitor for effectiveness, headaches tend to decrease in intensity and frequency with continued use, may produce tolerance
1.84. Isosorbide Mononitrate (Ismo, Imdur) Class: Nitrate Vasodilator Actions: Long acting metabolite of the coronary vasodilator isosorbide dinitrate. It decreases preload as measured by pulmonary capillary wedge pressure and left ventricular end volume and diastolic pressure with a consequent reduction in myocardial oxygen consumption. Onset: 1 hr. Peak: regular release 30-60 min; sustained release 3-4 hr Duration: regular release 5-12 hr, sustained release 12 hr Indications: Prevention of Angina Norm. Dosage, Freq, Route, Range: PO regular release 20 mg bid 7 hr apart; sustained release 30-60 mg early morning, may increase up to 120 mg after several days if needed Max: 240 mg/day Side Effects: headache, anxiety, coughing, nasal congestion, dry mouth Nursing Considerations: Monitor cardiac status, frequency and severity of angina and BP, assess for S&S for toxicity, Lab tests: monitor serum electrolytes periodically.
1.85. Nitroglycerin (Nitro-Dur, Nitrostat, Nitroquick) Class: Nitrate Vasodilator Actions: Organic nitrate and potent vasodilator that relaxes vascular smooth muscle. After conversion to nitric oxide, it leads to dose-related dilation of both venous and arterial blood vessels. Promotes peripheral pooling of blood, reduction of peripheral resistance, and decreased venous return to the heart. Both left ventricular preload and afterload are reduced and myocardial oxygen consumption or demand is decreased. Onset: SL 2 min PO 3 min Ointment 30 min Duration: SL 30 min PO 3-5 hr Ointment 3-6 hr Indications: Angina Norm. Dosage, Freq, Route, Range: SL 1-2 sprays (0.4-0.8 mg) or 0.3-0.6 mg tablet q3-5min as needed Max: 3 doses in 15 min PO 1.3-9 mg q8-12 hr Ointment apply 1.5-5 cm of ointment q4-6hr Side Effects: dizziness, headache, postural hypotension, Syncope, tachycardia Nursing Considerations: Monitor BP, HR location, duration, pain
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 39 of 75
Drug Med Cards
23. ACE-Inhibitors 1.86. Lisinopril (Prinivil) Class: Antihypertensive, ACE inhibitor Actions: Lowers BP, improves cardiac output and exercise tolerance. Aldosterone is also reduced, thus permitting a potassium-sparing effect. Onset: 1 hr. Peak: 6-8hr. Duration: 24hrs. Indications: Hypertension, Heart Failure Norm. Dosage, Freq, Route, Range: (Hypertension) PO 10 mg once/day, may increase up to 20-40 mg 1-2x/day (Heart Failure) PO 5-40 mg/day Max: 80 mg/day Side Effects: Headache, dizziness, fatigue, hypotension, chest pain, nausea, vomiting, diarrhea, anorexia, constipation, intestinal angioedema, dyspnea, cough, rash, hyperkalemia, increase BUN and creatinine levels Nursing Considerations: Check BP before giving med. With pt. in supine position, monitor serum Na and K+ levels, Lab tests: WBC q month for the first 3-6 months of therapy and at periodic intervals for 1 yr.
1.87. Ramipril (Altace) Class: Angiotensin-Converting Enzyme (ACE) Inhibitor; Antihypertensive Actions: lowers BP, and improves cardiac output as well as exercise tolerance. Onset: 2hr Peak: 6-8hr Duration: up to 24hr Half-life: 2-3hr Indications: Norm. Dosage, Freq, Route, Range: PO 2.5-5mg daily, may increase up to 20 mg/day in 1-2 divided doses Max: 20mg/day Side Effects: Nursing Considerations: Monitor BP, Lab Tests: BUN and serum creatinine periodically. Observe for S&S of hyperkalemia
Page 40 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
24. Calcium Channel Blockers 1.88. Amlopidine (Norvasc) Class: Calcium Channel Blocker; Antihypertensive Actions: selectively block calcium influx across cell membranes of cardiac and vascular smooth muscle without changing serum calcium concentrations. Peak: 6-9 hr. Duration: 24 hr. Indications: Hypertension, Stable/Vasospastic Angina Norm. Dosage, Freq, Route, Range: PO 5-10 mg once daily Max: 10 mg Side Effects: peripheral and facial edema, headache Nursing Considerations: Monitor BP & HR, monitor for S&S of peripheral and facial edema, monitor BP with postural changes
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 41 of 75
Drug Med Cards
25. Central Acting Antihypertensive 1.89. Clonidine (Catapres) Class: Central-Acting Antihypertensive; Analgesic Actions: Decreases systolic and diastolic BP and HR. Reportedly minimizes or eliminates many of the common clinical S&S associated w/ withdrawal of heroin, methadone, or other opiates. Onset: PO 3060min. Peak: PO 2-4hr. Duration: PO 8hr. Indications: Hypertension, ADHD, Severe Pain Norm. Dosage, Freq, Route, Range: PO 0.1mg Max: 2.4mg/day Side Effects: Hypotension, dry mouth, drowsiness, sedation, constipation Nursing Considerations: Monitor BP closely, monitor I&O during period of dosage adjustment
1.90. Guanfacine HCL (Intuniv, Tenex) Class: Alpha-Adrenergic Agonist; Central-Acting Antihypertensive Actions: In cerebral cortex, stimulation of alpha2-adrenoreceptors triggers inhibitory neurons to reduce central sympathetic outflow (ie., impulses from vasomotor center to heart * blood vessels) Onset: 2hr.; 6hr. ER Peak: 6hr. Duration: Up to 24hr. Indications: Hypertension; Attention Deficit Hyperactivity Disorder (ADHD) Norm. Dosage, Freq, Route, Range: PO 1mg/day titrate up (Normal range: 1-4mg/day) Side Effects: dizziness, sedation, fatigue, dry mouth, constipation, impotence Nursing Considerations: do not d/c abruptly, may cause plasma & urinary catecholamine increases leading symptoms of tachycardia, insomnia, anxiety, nervousness; monitor BP until stabilized; assess mental status & alertness; employ measure to keep mouth moist; avoid alcohol & do not self-medicate w/ OTC drugs
Page 42 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
26. Antihypertensives 1.91. Losartan (Cozaar) Class: Angiotensin II Receptor Antagonist; Antihypertensive Actions: Antihypertensive effect is due to vasodilation and inhibition of aldosterone effects on sodium and water retention. Peak: 6hr. Duration 24hr. Indications: Hypertension Norm. Dosage, Freq, Route, Range: PO 25-52mg in 1-2 divided doses Max: 100mg/day Side Effects: dizziness, dyspepsia, insomnia, headache Nursing Considerations: Monitor BP at drug trough, lab tests: monitor CBC, electrolytes, liver and kidney functions w/ long-term therapy
1.92. Valsartan (Diovan) Class: Renin Angiotensin System Antagonist; Antihypertensive Actions: Blocks angiotensin II receptors results in vasodilation as well as decreasing the aldosteronesecreting effects of angiotensin II. These actions result in the antihypertensive effect of valsartan. Onset: BP decreased in 2 weeks. Peak: Plasma levels, 2-4hr; BP effect 4 weeks Indications: Hypertension, Heart Failure Norm. Dosage, Freq, Route, Range: PO 40-80mg daily Max: 320mg/day Side Effects: headache, dizziness, nausea, vomiting Nursing Considerations: monitor BP, lab tests: periodic LFTs, BUM, and creatinine, serum potassium, and CNC w/ differential
1.93. Terazosin (Prazosin) Class: Alpha-Adrenergic Receptor Antagonist, Antihypertensive Actions: Selectively blocks Alpha1-adrenergic receptors in vascular smooth muscle in many tissues, including vascular smooth muscle, the bladder neck, and the prostate. Promotes vasodilation, thus producing relaxation that leads to reduction of peripheral vascular resistance and lowers BP as well as increased urine flow. Peak: 1-2 hr. Indications: Hypertension, Benign Prostatic Hypertrophy Norm. Dosage, Freq, Route, Range: PO start with 1 mg at bedtime, then 1-5 mg/day Max: 20 mg/day Side Effects: Asthenia (weakness), dizziness, headache, 1st –dose phenomenon syncope Nursing Considerations: Monitor BP, be alert for possible 1st –dose phenomenon
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 43 of 75
Drug Med Cards
27. Antipsychotics 1.94. Aripiprazole (Abilify) Class: Atypical Antipsychotic; Dopamine System Stabilizer Actions: combination of partial agonist activity at D2 and 5-HT1A receptors and antagonists activity at 5HT2A receptors. Peak: 3-5hrs. Indications: Schizpphrenia; Bipolar Mania; Agitation associated w/ Schizophrenia/Bipolar; Adjunct in Major Depression; Irritability associated w/ Autism Norm. Dosage, Freq, Route, Range: PO 10-15mg once daily, may increase at 2wk intervals to Max: 30mg/day Side Effects: headache, insomnia, light-headedness, somnolence, akathisia, risk of stroke in elderly w/ dementia-related-psychosis, N&V, constipation Nursing Considerations: monitor cardiovascular status, Lab tests: periodic Hct and Hbg, and blood glucose, monitor for elevated K and myoglobinuria if NMS is suspected.
1.95. Asenapine (Saphris) Class: Atypical Antipsychotic; Serotonin Antagonist; Antimanic; Antidepressant Actions: thought to be related to antagonism to certain CND dopamine (D2) and serotonin (5-HT2a) receptors. Peak: 0.5-1.5hr. Indications: Schizophrenia; Bipolar Disorder Norm. Dosage, Freq, Route, Range: SL 5mg bid Side Effects: Extrapyramidal symptoms (EPS), headache, somnolence, insomnia Nursing Considerations: monitor BP, HR, and weight; monitor for orthostatic hypotension; monitor diabetes
1.96. Atomoxetine (Strattera) Class: Miscellaneous Psychotherapeutic Actions: Selective inhibition of the presynaptic norepinephrine transporter, resulting in norepinephrine reuptake inhibition. Peak: 1-2hr. Indications: Attention Deficit Hyperactivity Disorder (ADHD) Norm. Dosage, Freq, Route, Range: PO start w/ 40mg in a.m., may increase after 3 days to target dose of 80mg/day given either in a.m. or divided dose. May increase to 100mg/day if needed. Side Effects: headache, insomnia, suicidal ideation, upper abdominal pain, nausea, vomiting, decreased appetite, severe liver failure, and cough Nursing Considerations: evaluate therapeutic effectiveness; report increased aggression & irritability as there may indicate need to d/c the drug; monitor children & adolescence for behavior changes that may indicate suicidal ideation; monitor cardiovascular status especially w/ preexisting hypertension; monitor HR & BP at baseline, following a dose increase, and periodically during therapy; Lab tests: periodic LFTs
Page 44 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.97. Chlorpromazine (Thorazine) Class: Antipsychotic; Phenothiazine; Antiemetic Actions: mechanism thought to be related to blockade of post-synaptic dopamine receptors in the brain. Onset: 30-60min. Peak: PO 2-4hr. IM 15-20min. Duration: 4-6hr. Indications: Psychotic disorder, agitation; nausea and vomiting; dementia; intractable hiccups; tetanus Norm. Dosage, Freq, Route, Range: PO 25-100mg tid or qid, Max: 1,000mg/day IM/IV: 25-50mg Max: 600mg Side Effects: Agranulocytosis,Neuroleptic malignant syndrome (NMS), hypothermia,adynamic ileus, sedation, extrapyramidal symptoms (EPS) Nursing Considerations: Lab tests: LFTs, periodic CBC w/ diff, and blood glucose, monitor cardiac status, be alert for NMS and report immediately, report EPS, monitor BP frequently, may cause pink to red-brown discoloration of urine, have pt. wear protective clothing and sunscreen when outdoors, have pt. practice meticulous oral hygiene to prevent oral candidiasis
1.98. Clozapine (Clozaril) Class: Atypical Antipsychotic Actions: Interferes w/ binding of dopamine to D1 and D2 receptors in the limbic region of the brain. Onset: 2-4 wk. Peak: 2.5 hr. Indications: Schizophrenia Norm. Dosage, Freq, Route, Range: PO initiate 12.5mg daily or bid and increase by 25-50mg/day and titrate to a target of 350-400mg/day in 3 divided doses Max: 900mg/day Side Effects: tachycardia, agranulocytosis, transient fever, neuroleptic malignant syndrome (NMS), increased mortality from severe hematologic, cardiovascular, and respiratory adverse effects. Nursing Considerations: Lab tests: baseline WBC and absolute neutrophil count must be made before initial treatment q wk. for first 6 mon. then q2wk.for the next 6 mon. then q4wk.periodic blood glucose, monitor cardiovascular and respiratory status,
1.99. Fluphenazine HCL (Prolixin) Class: Antipsychotic; Phenothiazine Actions: thought to be related to blockade of post-synaptic dopamine receptors in the brain. Onset: 1hr. Peak: 0.5hr. Duration: 6-8hr. Indications: Psychosis; Dementia Behavior Norm. Dosage, Freq, Route, Range: PO 0.5-10mg/day in 1-4 divided doses Max: 20mg/day Side Effects: extrapyramidal symptoms (EPS), tardive dyskinesia, impaired thermoregulation, leukopenia, agranulocytosis, photosensitivity Nursing Considerations: report any EPS or mental depression, Lab tests: periodic WBC w/ diff, LFTs, monitor renal function and notify prescriber if BUN is elevated, have pt. wear protective clothing and sunscreen when outdoors, may discolor urine pink to red or reddish brown
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 45 of 75
Drug Med Cards
1.100. Haloperidol (Haldol) Class: Antipsychotic, Butyrophenone Actions: Blocks postsynaptic dopamine receptors in the limbic system of the brain. ↓ in dopamine neurotransmission has been correlated w/ its higher instance of extrapyramidal effects. ↓ Psychotic manifestations & exerts strong antiemetic effect. Onset: IM 30-45min. Peak: PO 2-6hr., IM 10-20min. Indications: Management of manifestations of psychotic disorders & for control of tics & vocal utterances of Tourette’s syndrome, for treatment of agitated state is acute and chronic psychoses. Norm. Dosage, Freq, Route, Range: PO 0.2-5 mg bid or tid Max: 15 mg.day IM 2-5 mg q4hr PRN Max: 30 mg/day Side Effects: extrapyramidal reactions, tardive dyskinesia, agitation, drowsiness, lethargy, fatigue, tremor, ataxia, headache, confusion, vertigo, tachycardia Nursing Considerations: monitor for drug effectiveness (long half-life), monitor patients’ mental status daily, be alert for behavioral changes
1.101. Iloperidone (Fanapt) Class: Atypical Antipsychotic Actions: is both a dopamine (D2) and serotonin (5-HT2) antagonist. Peak: 2-4hr. Indications: Schizophrenia Norm. Dosage, Freq, Route, Range: PO initial 1mg big, then titrated to 6-12mg bid Side Effects: dizziness, somnolence, tachycardia Nursing Considerations: monitor for suicidal ideation, monitor BP, HR, and weight, monitor for orthostatic hypotension, Lab tests: baseline and periodic CBC w/ diff
1.102. Lithium Carbonate (Eskalith, Lithane, Lithobid, Lithonate, Lithotabs) Class: Antipsychotic; Mood Stabilizer Actions: The lithium ions behaves in the body much like the sodium ion: but its exact mechanism of action is unclear. Peak: 0.5-3hrs. Indications: Mania Norm. Dosage, Freq, Route, Range: PO: Loading Dose 600mg tid or 900mg sustained release bid or 30mL of solution tid PO: Maintenance Dose 300mg tid or qid or 15-20mL solution in 2-4 divided dose Max: 2.4g/day Side Effects: headache, lethargy fatigue, recent memory loss, peripheral circulatory collapse, nephrogenic diabetes insipidus, nausea, vomiting, anorexia, abdominal pain, diarrhea, dry mouth, fine, hand tremors, muscle weakness, reversible leukocytosis Nursing Considerations: Lab tests: periodic lithium levels; periodic thyroid function tests; monitor for S&S of lithium toxicity; be alert to and report symptoms of hypothyroidism; drink plenty of liquids (2-3L/day)during stabilization and at least (1-1.5L/day) during ongoing therapy
Page 46 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.103. Lurasidone (Latuda) Class: Atypical Antipsychotic Actions: the mechanism of action is unknown but the efficacy of lurasidone in schizophrenia is thought to be mediated through central dopamine type 2 (D2) and serotonin Type 2 (5HT2a) receptor antagonism. Indications: Schizophrenia Norm. Dosage, Freq, Route, Range: PO 40-160mg one daily Side Effects: akathisia, dizziness, somnolence, parkinsonism, nausea Nursing Considerations: monitor orthostatic VS, Lab tests: periodic blood glucose, lipid profile, LFTs, and CBC w/ diff, monitor closely pts. w/ neutropenia, monitor weight, monitor for and report promptly seizure activity, S&S of Neuroleptic Malignant Syndrome (NMS) or tardive dyskinesia
1.104. Olanzapine (Zyprexa) Class: Atypical Antipsychotic Actions: thought to be due to antagonism for both serotonin 5-HT2A/2C and dopamine D1-4 receptors. Peak: 6hr. Indications: Psychotic disorders; Bipolar Mania; Acute Agitation Norm. Dosage, Freq, Route, Range: PO start w/ 5-10mg/day, may increase by 2.5-5mg q wk. until desired response Max: 20mg/day Side Effects: weight gain, somnolence, dizziness, agitation, insomnia, headache, nervousness, hostility, Parkinsonism Nursing Considerations: monitor cerebrovascular status closely, Lab tests: periodically monitor ALT, blood glucose, monitor BP and HR periodically and monitor temp.
1.105. Paliperidone (Invega) Class: Atypical Antipsychotic Actions: Interferes w/ binding of dopamine to dopamine type 2 (D2) receptors, serotonin (5-HT2a) receptors and alpha-adrenergic receptors. Peak: 24hrs Indications: Schizophrenia; Schizoaffective Disorder Norm. Dosage, Freq, Route, Range: PO initially 6mg/day, may adjust up/down in 3mg increments Max: 12mg/day Side Effects: Akathisia, headache, somnolence Nursing Considerations: Baseline ECG is recommended to rule out congenital long-QT syndrome; Lab tests: baseline and periodic serum electrolytes, periodic blood glucose, and CBC; monitor diabetes and loss of glycemic control
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 47 of 75
Drug Med Cards
1.106. Prochlorperazine Meleate (Compazine) Class: Antipsychotic; Phenothiazine, Antiemetic Actions: Strong antipsychotic effects thought to be due to blockade of postsynaptic dopamine receptors in the brain. Antiemetic effect is produced by suppression of the chemoreceptor trigger zone (CTZ). Onset: PO 30-40 min, PR 60 min, IM 10-20 min Duration: PO 3-4 hr, Sustained Release PO 10-12 hr, PR 3-4 hr, IM up to 12 hr Indications: Severe Nausea/Vomiting, Psychotic Disorders Norm. Dosage, Freq, Route, Range: PO 5-10 mg 3-4 times/day, Sustained Release PO 10-15 mg q 12 hr PR 25 mg bid IM 5-10 mg q3-4hr up to 40 mg/day IV 2.5-10 mg q3-4hr Max: 40 mg/day Side Effects: drowsiness, extrapyramidal reactions (akathisia, dystonia or parkinsonism) Nursing Considerations: position carefully to prevent aspiration, Lab tests: periodic CBC with diff in longterm therapy, be alert of high core temperature
1.107. Quetiapine (Seroquel) Class: Atypical Antipsychotic Actions: effectiveness indicated to a reduction in psychotic behavior. Peak: 1.5hr. Half-life: 6hrs. Indications: management of schizophrenia, maintenance of acute bipolar disorder, and add-on therapy for major depressive disorder Norm. Dosage, Freq, Route, Range: 25-50mg dose and increase by 25-50mg/day Max: 800mg/day Side Effects: dizziness, headache, somnolence, leukopenia Nursing Considerations: Monitor for respiratory depression in patients with chronic respiratory insufficiency and suicidal tendencies
1.108. Risperidone (Risperdol) Class: Atypical Antipsychotic Actions: interferes w/ binding of dopamine to D2-interlimbic region of the brain, serotonin (5-HT2) receptors, and alpha-adrenergic receptors in the occipital cortex. Onset: therapeutic effect 1-2 wk. Peak: 12hr. Indications: Schizophrenia; Bipolar Disorder; Irritability Associated w/ Autism Norm. Dosage, Freq, Route, Range: PO 1-2mg/day in 1 or 2 doses then titrate up Max: 8mg/day Side Effects: sedation, drowsiness, headache, insomnia, agitation, extrapyramidal symptoms (EPS), neuroleptic malignant syndrome (NMS) Nursing Considerations: monitor cardiovascular status closely, Lab tests: monitor periodically blood glucose, serum electrolytes, LFTs, and CBC, be aware of risk for orthostatic hypotension
Page 48 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.109. Thioridazine HCL (Mellaril) Class: Antipsychotic; Phenothiazine Actions: blocks post-synaptic dopamine receptors in the mesolimbic system of the brain. Onset: days to weeks Indications: Psychotic disorders; moderate to marked depression; dementia behavior Norm. Dosage, Freq, Route, Range: PO 50-100mg tid Max: 800mg/day Side Effects: sedation, paralytic ileus, urinary retention Nursing Considerations: monitor I&O ratio and bowel elimination pattern, orthostatic hypotension may occur, Lab tests: obtain periodic CBC and LFTs during therapy, avoid alcohol, may cause pink-red to reddish-brown urine
1.110. Trifluoperazine HCL (Stelazine) Class: Antipsychotic; Phenothiazine Actions: thought to be related to blockade of post-synaptic dopamine receptors in the brain. Onset: Rapid Peak: 2-3hr. Duration: up to 12hr. Indications: Schizophrenia; Anxiety Norm. Dosage, Freq, Route, Range: PO 1-2mg bid Max: 20mg/day Side Effects: drowsiness, extrapyramidal symptoms (EPS), neuroleptic malignant syndrome (NMS), dry mouth, hypotension Nursing Considerations: monitor HR and BP, monitor I&O ratio and bowel elimination pattern, Lab tests: periodic CBC and serum prolactin, cover as much skin surface as possible with clothing when you must be in direct sunlight, urine may be discolored or reddish-brown
1.111. Ziprasidone HCL (Geodon) Class: Atypical Antipsychotic Actions: exerts antischizophrenic effects through dopamine (D2) and serotonin (5-HT2a) receptors antagonism. Peak: 6-8hrs. Indications: Schizophrenia; Acute episodes of Agitation/Acute psychosis, Acute Mania/Bipolar Disorder Norm. Dosage, Freq, Route, Range: PO start w/ 20mg bid w/ food, may increase q2days up to 80mg bid if needed Max: 160mg/day Side Effects: somnolence, nausea Nursing Considerations: Lab tests: baseline and periodic ECGs, serum potassium and serum magnesium, periodically monitor blood glucose, monitor I&O ratio and pattern, monitor BP, monitor cognitive status, monitor for loss of seizure control, avoid strenuous exercise, exposure to extreme heat, or other activities that may cause dehydration
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 49 of 75
Drug Med Cards
28. Anti-Coagulants 1.112. Enoxaparin (Lovenox) Class: Anticoagulant; Low Molecular Weight Heparin Actions: An effective anticoagulation agent, if is used for prophylactic treatment as an antithrombotic agent following certain types of surgery. Peak: 3 hr. Duration 4-6 hr. Indications: Prevention of DVT after Hip or Knee Surgery, Prevention of DVT after Abdominal Surgery, Treatment of DVT and Pulmonary Embolus, Non-Q Wave MI Acute STEMI Norm. Dosage, Freq, Route, Range: SQ 30 mg bid for 10-14 days starting 12-24 hr post-surgery Max: 60 mg/day Side Effects: Dyskinesia, Hyperkinesia, Nausea, Diarrhea, Urine discoloration Nursing Considerations: Monitor carefully for hyperpyrexia, confusion, or emergence of Parkinson’s S&S during drug w/drawal, monitor for orthostatic hypotension and worsening of dyskinesia, or hyperkinesia, Lab tests: Hgb and serum ferritin levels w/ prolonged therapy
1.113. Heparin (Heparin Sodium) Class: Anticoagulant Actions: Has rapid anticoagulant effect, does not lyse already existing thrombi but may prevent their extension & propagation. Onset: SQ 20-60min. Peak: in min. Duration: SQ 8-12hr. IV 2-6hr. Indications: prophylaxis and treatment of venous thrombosis and pulmonary embolism & to prevent thromboembolic complications arising from cardiac & vascular surgery, frostbite, & curing acute stage of MI Norm. Dosage, Freq, Route, Range: IV 5,000 units bolus dose then 20,000-40,000 units infused over 24hr, dose adjusted to maintain desired aPTT or 5,000-10,000 units IV piggyback q4-6 hr Max: 60,000 units/day SQ 10,000-20,000 units/m2/24hr Side Effects: spontaneous bleeding, fever, chills, numbness, elevated BP, headache Nursing Considerations: Lab tests: baseline blood coag., Hct, Hgb, RBC, & platelet count prior to ., monitor aPTT levels closely, blood draw for coag. test 30 min before each scheduled SQ or intermittent IV dose, observe all needle sites daily, monitor vital signs
Page 50 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
29. Antiplatelets 1.114. Aspirin (ASA) Class: Non-narcotic, Antiplatelet, Antipyretic Actions: inhibiting the formation of prostaglandins involved in the production of inflammation, pain and fever, powerfully inhibits platelet aggregation. High serum salicylate concentrations can impair hepatic synthesis of blood coagulation factors VII, IX, X. Peak: 15min-2hr. Indications: Anti-inflammatory action, pain, fever reducer, antiplatelet Norm. Dosage, Freq, Route, Range: PO: 350-650 mg q4h Max: 4 g/day Side Effects: Bronchospasm, anaphylactic shock (laryngeal edema), nausea, heartburn, stomach pains, thrombocytopenia, hemolytic anemia Nursing Considerations: Allergy to any ASA, monitor for salicylate toxicity. In adults, a sensation of fullness in the ears, tinnitus, and decreased or muffled hearing are the most frequent symptoms.
1.115. Clopidogrel (Plavix) Class: Antiplatelet Actions: prolongs bleeding time, thereby reducing atherosclerotic events in high-risk patients. Onset: 2hr. reaches steady state in 3-7 days Half-life: 8hr. Indications: acute coronary syndrome (ST or non-ST elevations). Secondary of MI, stroke, and vascular death Norm. Dosage, Freq, Route, Range: PO 75mg/day Max: 75mg/day Side Effects: fatigue, back pain, diarrhea, nausea, headache, dizziness Nursing Considerations: Monitor for S&S of GI bleeding. Lab tests: platelet count, and lipid profile
1.116. Dipyridamole (Apo-Dipyridamole) Class: Antiplatelet; Platelet Aggregate Inhibitor Actions: Nonnitrate coronary vasodilator that increase coronary blood flow by selectively dilating coronary arteries, thereby increasing myocardial oxygen supply. Peak: 45-150 min. Indications: Prevention of thromboembolism in cardiac valve replacement, Thromboembolic Disorders, Thallium Stress Test Norm. Dosage, Freq, Route, Range: PO 150-400 mg/day in divided doses Max: 400 mg/day Side Effects: headache, dizziness, faintness, syncope, weakness Nursing Considerations: monitor therapeutic effectiveness
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 51 of 75
Drug Med Cards
30. Proton Pump Inhibitor 1.117. Omeprazole (Prilosec, Prilosec OTC) Class: Proton Pump Inhibitor (PPI); Antisecretory Actions: Suppresses gastric acid secretion relieving gastrointestinal distress and promoting ulcer healing. Onset: 0.5-3.5hr. Peak: 5 days Indications: GERD, Duodenal Ulcer, Erosive Esophagitis, Hyper secretory disease, gastric ulcer Norm. Dosage, Freq, Route, Range: PO 20-40mg once/day for 4-8 weeks Max: 360mg/day Side Effects: headache, dizziness, fatigue, diarrhea, abdominal pain, nausea Nursing Considerations: Lab tests: monitor urinalysis for hematuria and proteinuria, periodic LFTs w/ prolonged use.
1.118. Pantoprazole (Protonix) Class: Gastric Proton Pump Inhibitor; Antisecretory Actions: suppresses gastic acid secretion by inhibiting the acid (proton H+) pump in the parietal cells. Peak: 2-4hrs. Indications: short-term treatment of erosive esophagitis associated w/ gastroesphageal reflux disease (GERD), hyper secretory Norm. Dosage, Freq, Route, Range: PO 40mg daily for 7-10days Max: 40mg/day Side Effects: diarrhea, flatulence, abdominal pain, headache, insomnia, rash Nursing Considerations: Lab tests: Urea breath test 4-6 wks after completion of therapy. Monitor for severe skin reaction
Page 52 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
31. H2- Receptor Antagonist 1.119. Famotidine (Pepcid) Class: Antisecretory (H2-Receptor Antagonist) Actions: reduces parietal cell output if hydrochloric acid; thus, detrimental effects of acid on gastric mucosa are diminished. Onset: 1hr Peak: 1-3hr Duration: 10-12hr Indications: short-term treatment of active duodenal ulcer, GERD, gastritis Norm. Dosage, Freq, Route, Range: PO 40mg at bedtime or 20mg bid IV 20 mg q12hr. Max: 40mg/day Side Effects: dizziness, headache, confusion, depression, constipation, diarrhea Nursing Considerations: Monitor for improvement in GI distress. Monitor for signs of GI bleeding. Be aware that pain relief may not be experience for several days.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 53 of 75
Drug Med Cards
32. Cerebral Stimulant 1.120. Amphetamine Sulfate (Adderall) Class: Cerebral Stimulant; Anorexiant Actions: Marked stimulant effect on CNS thought to be due to action on cerebral cortex & possibly the reticular activating system. Acts indirectly on adrenergic receptors by increasing synaptic release of norepinephrine in the brain & by blocking reuptake of norepinephrine at the presynaptic membrane. Peak: 1-5hr. Duration: Up to 10hr. Indications: Narcolepsy; Attention Deficit Disorder (ADD) Norm. Dosage, Freq, Route, Range: PO 10mg ER once daily in a.m.; may increase by 5-10mg at weekly intervals if need to max of 30mg/day Side Effects: Sudden death; irritability; restlessness; insomnia; euphoria; palpitation Nursing Considerations: Monitor S&S of toxicity in children; monitor for S&S of insomnia or anorexia; monitor BP & HR; monitor diabetic closely; monitor growth in children; meticulous oral hygiene is required because of decreased saliva; rinse mouth frequently with clear water; avoid caffeine-containing beverages because caffeine increase amphetamine effects; taper drug on withdrawal
1.121. Methylphenidate HCL (Ritalin, Focalin, Concerta) Class: Cerebral Stimulant Actions: Acts mainly on cerebral cortex exerting stimulant effect. Peak: 1.9hr. 4-7hr. sustained release, 2hr. transdermal Duration: 3-6hr., 8 hr. sustained release Indications: Narcolepsy; Attention Deficit Disorder (ADD) Norm. Dosage, Freq, Route, Range: PO immediate release products 20-30mg/day in divided doses Concerta extended release 18-36mg/day Side Effects: nervousness, insomnia, exfoliative dermatitis Nursing Considerations: Monitor BP & pulse at appropriate intervals; Lab tests: obtain periodic CBC w/ diff & platelet counts during prolonged therapy; monitor closely pt. w/ history of alcoholism; supervise drug withdrawal; check weight at least 2-3 times weekly & report weight loss; check height & weight in children, failure to gain in either should be reported to prescriber; w/hold patch from an ADHD child who exhibits anxiety, tension, or agitation & consult prescriber
Page 54 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
33. Antihistamines 1.122. Diphenhydramine (Benadryl) Class: Centrally acting cholinergic antagonist, Antihistamine, h1-receptor antagonist Actions: suppresses central cholinergic activity and prolongs action of dopamine by inhibiting its reuptake and storage. Onset: 15-30 min. Peak: 1-4hr. Duration: 4-7hr. Indications: temporary symptomatic relief of various allergic conditions and to treat or prevent motion sickness, vertigo, and reactions to blood or plasma in susceptible patients Norm. Dosage, Freq, Route, Range: PO 25-50mg tid or qid Max: 300mg/day IV/IM 10-50mg q4-6hr Max: 400mg/day Side Effects: drowsiness, tachycardia, dry mouth Nursing Considerations: supervise ambulation, monitor cardiovascular status, do not use with alcohol and other CNS depressants, increase fluid intake
1.123. Hydroxyzine HCL (Atarax) Class: Antihistamine, H1-receptor antagonist Actions: H1 receptor antagonist blocks histamine. Onset: PO 15-30min. Duration: 4-6hrs. Indications: Anxiety; Pruritus; Nausea Norm. Dosage, Freq, Route, Range: PO 50-100mg tid IM 50-100mg q4-6hrs. Side Effects: drowsiness, dizziness, headache, hypotension, urticarial, dyspnea, chest tightness, wheezing, involuntary motor activity Nursing Considerations: reduce if CNS depressants are prescribed concomitantly, monitor oral membranes, alertness and drowsiness
1.124. Hydroxyzine Pamoate (Vistaril) Class: Antihistamine, H1-receptor antagonist Actions: H1 receptor antagonist blocks histamine. Onset: PO 15-30min. Duration: 4-6hrs. Indications: Anxiety; Pruritus; Nausea Norm. Dosage, Freq, Route, Range: PO 50-100mg tid IM 50-100mg q4-6hrs. Side Effects: drowsiness, dizziness, headache, hypotension, urticarial, dyspnea, chest tightness, wheezing, involuntary motor activity Nursing Considerations: reduce if CNS depressants are prescribed concomitantly, monitor oral membranes, alertness and drowsiness
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 55 of 75
Drug Med Cards
1.125. Promethazine (Phenergan) Class: Antihistamine, Antiemetic, Antivertigo Actions: Long-acting derivative of phenothiazine with marked antihistamine activity and prominent sedative, amnesic, and anti-motion sickness actions. Onset: PO/PR/IM 20 min IV 5 min Duration: 2-8 hr Indications: Motion sickness, nausea, pruritus sedation Norm. Dosage, Freq, Route, Range: PO/PR 25mg q12hr Max: 50mg Side Effects: drowsiness, blurred vision, dry mouth Nursing Considerations: supervise ambulation, monitor respiratory function, drug may suppress cough reflex and cause thickening of bronchial secretions
Page 56 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
34. Antidiabetic 1.126. Glipizide (Glucotrol) Class: Antidiabetic, Sulfonylurea Actions: It lowers blood glucose level by stimulating pancreatic beta cells. Glipizide improves postprandial glycemic control. Onset: 15-30 min. Peak: 1-2 hr. Duration up to 24 hr. Indications: Adjunct to diet for control of hyperglycemia in patient with type 2 diabetes mellitus. Norm. Dosage, Freq, Route, Range: PO: 2.5-5 mg/day 30 min. before breakfast, may increase by 2.5-5 mg q1-2 wk; greater than 15mg/day in divided doses before morning and evening meals Max: 40 mg/day Side Effects: hypoglycemia, anorexia, nausea, epigastric discomfort, heartburn, diarrhea, allergic skin reactions Nursing Considerations: Observe for early signs of hypoglycemia, lab tests: monitor fasting and postprandial blood glucose, and periodic HgbA1C, LFTs, electrolytes and serum osmolarity, must be made aware of the potential for hypoglycemia responses.
1.127. Glyburide (DiaBeta, Glynase) Class: Antidiabetic; Sulfonylurea Actions: One of the most potent of the 2nd generation sulfonylurea hypoglycemic agents. Appears to lower blood sugar concentration in both diabetic and nondiabetic individuals by sensitizing pancreatic beta cells to release insulin in the presence of elevated serum glucose levels. Onset: 15-60min. Peak: 1-2hr. Duration: up to 24hr. Half-life: 10hr. Indications: adjunct to diet and exercise to lower blood glucose in patients with type 2 diabetes mellitus. Norm. Dosage, Freq, Route, Range: PO 1.25mg-5mg/day, may increase by 2.5-5mg q1-2wk; greater than 15mg/day should be given in divided doses with morning and evening meal Max: 20mg/day Side Effects: hypoglycemia, nausea, vomiting, blurred vision Nursing Considerations: Monitor blood glucose levels carefully, monitor at regular intervals: Fasting and postprandial blood glucose, HbA1C, and LFTs.
1.128. Insulin (Regular) (Humulin R, Novolin R) Class: Antidiabetic, short-acting insulin Actions: Lowers blood glucose levels by increasing peripheral glucose uptake and by inhibiting the liver from changing glycogen to glucose. Onset: 0.5-1hr. Peak: 2-4hr. Duration: 5-7hrs. Indications: Emergency treatment of diabetic ketoacidosis or coma, to initiate therapy in patient w/ insulindependent diabetes, an in combo w/ inter.-acting or long-acting insulin to provide better control of blood glucose concentration. Norm. Dosage, Freq, Route, Range: SQ 5-10 units 30-60 min a.c and at bedtime (dose adjustments based on blood glucose determinations) Side Effects: hypoglycemia, nausea, palpitation, profuse sweating, hunger, tremulousness, weakness, fatigue, numb mouth and tongue Nursing Considerations: lab tests: periodically monitor fasting and postprandial blood glucose and HbA1C, test urine for ketones in new, unstable & Type 1 diabetes, if patient lost weight, exercises
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 57 of 75
Drug Med Cards vigorously, or has an illness, whenever blood glucose is substantially elevated (Onset: 0.5-1 hr. Peak: 2-4 hr. Duration: 5-8 hr.)
1.129. Insulin (NPH) (Humulin N, Novolin N) Class: Antidiabetic, Intermediate-acting insulin Actions: Controls post-pyramidal hyperglycemia, usually w/o supplemental doses of insulin injection. Onset: 1-2hr. Peak: 4-12hrs. Duration: 18-24hrs. Indications: Used to control hyperglycemia in the diabetic patient. Norm. Dosage, Freq, Route, Range: SQ 5-10 units 30-60 min a.c and at bedtime (dose adjustments based on blood glucose determinations) Side Effects: hypoglycemia, nausea, palpitation, profuse sweating, hunger, tremulousness, weakness, fatigue, numb mouth and tongue Nursing Considerations: lab tests: periodically monitor fasting and postprandial blood glucose and HbA1C, test urine for ketones in new, unstable and Type 1 diabetes, if patient lost weight, exercises vigorously, or has an illness, whenever blood glucose is substantially elevated (Onset: 1-2 hr. Peak: 4-12 hr. Duration: 10-18hr.)
1.130. Insulin Detemir (Levemir) Class: Antidiabetic; Long-acting insulin Actions: effective as a glucose-lowering agent, w/ glycemic control equivalent to that of NPH insulin. Peak: 6-8hrs. Indications: treatment of diabetes mellitus Norm. Dosage, Freq, Route, Range: SQ 0.1-0.2units/kg daily in evening or 10units daily or bid in evenly spaced doses Side Effects: hypoglycemia, weight gain, allergic reactions, rash Nursing Considerations: Monitor for S&S of hypoglycemia. Periodic fasting blood glucose and HbA1C, serum potassium with concurrent potassium-lowering drugs
1.131. Insulin Glargine (Lantus) Class: Antidiabetic long-acting insulin Actions: Lowers blood glucose levels over an extended period of time. It also prevents the conversion of glucagon to glucose in the liver. Onset: 3-4hrs. Duration: 10.4-24hrs. Indications: Bedtime dosing of adults and children w/ type 1 diabetes, or adults w/ type 2 diabetes Norm. Dosage, Freq, Route, Range: SQ for Type 1: if not taking insulin, give 10 units at same time each day (usually at bedtime) once daily, adjust based on patient need and concurrent medication SQ Type 2: if already taking oral hypoglycemic drugs, start w/ 10 units at same time each day (usually at bedtime) once daily and adjust according to patient’s need Side Effects: hypoglycemia, hypokalemia, injection site reaction Nursing Considerations: monitor for S&S of hypoglycemia, lab tests: periodically monitor fasting and postprandial blood glucose and HbA1C (Onset: 2-8 hr. Peak: none Duration: 5-24 hr.)
Page 58 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.132. Insulin Lispro (Humalog) Class: Antidiabetic; Rapid-Acting Insulin Actions: It lowers blood glucose levels and inhibits liver from changing glycogen to glucose. Onset: less than 15 minutes Peak: 0.5-1hr Duration: 3-4hr. Indications: Diabetes Mellitus Norm. Dosage, Freq, Route, Range: SQ 5-10 units 0-15min before meals (dose adjustments based on blood glucose determinations) Side Effects: hypoglycemia, hypokalemia, injection site reaction Nursing Considerations: monitor for S&S of hypoglycemia, lab tests: periodically monitor fasting and postprandial blood glucose and HbA1C
1.133. Metformin (Glucophage) Class: Antidiabetic; Biguanide Actions: Effective in lowering serum glucose level and ultimately, the HbA1C valve. Peak: 1-3hr. Half-life: 6.2-17.6hr. Indications: treatment of type 2 diabetes mellitus as adjunct to diet and exercise Norm. Dosage, Freq, Route, Range: PO start w/ 500mg daily tid or 850mg daily bid w/ meals, may increase by 500-850mg/day q1-3wk Max: 2550mg/day Side Effects: nausea, vomiting, abdominal pain, diarrhea, bitter or metallic taste, bloatedness, anorexia Nursing Considerations: Monitor vital signs and fasting and postprandial blood glucose valves, monitor cardiopulmonary status, Lab tests: baseline and periodic LFTs, kidney function tests, hematologic parameters for anemia, periodic fasting blood glucose, and HbA1C q3months.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 59 of 75
Drug Med Cards
35. Antihypoglycemic 1.134. Glucagon (Glucagen) Class: Antihypoglycemic Actions: increases blood glucose secondary to gluconeogenesis, which is the breakdown of glycogen in the liver. Onset: 5-20 min. Peak: 30 min. Duration: 1-1.5hr. Half-life: 3-10 min. Indications: hypoglycemia, radiologic studies of GI Tract Norm. Dosage, Freq, Route, Range: IM/IV/SQ 1mg may repeat q5-20min if no response for 1-2more doses Side Effects: nausea, vomiting, Stevens-Johnson syndrome Nursing Considerations: be prepared to give IV glucose if patient fails to respond to glucagon
Page 60 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
36. Anti-fungal 1.135. Metronidazole (Flagyl) Class: Antitrichomonal; Amebicide Actions: Has direct trichomonacidal and amebicial activity; exhibits antibacterial activity against obligate anaerobic bacilli, and Clostridia. Peak: 1-3 hr. Indications: Trichomoniasis, Giardiasis, Amebiasis, Pseudomembranous Colitis, Rosacea Norm. Dosage, Freq, Route, Range: PO 7.5 mg/kg q6hr. IV Loading Dose 1.5 mg/kg IV Maintenance Dose 7.5 mg/kg q6hr. Max: 4 g/day Side Effects: Candida, Nausea Nursing Considerations: Discontinue therapy immediately if symptoms of CNS toxicity develop, Monitor for seizures and peripheral neuropathy, Lab tests: obtain total and differential WBC count before, during, and after therapy, monitor S&S of sodium retention, monitor patients on lithium, report appearance of candidiasis, repeat feces exam, usually up to 3 months to ensure that amebae have been eliminated.
1.136. Ticonozole (Monistat Cream) Class: Anti-fungal Actions: spectrum antifungal that inhibits the growth of yeast (Candida Albacans) Indications: Vulvovaginal candidiasis Norm. Dosage, Freq, Route, Range: 6.5% vaginal ointment, intra vaginal x1day (one full applicator at bed time) Side Effects: mild erythema, burning, discomfort, rash, and itching Nursing Considerations: monitor for sensitization, and allergic response.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 61 of 75
Drug Med Cards
37. Eye Drops 1.137. Brimonidine Tartrate (Alphagan P) Class: Carbonic Anhydrase Inhibitor; Sulfonamide Actions: to reduce IOP and to protect the lens during surgery and laser iridotomy; to counteract effects of mydriatics and cycloplegics following surgery or, ophthalmoscopic exam Indications: Intraoperative and postsurgical increase in IOP, Open-Angle Glaucoma, Glaucoma Norm. Dosage, Freq, Route, Range: 1-2 drops per eye/day Side Effects: diminished vision in poorly illuminated areas, headache, drowsiness Nursing Considerations: Do not use in patients with Sulfa allergies
1.138. Timolol Maleate (Timoptic GTTS) Class: Beta-Adrenergic Antagonist, eye prep, miotic, antihypertensive, antuanginal Actions: GTTS: lowers elevated and normal IOP by reducing formation of aqueous humor/may increase out flow. Peak: PO 1-2hr. Topical: 1-5hrs. Indications: Chronic, open angle glaucoma, sec. glaucoma, or ocular hypertension Norm. Dosage, Freq, Route, Range: 0.25%, 0.5% one drop bid Side Effects: eye irritant, conjunctivitis, blepharitis, keratitis, superficial punctuate Nursing Considerations: √ pulse before istering oral or topical, √ BP for any extreme rates or rhythm
Page 62 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
38. Antidepressant 1.139. Bupropion HCL (Wellbutrin, Zyban, Aplenzin, Budeprion) Class: Antidepressant Actions: The neurochemical mechanisms of bupropion is not fully understood. It selectively inhibits the neuronal reuptake of dopamine. Onset: 3-4wks. Peak: 1-3hrs. Indications: Depression/Seasonal Affective Disorder Norm. Dosage, Freq, Route, Range: PO 100mg tid (immediate release) or 150mg bid (SR), or 300mg daily (XL), doses greater than 450mg/day are associated w/ an increased risk of adverse reactions including seizures Max: 300mg/day Side Effects: agitation, insomnia, dry mouth, blurred vision, headache, dizziness, tremor, nausea, vomiting, constipation. Nursing Considerations: Lab tests: periodic renal function tests and LFTs; monitor for and report delusions, hallucinations, psychotic, episodes, confusion, and paranoia; report significant restlessness, agitation, anxiety, and insomnia; monitor weight weekly; report promptly suicidal thoughts; do not take any OTC drugs w/o consulting physician.
1.140. Desvenlafaxine (Pristiq) Class: Antidepressant; Serotonin Norepinephrine Reuptake Inhibitor (SNRI) Actions: Potent inhibitor of neuronal serotonin and norepinephrine reuptake. Onset: 2wks. Peak: 1-2hrs. Duration: extensively tissue bound Indications: Depression; Anxiety Norm. Dosage, Freq, Route, Range: PO 25-125mg tid Max: 375mg/day Side Effects: increased BP & HR, dizziness, somnolence, suicidality, nausea, vomiting, dry mouth, sweating Nursing Considerations: Monitor for worsening of depression or emergence of suicidal ideation; monitor cardiovascular status periodically w/ measurements of BP & HR; Lab tests: periodic lipid profile; monitor neurologic status and report excessive anxiety, nervousness, and insomnia; monitor weight periodically and report excess weight loss; avoid using alcohol
1.141. Duloxetine (Cymbalta) Class: Antidepressant; Selective Serotonin Norepinephrine Reuptake Inhibitor (SSNRI) Actions: Causes potentiation of serotonergic and noradrenergic activity in the CNS. Antidepressant and antianxiety effects are presumed to be due to its dual inhibition of CNS presynaptic neuronal uptake of serotonin and norepinephrine, this increasing the serum levels of bith substances. Peak: 6hrs. Indications: Depression; Generalized Anxiety/Diabetic Neuropathy/Musculoskeletal Pain; Fibromyalgia Norm. Dosage, Freq, Route, Range: PO 40-60mg/day in 1-2 divided doses Side Effects: insomnia, dry mouth, constipation Nursing Considerations: Monitor for S&S of numerous drug-drug interactions; Lab tests: LFTs for unexplained abdominal pain or enlarged liver; monitor closely for and report suicidal ideation; report emergence of any of the following: anxiety, insomnia, agitation, panic attacks, irritability, hostility, psychomotor restlessness, hypomania, and mania
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 63 of 75
Drug Med Cards
1.142. Mirtazapine (Remeron) Class: Tetracyclic Antidepressant; Anxiolytic Actions: Acts as antidepressant. Effectiveness is indicated by mood elevation. Peak: 2 hr. Indications: Depression Norm. Dosage, Freq, Route, Range: PO 15mg/day in a single dose at bedtime, may increase Q1-2week Max: 45mg/day Side Effects: Somnolence, increased appetite, constipation, dry mouth Nursing Considerations: Lab tests: monitor WBC count w/ differential, lipid profile, and ALT/AST periodically, monitor for worsening of depression or suicidal ideation, asses for weight gain and excessive somnolence or dizziness, monitor for orthostatic hypotension w/ a Hx of cardiovascular disease or cerebrovascular disease.
1.143. Trazadone (Desyrel, Oleptro) Class: Antidepressant Actions: Centrally acting antidepressant that potentiates serotonin effects by selectively blocking its reuptake at presynaptic membranes in CNS. Onset: 1-2wks. Peak: 1-2hrs. Indications: Depression Norm. Dosage, Freq, Route, Range: PO 150mg/day in divided doses, may increase by 50mg/day q34days Max: 400-600mg/day (Immediate release) PO 150mg/day may increase by 75mg/day at 3 day intervals Max: 375mg/day (Extended release) Side Effects: drowsiness, hypotension (including orthostatic hypotension), dry mouth Nursing Considerations: Monitor BP & HR & rhythm; monitor for orthostatic hypotension; be aware that overdose is characterized by an extension of common adverse effects: vomiting, lethargy, drowsiness, and exaggerated anticholinergic effects.
1.144. Venlafaxine (Effexor) Class: Antidepressant; Serotonin Norepinephrine Reuptake Inhibitor (SNRI) Actions: Potent inhibitor of neuronal serotonin and norepinephrine reuptake. Onset: 2wks. Peak: 1-2hrs. Duration: extensively tissue bound Indications: Depression; Anxiety Norm. Dosage, Freq, Route, Range: PO 25-125mg tid Max: 375mg/day Side Effects: increased BP & HR, dizziness, somnolence, suicidality, nausea, vomiting, dry mouth, sweating Nursing Considerations: Monitor for worsening of depression or emergence of suicidal ideation; monitor cardiovascular status periodically w/ measurements of BP & HR; Lab tests: periodic lipid profile; monitor neurologic status and report excessive anxiety, nervousness, and insomnia; monitor weight periodically and report excess weight loss; avoid using alcohol
Page 64 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
39. Tricyclic Antidepressants 1.145. Amitriptyline HCL (Elavil) Class: Tricyclic Antidepressant Actions: a tricyclic antidepressant that inhibits the reuptake of serotonin (5-HT) and norepinephrine from the synaptic gap; also inhibits norepinephrine reuptake to a moderate degree. Peak: 2-12hrs. Indications: Antidepressant Norm. Dosage, Freq, Route, Range: Side Effects: drowsiness, sedation, dizziness, orthostatic hypotension, dry mouth, constipation, urinary retention, bone marrow suppression Nursing Considerations: Lab tests: baseline and periodic leukocyte and differential counts, renal and hepatic function tests, monitor BP and pulse rate, monitor I&O and bowel elimination pattern
1.146. Doxepin HCL (Sinequan, Prudoxin, Silenor, Zonalon) Class: Tricyclic Antidepressants; Anxiolytic Actions: inhibits serotonin reuptake from the synaptic gap; also inhibits norepinephrine reuptake to a moderate degree. Peak: 2hrs. Indications: Depression/Anxiety; Insomnia (Silenor), Dermatitis Norm. Dosage, Freq, Route, Range: PO 25-150mg/day in divided doses, may increase up to 300mg/day Max: 300mg/day Side Effects: drowsiness, orthostatic hypotension, dry mouth, blurring or stinging at application site Nursing Considerations: monitor use of other CNS depressants, including alcohol; be alert to changes in voiding and evaluate pt. for constipation and abdominal distention; maintain established dosage regimen and avoid change of intervals, doubling, reducing, or skipping doses.
1.147. Imipramine HCL (Tofranil) Class: Tricyclic Antidepressant (TCA) Actions: TCAs potentiate both norepinephrine and serotonin in the CNS by blocking their reuptake. Peak: 1-2hr. Indications: Depression; enuresis Norm. Dosage, Freq, Route, Range: PO 75-100mg/day Max: 300mg/day in 1 or more divided doses. Side Effects: sedation, drowsiness, angioedema, orthostatic hypotension, arrhythmias, MI, heart block, blurred vision, slight mydriasis, dry mouth, urinary retention, agranulocytosis, thrombocytopenia Nursing Considerations: Lab tests: monitor periodic LFTs, renal function, CBC w/ diff, and fluid and electrolyte balance, monitor HR and BP frequently, report EPS, Avoid exposure to sunlight and use sunscreen
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 65 of 75
Drug Med Cards
1.148. Nortriptyline HCL (Aventyl, Pamelor) Class: Tricyclic Antidepressant Actions: Secondary amine derivative of amitriptyline that inhibits that action of many chemical agents including catecholamines. Mood elevation may be due to its inhibition of reuptake of serotonin or another neurotransmitter at the presynaptic membrane. Peak: 7-8.5hrs. Duration: Crosses placenta; distributed in breast milk Indications: Antidepressant; Nocturnal Enuresis Norm. Dosage, Freq, Route, Range: PO 25mg tid or qid, gradually increase to 100-150mg/day Side Effects: orthostatic hypotension, dry mouth, agranulocytosis, urinary retention Nursing Considerations: monitor BP & pulse rate during adjustment period, if systolic BP fall more than 20mm Hg or if there is a sudden increase in pulse rate, w/hold medication and notify prescriber; inspect oral membranes daily; monitor bowel elimination pattern and I&O ratio; do not use OTC drugs unless your prescriber approves
Page 66 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
40. Selective Serotonin Reuptake Inhibitor (SSRI) 1.149. Citalopram Hydrobromide (Celexa) Class: Selective Serotonin Reuptake Inhibitor (SSRI) Actions: SSRI w/ an antidepressant effect presumed to be linked to its inhibition of CNS presynaptic neuronal uptake of serotonin. Peak: steady-state serum concentrations in 1wk; peak blood levels at 4hrs. Indications: Depression Norm. Dosage, Freq, Route, Range: PO start at 20mg/day, may increase to 40mg/day if needed Side Effects: nausea, dry mouth, insomnia, somnolence Nursing Considerations: watch closely for worsening of depression or emergence of suicidal ideations; Lab tests: monitor periodically hepatic function, CBC, serum sodium, and lithium levels when the two drugs are given concurrently; monitor periodically HR & BP, and carefully monitor complete cardiac status in person w/ known or cardiac disease; avoid alcohol
1.150. Escitalopram Oxalate (Lexapro) Class: Antidepressant; Selective Serotonin Reuptake Inhibitor (SSRI) Actions: antidepressant effect is presumed to be linked to its inhibition of CNS presynaptic neuronal uptake of serotonin. Onset: Approximately 1 wk. Peak: 3hr Half-life: 25hr Indications: depression, generalized anxiety disorder Norm. Dosage, Freq, Route, Range: PO 10mg daily, may increase to 20mg daily if needed after 1 wk Max: 20mg/day Side Effects: nausea, insomnia, somnolence, decreased libido Nursing Considerations: closely observe for worsening of depression or suicide, Lab tests: monitor periodically LFTs, serum sodium, and lithium levels, monitor periodically HR and BP and carefully monitor complete cardiac status
1.151. Fluoxetine HCL (Prozac) Class: Selective Serotonin Reuptake Inhibitor (SSRI), Antidepressant Actions: antidepressant effect is presumed to be linked to inhibition of CNS neuronal uptake of serotonin Indications: disorder
depression, gastric depression, OCD, bulimia, premenstrual dysphoric disorder, panic
Norm. Dosage, Freq, Route, Range: PO 20mg/day in AM, may increase by 20mg/day at weekly intervals Max: 80mg/day Side Effects: headache, nervousness, anxiety, insomnia, nausea, diarrhea Nursing Considerations: Monitor renal and hepatic functions. Supervise patients closely who are high suicide risks. Lab tests: periodic serum electrolytes, monitor closely plasma glucose in diabetes.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 67 of 75
Drug Med Cards
1.152. Paroxetine (Paxil, Pexeva) Class: Antidepressant; Selective Serotonin Reuptake Inhibitor (SSRI) Actions: It is highly potent and a highly selective inhibitor of serotonin reuptake by neurons in CNS. Onset: 2wks. Peak: 5-8hrs. Indications: Depression; OCD; Panic Attacks; Social Anxiety; Generalized Anxiety, PTSD; Premenstrual Dysphoric Disorder Norm. Dosage, Freq, Route, Range: PO 10-50mg/day Max: 80mg/day Side Effects: Headache, sedation, nausea, dry mouth Nursing Considerations: monitor for worsening of depression or emergence of suicidal ideation; monitor for significant weight loss; monitor pt. w/ history of mania for reactivation of condition; monitor pts. w/ preexisting cardiovascular disease carefully because paroxetine may adversely affect hemodynamics status
1.153. Sertraline HCL (Zoloft) Class: Antidepressant; Selective Serotonin Reuptake Inhibitor (SSRI) Actions: Effective in controlling depression, obsessive-compulsive disorder, anxiety, and panic disorder. Onset: 2-4 weeks Indications: Depression, Anxiety, Obsessive-Compulsive Disorder Norm. Dosage, Freq, Route, Range: begin w/ 50mg/day, gradually increase every few weeks according to response Max: 200mg/day Side Effects: agitation, insomnia, headache, dizziness, somnolence, fatigue Nursing Considerations: supervise patients at risk for suicide closely, monitor for worsening of depression or emergence of suicidal ideation, monitor older adults for fluid and sodium imbalances, monitor patients w/ a Hx of a seizure disorder closely, lab tests: monitor PT /INR w/ patients receiving concurrent warfarin therapy
1.154. Vilazodone (Vibryd) Class: Selective Serotonin Reuptake Inhibitor (SSRI); Psychotherapeutic Agent; Antidepressant Actions: Antidepressant is presumed to be linked to inhibition of CNS neuronal uptake of the neurotransmitter, serotonin. Peak: 4-5hrs. Indications: Major Depressive Disorder Norm. Dosage, Freq, Route, Range: PO initial dose of 10mg/day for 7 days, increase to 20mg/day for 7 days, then to 40mg/day Side Effects: dizziness, diarrhea, nausea Nursing Considerations: monitor for worsening of depression or emergence of suicidal ideation; supervise pts. Closely who are high suicide risks; do not stop medication abruptly
Page 68 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
41. Monoamine Oxidase Inhibitors (MAOIs) 1.155. Isocarboxazid (Marplan) Class: Antidepressant; MAOI Actions: Inhibits monoamine oxidase, the enzyme involved in the catabolism of catecholamine neurotransmitters and serotonin. Duration: up to 2wks. Indications: Refractory Depression Norm. Dosage, Freq, Route, Range: PO 10-30mg/day in 1-3 divided doses Max: 30mg/day Side Effects: drowsiness, overactivity, insomnia, orthostatic hypotension, paradoxical hypertension, blurred vision, nausea, constipation, anorexia, urinary retention, dry mouth Nursing Considerations: Monitor BP for orthostatic hypotension, monitor for therapeutic effectiveness, monitor and report promptly signs of clinical deterioration or suicidal ideation, check for peripheral edema daily and monitor weight several times weekly and monitor weight several times weekly, toxic symptoms from over-dosage or from substances or from ingestion of contraindicated substances (e.g., foods high in tyramine) may occur w/in hours
1.156. Phenelzine Sulfate (Nardil) Class: Antidepressant; MAOI Actions: potent hydrazine MAOI. Antidepressant action believed to be due to irreversible inhibition of MAOI, thereby permitting increased conxentrations of endogenous epinephrine, norepinephrine, serotonin, and dopamine w/in presynaptic neurons and at receptor sites. Onset: 2 weeks Indications: Depression Norm. Dosage, Freq, Route, Range: PO 1.5mg tid, rapidly increase to at least 60mg/day, may need up to 90mg/day Max: 90mg/day Side Effects: orthostatic hypotension, insomnia, respiratory depression, coma, hypertensive crisis, circulatory collapse, constipation, dry mouth, nausea, vomiting, anorexia, leukopenia Nursing Considerations: Monitor BP and Pulse, Lab tests: baseline and periodic CBC and LFTs; pts on prolonged therapy should be checked periodically for altered color perception, changes in fundi or visual fields, changes in red-green vision may be the 1st indication of eye damage, strict thymine diet
1.157. Tranylcypromine Sulfate (Parnate) Class: Antidepressant; MAOI Actions: Potent MAO w/ a antidepressant activity that arises from the increased availability of monoamines resulting from the inhibition of the enzyme MAO. This leads to increased concentration of neurotransmitters, such as epinephrine, norepinephrine, and dopamine in the CNS. Onset: 10 days Indications: Severe Depression Norm. Dosage, Freq, Route, Range: PO 30mg/day in 2 divided doses, may increase by 10mg/day at 23wk intervals Max: 60mg/day Side Effects: Orthostatic hypotension, hypertensive crisis Nursing Considerations: monitor BP closely, sever hypertensive reactions are known to occur with MAOIs; monitor for changes in behavior; do not eat tyramine-containing foods; be aware of excessive use of caffeine-containing beverages; make position changes slowly; avoid alcohol and other CNS depressants
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 69 of 75
Drug Med Cards
42. Anti-Emetic 1.158. Ondansetron HCL (Zofran) Class: 5-HT3 Anatagonist, Antiemetic Actions: Prevents nausea and vomiting associated with cancer chemotherapy and anesthesia. Peak: 11.5hr Half-life: 3hr Indications: prevention of nausea and vomiting associated with initiation and repeated courses of cancer chemotherapy, including high-dose cisplatin; postoperative nausea and vomiting Norm. Dosage, Freq, Route, Range: PO 8-24mg 30 min before chemotherapy, than q8hr times 2 more doses Side Effects: headache, sedation, diarrhea Nursing Considerations: monitor fluid and electrolyte status, cardiovascular status
Page 70 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
43. Antituberculosis 1.159. Isoniazid (INH, Laniazid) Class: Anti-infective; Antituberculosis Actions: Exerts bacteriostatic action against actively growing tubercle bacilli, may be bactericidal in higher concentrations. Peak: 1-2 hr Indications: Treatment of Active Tuberculosis, preventative therapy Norm. Dosage, Freq, Route, Range: PO/IM 5mg/kg Max: 300 mg/day Side Effects: Paresthesias, peripheral neuropathy, hepatotoxicity (elevated AST, ALT; bilirubinemia; jaundice; hepatitis) Nursing Considerations: Monitor for therapeutic effectiveness, w/hold drug and notify prescriber immediately of a hypersensitivity reaction, Lab tests: monitor LFTs periodically, monitor for and report signs of hepatotoxicity, monitor BP, check weight at least twice weekly under standard conditions
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 71 of 75
Drug Med Cards
44. Substance Abuse Deterrent 1.160. Acamprosate Calcium (Campral) Class: Substance Abuse Deterrent Actions: Reduces craving for alcohol intake due to chronic use, but does not cause alcohol aversion or a disulfiram-like reaction as a result of alcohol ingestion. Half-life: 20-33hr. Indications: Maintenance of Alcohol Abstinence Norm. Dosage, Freq, Route, Range: PO 666mg tid Side Effects: diarrhea, flatulence Nursing Considerations: Monitor S&S of depression or suicidal thinking; monitor or impaired judgment or thinking, dizziness or impaired motor skills; report promptly unusual anxiousness or nervousness, depression or suicidal thoughts, burning or tingling sensations in arms, legs, hands or feet, chest pains or palpitations, or difficulty urinating; report any alcohol consumption during therapy.
1.161. Antabuse Class: Enzyme Inhibitor; Anti-Alcoholic Agent Actions: Acts as a deterrent to alcohol ingestion by inhibiting the enzyme acetaldehyde dehydrogenase, which normally metabolizes alcohol in the body. Onset: Up to 12hr. Duration: Up to 2wk. Onset: Up to 12hr. Duration: Up to 2wk. Indications: Alcoholism Norm. Dosage, Freq, Route, Range: PO 500mg/day for 1-2wk, then 125-500mg/day Max: 500mg/day Side Effects: marked respiratory depression, unconsciousness, convulsions, sudden death, hepatotoxicity Nursing Considerations: Lab tests: baseline & follow-up transaminase studies every 10-14 days to detect hepatic dysfunction; treat pt. w/ severe disulfiram reaction as though in shock, monitor potassium levels, especially if pt. has diabetes mellitus; explain the danger of alcohol ingestion during treatment to pt.; report promptly to prescriber the onset of nausea w/ RUQ pain or discomfort, itching, jaundiced sclera or skin, dark urine or clay-colored stools, w/hold drug pending LFTs
Page 72 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
45. Bone Metabolism Regulatory 1.162. Pamidronate (Aredia) Class: Bisphosphonate (Bone Metabolism Regulatory) Actions: Reduces bone turnover and, when used in combination with adequate hydration, it increases renal excretion of calcium, thus reducing serum calcium concentrations. Onset: 24-48 hr Peak: 6 days Duration: 2 weeks-3months Indications: Moderate to severe hypercalcemia of malignancy, Paget’s Diease, Osteolytic Metastases Norm. Dosage, Freq, Route, Range: IV 60-90 mg infused over 4-24 hr, may repeat in 7 days Side Effects: fever w/ or w/o rigors, thrombophlebitis at injection site, hypocalcemia, epigastric discomfort Nursing Considerations: Assess IV injection site for thrombophlebitis, Lab tests: monitor serm calcium, phosphate, magnesium, and potassium at frequent intervals; CBC with defferential, Hct and Hgb; and kidney function tests throughout course of therapy, monitor for S&S of hypocalcemia, hypokalemia, hypomagnesemia and hypophosphatemia, monitor for seizures, monitor vital signs
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 73 of 75
Drug Med Cards
46. Bacterial Collagenase Enzyme 1.163. Collagenase Clostridum Histolyticum (Xiaflex) Class: Bacterial Collagenase enzyme Actions: Collagenases are proteinases that hydrolyze collagen in its native triple helical conformation under physiological conditions, resulting in lysis of collagen deposits. Indications: Dupuytren’s contracture, Peyronie’s Disease Norm. Dosage, Freq, Route, Range: Topical 1-3x daily to affected areas Side Effects: mild pain or tenderness in treated hand, cracked skin, under arm pain Nursing Considerations: call physician if fever, chills, body aches, flu symptoms, or swollen glands in your elbow or under arm, watch for bleeding, bruising, swelling, redness, warmth, numbness, tingling, or sudden pain or loss of movement
Page 74 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
Bibliography Ebersole, P., Hess, P., Touhy, T.A., Schmidt Logan, A., & Jett, K. (2008) Toward healthy aging: Human needs and nursing response ( 7th ed.). St. Louis, MO: Mosby. Eliopoulous C. (2009). Gerontological nursing. ( 7th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. Grodner, M., Long, S., & Walkingshaw,B.C. (2007). Foundations and clinical application of nutrition: A nursing approach ( 4th ed.). St. Louis, MO: Mosby. Ignatavicius, D. D., & Workman, M. L. (2010). Medical-Surgical nursing (6th ed.). St. Louis, MO: Saunders. Lowdermilk, D.L.,& Perry, S.E. ( 2007) . Maternity & women’s health care (9th ed.). St. Louis, MO: Mosby. Lehne, R.A. (2010). Pharmacology for nursing care (7th ed.). St. Louis, MO: Saunders. Lilley, L. L., Harrington, S., & Snyder, J.S. (2007). Pharmacology and the nursing process (5th ED.). St. Louis, MO: Mosby. Roach, S. S.,& Ford, S. M. (2008). Introductory clinical pharmacology. Philadelphia, PA: Lippincott Williams & Wilkins. Smeltzer, S. C., Bare, B.G., Hinkle, J. L., & Cheever, K.H. ( 2008). Brunner and Suddarth’s textbook of medical-surgical nursing ( 11th ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 75 of 75
Acyclovir
Amantadine HCl
(Zovirax)
(Symmetrel)
Class: Antiviral
Class: Antiviral; Central-Acting Cholinergic Receptor Antagonist; Antiparkinson
Actions: reduces viral shedding and formation of new lesions and speeds healing time. Peak: 1.5-2hr. Half-life: 2.5-5hr.
Actions: Because Amantadine does not suppress antibody formation, it can be istered for interim protection in combination w/ influenza. Onset: w/in 48hrs. Peak: 1-4hrs
Indications: (IV treatment) viral encephalitis, herpes simplex, varicella-zoster virus (shingles/chickpox); (orally) herpes simplex, varicella-zoster virus; (topically) herpes labialis (cold sores) and initial episodes of herpes gentitalis
Indications: Influenza A Treatment; Influenza A Preventative; Parkinsonism; DrugInduced Extrapyramidal Symptoms (EPS)
Norm. Dosage, Freq, Route, Range: PO 400mg bid Max: 800mg/day
Norm. Dosage, Freq, Route, Range: PO 100mg 1-2times/day
Side Effects: headache, nausea, vomiting, diarrhea
Side Effects: dizziness, light-headedness, difficulty in concentrating, insomnia, leukopenia
Nursing Considerations: Monitor I&O & hydration status. Lab tests: baseline and periodic renal function tests
Nursing Considerations: Lab tests: pH and serum electrolytes; monitor and report mental status changes, nervousness, difficulty concentrating, or insomnia, loss of seizure control, S&S of toxicity, especially in doses over 200mg/day
Alprazolam
Diazepam
(Xanax)
(Diastat, Valium)
Class: Anxiolytic; Sedative-Hypnotic; Benzodiazepine
Class: Benzodiazepine Anticonvulsant; Anxiolytic
Actions: A CNS depressant that appears to act at the limbic, thalamic, and hypothalamic levels of the CNS. Has antianxiety and sedative effects w/ addictive potential. Peak: 1-2 hr. Halh-life: 12-15 hr.
Actions: Long-acting benzodiazepine psychotherapeutic agent. Benzodiazepines act at the limbic. Thalamic, and hypothalamic regions of the CNS and produce CNS depression resulting in sedation, and anticonvulsant activity dependent on the dosage. Onset: PO 30-60 min Peak: PO 1-2 hr Duration: IV 15 min-1 hr PO up to 3 hr
Indications: Anxiety Disorders, Panic Attacks Indications: Status Epilepticus, Muscle Spasm, Anxiety, Alcohol Withdrawal, Pre-op Norm. Dosage, Freq, Route, Range: PO 0.25-5 mg tid Max: 4 mg/day Norm. Dosage, Freq, Route, Range: IV/IM 5-10 m, repeat if needed at 10-15 min intervals up to 30 mg, then repeat if needed q2-4hr
Side Effects: Drowsiness, sedation Nursing Considerations: Monitor S&S of drowsiness and sedation, especially in older adults or the debilitated, Lab tests: CBC, urinalysis and blood chemistry studies particularly during continuing therapy
Side Effects: Drowsiness, fatigue, confusion, vivid dreams, headache Nursing Considerations: Monitor for adverse reactions, Monitor for therapeutic effectiveness-max effect may require 1-2 week, monitor for and report promptly signs of suicidal ideation especially in those treated for anxiety states accompanied by depression, observe patient closely and monitor vital signs when diazepam is given parentally; hypotension, muscular weakness, tachycardia, and respiratory depression may occur, Lab tests: periodic CBC and LFTs
Lorazepam
Temazepam
(Ativan)
(Restoril)
Class: Anxioltic; Sedative-Hypnotic; Benzodiazepine
Class: Benzodiazepine, Anxiolytic, Sedative-Hypnotic
Actions: most potent of the available benzodiazepine. Effects (antianxiety, sedative, hypnotic, and skeletal muscle relaxant) are mediated by the inhibition neurotransmitter GABA. Action sites are thalamic, hypothalamic, and limbic levels of CNS. Onset: IV 1-5 min. IM 15-30 min. Peak: IM 60-9 min. PO 2 hr Duration 12-24 hr
Actions: reduces night awakenings and early morning awakenings; increases total sleep times, absence of rebound effects. Onset: 30-50 min. Peak: 2-3hr. Duration: 10-12hr. Half-life: 8-24hr Indications: to relieve insomnia
Indications: Antianxiety, Insomnia, Premedication, Status Epilepticus Norm. Dosage, Freq, Route, Range: PO 7.5-30mg at bedtime Max: 30mg/night Norm. Dosage, Freq, Route, Range: PO 2-6 mg/day in divided doses Max: 10 mg/day Side Effects: drowsiness, sedation, dizziness, weakness Nursing Considerations: Supervise ambulation, Lab tests: Assess CBC and LFTs periodically
Side Effects: drowsiness, dizziness, lethargy Nursing Considerations: hypersensitivity, Lab tests: LFTs and kidney function tests during long-term use, be aware of S&S of overdose: weakness, confusion, slurred speech, ataxia, coma w/ reduced or absent reflexes, hypertension and respiratory depression
Drug Med Cards
Table of Contents 1. Anti-Viral ........................................................................................................................................... 5 2. Benzodiazepenes .............................................................................................................................. 6 3. Diuretics ............................................................................................................................................ 8 4. Antiseizure Meds .............................................................................................................................. 9 5. Vitamins and Minerals .................................................................................................................... 13 6. Steroid ............................................................................................................................................. 14 7. Opiod............................................................................................................................................... 15 8. Opiod Antagonists........................................................................................................................... 17 9. NSAIDS ............................................................................................................................................ 18 10. Analgesic, Antipyretic ..................................................................................................................... 19 11. Anticholinergic ................................................................................................................................ 20 12. Bronchodilator ................................................................................................................................ 21 13. Thyroid Hormone Replacement ...................................................................................................... 22 14. Alpha Adronergic Receptor Antagonist .......................................................................................... 23 15. Antiparkinson (Cholinergic Receptor Antagonist............................................................................ 24 16. Fluid and Electrolytes ...................................................................................................................... 26 17. Antibiotics ....................................................................................................................................... 28 18. Cholesterol Lowering Agents .......................................................................................................... 32 19. Laxatives/ Stool Softeners............................................................................................................... 34 20. Anti-Diarrheal.................................................................................................................................. 36 21. Beta-Blockers .................................................................................................................................. 37 22. Nitrates ........................................................................................................................................... 39 23. ACE-Inhibitors ................................................................................................................................. 40 24. Calcium Channel Blockers ............................................................................................................... 41 25. Central Acting Antihypertensive ..................................................................................................... 42 26. Antihypertensives ........................................................................................................................... 43 27. Antipsychotics ................................................................................................................................. 44 28. Anti-Coagulants ............................................................................................................................... 50 29. Antiplatelets .................................................................................................................................... 51 30. Proton Pump Inhibitor .................................................................................................................... 52 31. H2- Receptor Antagonist ................................................................................................................. 53 32. Cerebral Stimulant .......................................................................................................................... 54 33. Antihistamines ................................................................................................................................ 55 34. Antidiabetic ..................................................................................................................................... 57 35. Antihypoglycemic ............................................................................................................................ 60 36. Anti-fungal....................................................................................................................................... 61 37. Eye Drops ........................................................................................................................................ 62 38. Antidepressant ................................................................................................................................ 63 39. Tricyclic Antidepressants ................................................................................................................ 65 40. Selective Serotonin Reuptake Inhibitor (SSRI) ................................................................................ 67 41. Monoamine Oxidase Inhibitors (MAOIs) ........................................................................................ 69 42. Anti-Emetic...................................................................................................................................... 70 43. Antituberculosis .............................................................................................................................. 71 44. Substance Abuse Deterrent ............................................................................................................ 72 45. Bone Metabolism Regulatory ......................................................................................................... 73 46. Bacterial Collagenase Enzyme......................................................................................................... 74 Bibliography ................................................................................................................................................ 75
Page 2 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards With over 8 years in the medical field, Mike Linares has worked both out in the field on an Ambulance in the dangerous streets of Los Angeles County and the in crazy busy the Emergency Rooms. Coupled with his ion for teaching & desire to help other students and mixed with his chronic typpos and bad grammmer, SIMPLEnursing.com was born to not only help his fellow RN students, but nursing students worldwide. "I hope you enjoy the valuable jewels that Simplenursing.com has to offer. If so please let me know! I am a real person & I´d love to hear your thoughts good or bad on Face book, Twitter, or Youtube." Committed to Your Success, Mike P.S.Feel free to Face book, Twitter, or Youtube me!!
Mike Linares Student Nurse Mentor & Certified EKG Instructor
HOW THIS WHOLE THING CAME TO BE... Before Helping Multiple Successful Nursing Students Excel I Was The "Drone" Nursing Student Working Too Hard & Eventually I FAILED OUT of Nursing School.
Before Helping Hundreds of Struggling Nursing Students Reach Graduation Day & Before Becoming a Student Nurse Mentor & Certified EKG Instructor, I Myself Was A Struggling "At Risk" Student Nurse Drowning In My Books & Lost In Clinical. I was that struggling student working full time in the Emergency Room at one of those MEGA hospitals in Orange, California. I worked as an EMT aka a "medic" for 8 years prior to failing out. I knew how to take care patients, I knew the basics of the ABCs of basic life , I knew how to take vital signs and how to fix minor injuries. I thought I had enough experience to skate right through nursing school, I thinking "how hard can it be" right? After two semesters, I FAILED out of the Program. I felt defeated, depressed and like a loser. It was one of the lowest points of my life. Sitting in my room practically bawling my eyes out, I quotes my mom and dad used to encourage me with, "son, whatever doesn´t kill you, Makes you Stronger" & " Failing is Not a Bad Thing, As long as learn, become better, and NEVER EVER QUIT"
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 3 of 75
Drug Med Cards My Clinial FAILURE form had bold red letters stating: LACK In Prepared LACK Organizational Skills LACK Critical Thinking with Nursing Process Ending with: "able to return next semester contingent upon demonstrating INCREASED COMPETANCIES in these core areas." "NEVER GIVE UP!!" my mom & dad used to tell me, so I set out on a Quest to develop a system to make Simplify Nursing School! What Happened Next Might Surprise you, In a systematic way to put all the "core competencies" of nursing school that instructors look for to students. My quest was to make it SIMPLE first and foremost, by cutting out the fluff and getting down to the nitty critty making it easier. The Goal Was To Make A Simple System... And the best part is it was really helping myself and other students in my class their tests when I would share with them my strategies and systems to help them their tests without having to memorize everything in the book!
This is where my mentoring for student nurses began. That's when something clicked and everything changed for me. It was like I had an Ah - HA moment! At that moment I realized there are better, more predictable, and more low cost ways to get higher test scores and have more critical thinking skills than the money I had been spending on dead end study books that claimed to help but really just confuse me more. I needed simplicity!!! Within the next six months I had created over 27 different student help systems, strategies and tactics that produced better results for me - some better than others. Then over the next few semesters I tracked, tested, and tweaked each system until my students were ing with a 82% or better on each and every test, 2 students being out of School for over 25 years & coming back to score 94% on their EKG cardiac test! Truly amazing & truly making me proud to be their mentor.
Page 4 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.
Anti-Viral
1.1. Acyclovir (Zovirax) Class: Antiviral Actions: reduces viral shedding and formation of new lesions and speeds healing time. Peak: 1.5-2hr. Half-life: 2.5-5hr. Indications: (IV treatment) viral encephalitis, herpes simplex, varicella-zoster virus (shingles/chickpox); (orally) herpes simplex, varicella-zoster virus; (topically) herpes labialis (cold sores) and initial episodes of herpes gentitalis Norm. Dosage, Freq, Route, Range: PO 400mg bid Max: 800mg/day Side Effects: headache, nausea, vomiting, diarrhea Nursing Considerations: Monitor I&O & hydration status. Lab tests: baseline and periodic renal function tests
1.2. Amantadine HCl (Symmetrel) Class: Antiviral; Central-Acting Cholinergic Receptor Antagonist; Antiparkinson Actions: Because Amantadine does not suppress antibody formation, it can be istered for interim protection in combination w/ influenza. Onset: w/in 48hrs. Peak: 1-4hrs Indications: Influenza A Treatment; Influenza A Preventative; Parkinsonism; Drug-Induced Extrapyramidal Symptoms (EPS) Norm. Dosage, Freq, Route, Range: PO 100mg 1-2times/day Side Effects: dizziness, light-headedness, difficulty in concentrating, insomnia, leukopenia Nursing Considerations: Lab tests: pH and serum electrolytes; monitor and report mental status changes, nervousness, difficulty concentrating, or insomnia, loss of seizure control, S&S of toxicity, especially in doses over 200mg/day
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 5 of 75
Drug Med Cards
2.
Benzodiazepenes
1.3. Alprazolam (Xanax) Class: Anxiolytic; Sedative-Hypnotic; Benzodiazepine Actions: A CNS depressant that appears to act at the limbic, thalamic, and hypothalamic levels of the CNS. Has antianxiety and sedative effects w/ addictive potential. Peak: 1-2 hr. Halh-life: 12-15 hr. Indications: Anxiety Disorders, Panic Attacks Norm. Dosage, Freq, Route, Range: PO 0.25-5 mg tid Max: 4 mg/day Side Effects: Drowsiness, sedation Nursing Considerations: Monitor S&S of drowsiness and sedation, especially in older adults or the debilitated, Lab tests: CBC, urinalysis and blood chemistry studies particularly during continuing therapy
1.4. Diazepam (Diastat, Valium) Class: Benzodiazepine Anticonvulsant; Anxiolytic Actions: Long-acting benzodiazepine psychotherapeutic agent. Benzodiazepines act at the limbic. Thalamic, and hypothalamic regions of the CNS and produce CNS depression resulting in sedation, and anticonvulsant activity dependent on the dosage. Onset: PO 30-60 min Peak: PO 1-2 hr Duration: IV 15 min-1 hr PO up to 3 hr Indications: Status Epilepticus, Muscle Spasm, Anxiety, Alcohol Withdrawal, Pre-op Norm. Dosage, Freq, Route, Range: IV/IM 5-10 m, repeat if needed at 10-15 min intervals up to 30 mg, then repeat if needed q2-4hr Side Effects: Drowsiness, fatigue, confusion, vivid dreams, headache Nursing Considerations: Monitor for adverse reactions, Monitor for therapeutic effectiveness-max effect may require 1-2 week, monitor for and report promptly signs of suicidal ideation especially in those treated for anxiety states accompanied by depression, observe patient closely and monitor vital signs when diazepam is given parentally; hypotension, muscular weakness, tachycardia, and respiratory depression may occur, Lab tests: periodic CBC and LFTs.
1.5. Lorazepam (Ativan) Class: Anxioltic; Sedative-Hypnotic; Benzodiazepine Actions: most potent of the available benzodiazepine. Effects (antianxiety, sedative, hypnotic, and skeletal muscle relaxant) are mediated by the inhibition neurotransmitter GABA. Action sites are thalamic, hypothalamic, and limbic levels of CNS. Onset: IV 1-5 min. IM 15-30 min. Peak: IM 60-9 min. PO 2 hr Duration 12-24 hr Indications: Antianxiety, Insomnia, Premedication, Status Epilepticus Norm. Dosage, Freq, Route, Range: PO 2-6 mg/day in divided doses Max: 10 mg/day Side Effects: drowsiness, sedation, dizziness, weakness Nursing Considerations: Supervise ambulation, Lab tests: Assess CBC and LFTs periodically
Page 6 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.6. Temazepam (Restoril) Class: Benzodiazepine, Anxiolytic, Sedative-Hypnotic Actions: reduces night awakenings and early morning awakenings; increases total sleep times, absence of rebound effects. Onset: 30-50 min. Peak: 2-3hr. Duration: 10-12hr. Half-life: 8-24hr Indications: to relieve insomnia Norm. Dosage, Freq, Route, Range: PO 7.5-30mg at bedtime Max: 30mg/night Side Effects: drowsiness, dizziness, lethargy Nursing Considerations: hypersensitivity, Lab tests: LFTs and kidney function tests during long-term use, be aware of S&S of overdose: weakness, confusion, slurred speech, ataxia, coma w/ reduced or absent reflexes, hypertension and respiratory depression
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 7 of 75
Drug Med Cards
3.
Diuretics
1.7. Furosemide (Lasix) Class: Loop diruetic Actions: Inhibits NA & Cl reabsorption, ↑ urine, ↓ edema & intravascular volume. Onset: PO 30-60min. IV 5 min Peak: PO 60-70min IV 20-60min. Duration: 2hr. Indications: promote urine output & decrease edema associated w/ CHF, cirrhosis of liver & kidney disease, decrease CHF, decrease hypertension Norm. Dosage, Freq, Route, Range: (Edema) PO: 20-80 mg in 1 or more divided doses Max: 600 mg/day (Hypertension) PO: 10-40 mg/kg bid Max: 480 mg/day Side Effects: Circulatory collapse, hypokalemia, aplastic anemia, agranulocytosis (rare) Nursing Considerations: check K+ levels prior to ., monitor I&O closely, rapid acting doses to prevent sleep disturbance, Potassium rich foods: bananas, oranges, dried dates, etc., CBC, serum and urine electrolytes, CO2 BUN, Blood Sugar, Uric Acid, Urine and Blood Glucose, HbA1C in diabetic patients w/ decompensated hepatic cirrhosis, may cause hyperglycemia
1.8. Hydrochlorothiazide (Microzide, Oretic) Class: Electrolytic and Water Balance; Thiazide Diuretic Actions: Therapeutic effectiveness is measured by decrease in edema and lowering of blood pressure. Onset: 2hr. Peak: 4hr. Duration: 6-12hr. Half-life: 45-120min. Indications: adjunct treatment of edema associated with CHF, hepatic cirrhosis, renal failure, and in the management of hypertension Norm. Dosage, Freq, Route, Range: PO 25-100mg/day in 1-3 divided doses Max: 200mg/day Side Effects: Hyperglycemia, hyperuricemia, hypokalemia Nursing Considerations: Check BP, monitor I&O and check for edema, Lab tests: baseline and periodic determinations of serum electrolytes, blood counts, BUN, blood glucose, uric acid, CO2, are recommended.
1.9. Spironolactone (Aldactone) Class: Electrolytic and water balance; Aldosterone Antagonist; Potassium-Sparing Diuretic Actions: A diuretic agent that promotes sodium and chloride excretion w/o concomitant loss of potassium. Lowers systolic and diastolic pressures in hypertensive patients. Effective in treatment of primary aldosteronism. Onset: gradual Peak: 2-3days; Max effect may take up to 2 weeks Duration: 2-3 days or longer Indications: Edema due to CHF, Hypertension, Primary Aldosteronism, Hypokalemia Norm. Dosage, Freq, Route, Range: PO 25-400mg/day in divided doses Max: 400mg/day Side Effects: fluid and electrolyte imbalance, nausea, vomiting Nursing Considerations: check BP, lab tests: monitor serum electrolytes (Na and K), assess for signs and symptoms of fluid and electrolyte imbalance, monitor daily I&O and check for edema
Page 8 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
4.
Antiseizure Meds
1.10. Carbamazepine (Carbatrol, Tegretol, Epitol, Equetro, Mazepine) Class: Anticonvulsant tricyclic Actions: effective anticonvulsant for a range of seizure disorders and as an adjuvant reduces depressive S&S and stabilizes mood. Peak: 2-8hr. Half-life: variable due to autoinduction 25-65hr. than 14-16he with repeated use Indications: Seizures; Trigeminal Neuralgia; Bipolar Disorder (Equetro) Norm. Dosage, Freq, Route, Range: PO 200mg bid, gradually increase to 800-1200mg/day in 3-4 divided doses Max: 1200mg/day Side Effects: leukopenia, confusion, headache, dizziness Nursing Considerations: Lab tests: baseline and periodic CBCs including platelets, reticulocytes, serum electrolytes and serum iron, LFTs, BUN and complete urinalysis, attempt a dosage reduction after 3 months, monitor for toxicity, I&O and vital signs
1.11. Clonazepam (Klonopin) Class: Anticonvulsant; Benzodiazepine Actions: Suppresses spike and wave discharge (petitmal) and decreases amplitude, frequency, duration, and spread of discharge in minor motor seizures. Onset: 60 min Peak: 1-2 hr Duration up to 12 hr in adults; 6-8 hr in children Indications: Seizures, Panic Disorders Norm. Dosage, Freq, Route, Range: PO 1.5mg/day in 3 divided doses, increased by 0.5-1 q3days until seizures are controlled or until intolerable adverse effects Max: 20 mg/day Side Effects: Drowsiness, sedation, ataxia Nursing Considerations: Monitor for signs of suicidal ideation in depressive individuals, Lab tests: periodic LFTs, platelet counts, blood counts, and renal function tests, Monitor for S&S of overdose, including somnolence, confusion, irritability, sweating, muscle and abdominal cramps, diminished reflexes, coma.
1.12. Gabapentin (Neurontin) Class: Anticonvulsant; Gaba Analog Actions: Used in conjunction with other anticonvulsants to control types of seizure in patients with epilepsy. Effective in controlling painful neuropathies Indications: Seizure disorder, Past-Herpetic Neuralgia, Restless Leg Syndrome Norm. Dosage, Freq, Route, Range: start at 300mg may slowly increase Max: 1,200mg/day Side Effects: drowsiness, fatigue Nursing Considerations: monitor for therapeutic effectiveness, may not occur until several weeks following initiation of therapy, monitor for and report dizziness, somnolence, or other sign of CNS depression
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 9 of 75
Drug Med Cards
1.13. Lamotrigine (Lamictal) Class: Anticonvulsant Actions: may act by inhibiting the release of glutamate and aspartate, excitatory neurotransmitters at voltage-sensitive sodium channels, resulting in decreased seizure activity in the brain. Onset: 12wks. Peak: 1-4hr. Indications: Seizures; Bipolar disorder Norm. Dosage, Freq, Route, Range: PO start w/ 25mg daily for 2 wks, then 50mg daily for 2 wks, then 100mg daily for 1 wk, then 200mg daily (low and slow) Side Effects: dizziness, ataxia, somnolence, headache, nausea, diplopia, blurred vision, Stevens-Johnson syndrome, toxic epidermal necrolysis, rhinitis Nursing Considerations: do not take med if skin rash develops, monitor pts. w/ bipolar disorder for worsening of their symptoms and suicidal ideation, use protection from sunlight or ultraviolet light until tolerance is known
1.14. Levetiracetam (Keppra) Class: Anticonvulsant Actions: The precise mechanism of antiepileptic effects is unknown. Peak: 1hr. Indications: Partial onset Seizures; Tonic Clonic Seizures; Myoclonic Seizures Norm. Dosage, Freq, Route, Range: 3,000mg/day or 1,000 mg/day ER tablet
PO/IV 500mg bid may increase by 500mg bid q2wks. Max:
Side Effects: Asthenia, headache, infection, somnolence, suicidal ideation Nursing Considerations: Lab tests: periodic CBC w/ diff, Hct, and Hgb, LFTs; monitor individuals w/ a history of psychosis or depression for S&S of suicidal tendencies, suicidal ideation, and suicidality
1.15. Oxcarbazepine (Trileptal) Class: Anticonvulsant Actions: Anticonvulsant properties may result from blockage of voltage-sensitive sodium channels, which results in stabilization of hyper-excited neural membranes. Peak: steady-state level reached in 2-3 days Indications: Partial Seizures Norm. Dosage, Freq, Route, Range: PO start w/ 300mg bid and increase by 600mg/day qwk. To 2,400mg/day in 2 divided doses for monotherapy or 1,22mg/day as adjunctive therapy Side Effects: fatigue, nausea, vomiting, abdominal pain, headache, dizziness, somnolence, ataxia, nystagmus, abnormal gait, Stevens-Johnson syndrome, toxic epidermal necrolysis, diplopia, vertigo, abnormal vision Nursing Considerations: Monitor for & report S&S of hyponatremia or CNS impairment; monitor phenytoin levels; Lab tests: periodic serum sodium, T4 level; monitor plasma level
Page 10 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.16. Phenobarbital (Solfoton) Class: Anticonvulsant; Sedative-Hypnotic; Barbiturate Actions: have anticonvulsant properties. Sedative and hypnotic effects appear to be due primarily to interference w/ impulse transmission of cerebral cortex by inhibition of reticular activating system. Limiting the spread of seizure activity results by increasing the threshold of motor cortex stimulation. Peak: PO 812 hr, IV 30 min Duration: IV 4-6 hr Indications: Anticonvulsant, Status Epilepticus, Sedative/Hypmotic Norm. Dosage, Freq, Route, Range: PO/IV 1-3 mg/kg/day in divided doses Side Effects: Somnolence, nightmares, insomnia, “hangover”, headache, anxiety Nursing Considerations: Observe patients receiving large doses for at least 30 min to ensure that sedation is not excessive, keep under observation, check IV site frequently, monitor serum drug levelsgreater than 50 mcg/mL may cause coma, expect restlessness
1.17. Phenytoin (Dilantin) Class: Anticonvulsant; Hydantoin Actions: Anticonvulsant action elevates the seizure threshold and/or limits the spread of seizure discharge. Accompanied by reduced voltage, frequency, and spread of electrical discharges w/in the motor cortex. Peak: Prompt Release: 1.5-3 hr Sustained Release: 4-12 hr Indications: To control tonic-clonic (grand mal) seizures, psychomotor and nonepileptic seizures (ex: Reye’s syndrome). Used to prevent or treat seizures occurring during or after neurosurgery. Not effective for absence seizures. Norm. Dosage, Freq, Route, Range: PO 15-20 mg/kg loading dose than 300 mg/day in 1-3 divided doses, may be gradually increased by 100 mg/week until seizures are controlled IV: 10-15 mg/kg then 300 mg/day in divided doses Side Effects: drowsiness, gingival hyperplasia, thrombocytopenia, leukopenia Nursing Considerations: Monitor Vital signs, Lab tests: periodic serum phenytoin concent., CBC w/ differential, platelet count, Hct, Hgb, serum glucose, serum calcium, serum magnesium, and LFTs
1.18. Pregabalin (Lyrica) Class: Anticonvulsant; Gaba-analog; Analgesic/Miscellaneous; Anxiolytic Actions: an analog of GABA that increases GABA levels and reduces calcium currents in the calcium channels of neurons. Peak: 1.5hr. Half-life:6hr. Indications: management of neuropathic pain associated with diabetic peripheral neuropathy or spinal cord injury, adjunctive therapy for adult patietns w/ partial-onset seizures, management of postherpetic neuralgia, fibromyalgia Norm. Dosage, Freq, Route, Range: PO 50-100mg tid Max: 300mg/day Side Effects: accidental injury, ataxia, dizziness, somnlonce, peripheral edema, weight gain, diplopia, blurry vision Nursing Considerations: Monitor for and report promptly mental status or behavior changes (e.g., anxiety, panic attacks, restlessness, irritability, depression, suicidal thoughts). Monitor for weight gain, peripheral edema and S&S of heart failure. Monitor diabetics for increased incidences of hypoglycemia.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 11 of 75
Drug Med Cards
1.19. Primidone (Mysoline) Class: Anticonvulsant; Barbiturate Actions: effective as an anticonvulsant in all types of seizure disorders except absent seizure. Peak: 4hr Half-life: 3-24hr Indications: management of complex partial and generalized tonic-clonic seizure Norm. Dosage, Freq, Route, Range: PO 250mg/day increased by 250mg/wk Max: 2g/day in 2-4 divided doses Side Effects: drowsiness, sedation, vertigo, ataxia, headache, nausea, vomiting, anorexia, leukopenia, thrombocytopenia Nursing Considerations: Lab tests: baseline and periodic CBC, complete blood chemistry (q6mo), and primidone blood levels (Therapeutic blood levels 5-10 mcg/mL). Monitor primidone plasma levels (concentrations greater than 10mcg/mL are usually associated w/ significant ataxia and lethargy). Observe for S&S of folic acid deficiency: mental dysfunction, psychiatric disorders, neuropathy, and megaloblastic anemia.
1.20. Valproic Acid (Depakote, Depacon, Depakene) Class: Anticonvulsant; GABA inhibitor Actions: Anticonvulsant w/ increased bioavailability of the inhibitory neurotransmitter GABA to brain neurons. Peak: 1-4hrs. Indications: Management of seizures; Migraine headache prophylaxis; Mania Norm. Dosage, Freq, Route, Range: (seizures) PO/IV: 10-15mg/kg/day in divided doses when total is greater than 25mg. increase at 1wk. intervals bu 5-10mg/kg/day until seizures are controlled Max: 60mg/kg/day (Mania) PO: 750mg/day istered in divided doses Side Effects: sedation, drowsiness, deep coma, death (w/ overdose), nausea, vomiting, indigestion, liver failure, pancreatitis, prolonged bleeding time, bone marrow depression Nursing Considerations: Lab tests: baseline platelet count, bleeding time, coagulation, parameters, and serum ammonia, LFTs, then repeat at least q2months of therapy, avoid alcohol
Page 12 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
5.
Vitamins and Minerals
1.21. Multivitamin (One-A-Day) Class: Vitamins Actions: Contain fat-soluble vitamins (A, D and E) and most water-soluble vitamins (B-Complex vitamins B1, B2, B3, B5, B6, B12, Vitamin C, Biotin, and Folic Acid). These vitamins are a diverse group of compounds necessary for growth and development. May act as coenzymes or catalysts in numerous metabolic processes. Onset, Peak, Duration: Unknown Indications: Treatment and prevention of vitamin deficiencies. Norm. Dosage, Freq, Route, Range: recommended by individual manufacturer
1 dose unit (capsule, tablet, dropperful)/day or amount
Side Effects: Urine discoloration, allergic reactions to preservatives, additives, or colorants Nursing Considerations: Asses patient for signs of nutritional deficiency before and throughout therapy.
1.22. Omega-3 Fatty Acids (Fish Oil, Omega-3 Fatty Acids) Class: Nutritional Supplement, Omega-3 Fatty Acids Actions: is not completely understood. May include inhibition of acetyl-CoA and increased peroxisomal beta-oxidation in the liver. Indications: Hypertriglyceridemia Norm. Dosage, Freq, Route, Range: PO 4 g daily as single or divided doses Max: 4 g/day Side Effects: Back pain, flu syndrome, unspecified pain Nursing Considerations: Monitor for S&S of hypersensitivity in those w/ known allergy to fish, Lab tests: baseline and periodic lipid profile
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 13 of 75
Drug Med Cards
6.
Steroid
1.23. Dexamethasone Sodium Phosphate (Baycadron, Decadron, Dexamethasone) Class: Adrenal Corticosteroid; Glucocorticoid Actions: Long-acting synthetic adrenocorticoid with intense anti-inflammatory activity and minimal mineralocorticoid activity. Onset: Rapid Peak: PO 1-2 hr IM 8 hr Duration: PO 2.75 days IM 6 days Intra lesional Intra-articular 1-3 weeks Indications: Allergies, Inflammation, Neoplasias, Adrenocorticol Function Abnormalities, Cerebral Edema, Shock Norm. Dosage, Freq, Route, Range: PO 0.25-4mg bid to qid IM 8-16mg q1-3weeks IV 0.75-0.9mg/kg/day divided q6-12hr. Max: 16mg/day Side Effects: Nasal Irritation, edema, hyperglycemia, impaired wound healing, subacapsular cataract, oral candidiasis Nursing Considerations: take drug exactly as prescribed, report lack ir response to med or malaise, orthostatic hypotension, muscular weakness and pain, nausea, vomiting, anorexia, hypoglycemic reaction, or mental depression to prescriber, report any changes in appearance and easy bruising
1.24. Fluticasone (Flonase, Flovent) Class: Synthetic steroids of glucocorticoid family of drugs Actions: Fluticasone mimics the naturally-occurring hormone produced by the adrenal glands, cortisol or hydrocortisone. The exact mechanism of action of fluticasone is unknown. Fluticasone has potent antiinflammatory actions. Onset: 1-3 wk. Peak: 4-8hr. Indications: Seasonal allergy rhinitis Norm. Dosage, Freq, Route, Range: Intranasal 100 mcg (1 inhalation) per nostril 1-2 times daily Max: 4 times daily Side Effects: transient nasal irritation, burning, sneezing, epitaxis, bloody mucous, nasopharyngeal itching, dryness, crusting, and ulceration, headache, nausea, vomiting Nursing Considerations: oral and nasal inhalers are not to be used interchangeably, use of oral and nasal inhaler provided by manufacturer should be carefully reviewed with patient
1.25. Triamcinolone Acetonide (Nasacort HFA) Class: Adrenal Corticosteroid, Glucocorticoid Actions: Anti-inflammatory and immunosuppressant drug that is effective in the treatment of bronchial asthma. Onset: PO & IM 24-48hr. Peak: PO 1-2hr. IM 8-10hr. Duration: PO 2.25 days IM 1-6wks. Indications: Anti-inflammatory or immunosuppressant agent. Orally inhaled: Bronchial asthma in patient who has responded to conventional inhalation treatment. Does not suppress hypothalamic-pituitaryadrenal axis Norm. Dosage, Freq, Route, Range: Inhaled 2-4 inhalations
IM/SQ/Intra-auricle/Intradermal 4-48 mg/day in divided doses
Side Effects: headache, nausea, vomiting, insomnia, confusion, peptic ulcer Nursing Considerations: notify prescriber if wheezing occurs immediately following a dose, monitor for signs of negative nitrogen balance, lab tests: periodic serum electrolytes and blood glucose
Page 14 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
7.
Opiod
1.26. Fentanyl (Duragesic) Class: Opioid Analgesic Actions: Binds to opiate receptors in the CNS, alters response and perception of pain. Onset: IV immediate, IM min. Transdermal: 12-24hr. Peak: IV 3-5min. Transdermal: 24-72hrs. Duration: IV 30-60min IM 1-2hr. Transdermal 72hrs. Indications: For moderate to severe chronic pain requiring continuous opioid analgesic therapy. Norm. Dosage, Freq, Route, Range: 25-100mcg/hr. for 72hr. transdermal patch Side Effects: CNS depression, do not drink or eat grapefruit, polypharmacy Nursing Considerations: BP, Pulse, Respirations <6 need Narcan
1.27. Hydrocodone Bitartrate (Mycodone) Class: Narcotic (Opiate Agonist) Analgesic; Antitussive Actions: CNS suppressant with moderate to severe pain relief of pain. Suppress cough reflex by direct action on cough center in medulla. Onset: 10-20 min Duration: 3-6 hr Indications: Mild to Moderate pain, Cough Norm. Dosage, Freq, Route, Range: 5-10 mg q4-6hr PRN Max: 60 mg/day Side Effects: constipation, nausea, drowsiness, respiratory depression Nursing Considerations: Monitor for effectiveness of drug for pain relief, nausea and vomiting, respiratory status and bowel elimination
1.28. Hydromorphone (Dilaudid) Class: Narcotic, Analgesic Actions: Potent opiate receptor agonist that does not alter pain threshold but changes the perception of pain in CNS. An effective narcotic analgesic that controls mild to moderate pain; has antitussive properties. Onset: IV 15min., PO 30min. Peak: 30-90min. Duration: 3-4hrs. Indications: Relief of moderate to severe pain Norm. Dosage, Freq, Route, Range: PO 2.5-10 mg q4-6hr Max: 60mg/day SQ/IM/IV 0.75-2 mg q4-6hr Max: 12 mg/day Side Effects: depression
Nausea, vomiting, constipation, drowsiness, hypotension, tachycardia, respiratory
Nursing Considerations: Baseline respiratory rate, rhythm, and depth & size of pupils;; respirations ↓ 12/min. or less & mitosis are signs of toxicity, monitor vital signs at reg. intervals, monitor I&O ratio & pattern for urinary retention, monitor bowel pattern, √ for nausea/vomiting and orthostatic hypotension.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 15 of 75
Drug Med Cards
1.29. Morphine Sulfate (Astramorph PF, Avinza, Depo-Dur, Duromorph) Class: Analgesic, Narcotic (opiate agonist) Actions: Controls severe pain, also used as an adjunct to anesthesia. Peak: PO 60min. PR 20-60min. SQ 30-60min. IM 30-60min. IV 20min. Duration: 7hr. Indications: Pain relief Norm. Dosage, Freq, Route, Range: PO 10-30 mg q4hr or 15-30 mg sustained release q8-12hr Max: 180 mg/day IV 2.5-15 mg/70kg q2-4hr or 0.8-10 mg/hr by continuous infusion, may increase PRN to control pain or 5-10 mg given epidurally q24hr IM/SQ 5-20 mg q4hr PRN Max: 120 mg/day PR10-20 mg q4hr PRN Max: 120 mg/day Side Effects: hypersensitivity, nausea, vomiting, constipation, urinary retention Nursing Considerations: Baseline respiratory rate, rhythm and depth and size of pupils, respirations 12/min and ↓and miosis are signs of toxicity, assess vital signs at regular intervals, encourage changes in positions, deep breathing, and coughing at regular intervals, Monitor I&O, √ for nausea and orthostatic hypotension
1.30. Oxycontin Class: Narcotic (opiate agonist); Analgesic Actions: Semisynthetic derivative of an opium agonist the binds with stereo-specific receptors in various sites of CNS to alter both perception of pain and emotional response to pain. Onset: 10-15 min. Peak: 3060 min. Duration: 4-5 hr. Indications: Moderate to severe pain Norm. Dosage, Freq, Route, Range: PO 5-10 mg q6hr (may titrate up to 10-30 mg q4hr PRN) Immediaterelease 10 mg q12hr (may titrate up) Max: 180 mg/day Side Effects: sedation, constipation, light-headedness, dizziness, fainting, hepatotoxicity Nursing Considerations: Monitor patient’s response closely, especially to sustained-release preparations, Lab tests: monitor LFTs and hematologic status periodically in patients on high dose, evaluate patients continued need
Page 16 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
8.
Opiod Antagonists
1.31. Naloxone (Narcan) Class: Opioid Antagonist Actions: A potent narcotic antagonist, essentially free of agonistic (morphine-like) properties. Reverses the effects of opiates, including respiratory depression, sedation, and hypotension. Onset: 2 min Duration: 45 min Indications: Opiate Overdose Norm. Dosage, Freq, Route, Range: IV 0.4-2mg, may repeat q2-3min up to 10mg if necessary Max: 10mg Side Effects: increased BP, tachycardia, nausea, vomiting Nursing Considerations: Observe patient closely; duration of action of some narcotics may exceed that of naloxone. Keep prescriber informed
1.32. Naltrexone HCL (Vivitrol) Class: Narcotic (opiate Antagonist) Actions: Weakens or completely and reversibly blocks the subjective effects (the “high”) of IV opioids and analgesics possessing both agonist and antagonist activity. Onset: 15-30min Peak: 1hr. Duration: PO 2472hr. IM 4wk. Indications: Opioid Dependence; Alcohol Dependence Norm. Dosage, Freq, Route, Range: PO 25mg followed by another 25mg in 1hr. if no withdrawal response; maintenance regimen of 50-150mg/day is individualized Max: 800mg/day IM 380mg q4wk Side Effects: nausea, vomiting, abdominal cramps/pain, hepatotoxicity, muscle & t pains, difficulty sleeping, anxiety, headache, nervousness Nursing Considerations: Lab tests: check LFTs before the treatment is started, at monthly intervals for 6 months, and then periodically as indicated; do not self-medicate w/ OTC drugs; report promptly onset of signs of hepatic toxicity to prescriber
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 17 of 75
Drug Med Cards
9.
NSAIDS
1.33. Celecoxib (Celebrex) Class: Analgesic; NSAID; Cyclooxygenase-2 (Cox-2) Inhibitor; Anti-inflammatory Actions: Exhibits anti-inflammatory; analgesic, and antipyretic activities. Reduces or eliminates the pain of rheumatoid and osteoarthritis. Peak: 3 hr Indications: Osteoarthritis/Arthritis/Ankylosing Spondylitis, Rheumatoid Arthritis Norm. Dosage, Freq, Route, Range: PO 100mg bid Max: 200mg Side Effects: back pain, dizziness, headache, insomnia, diarrhea, abdominal pain Nursing Considerations: Lab tests: periodically monitor Hct and Hgb, Lfts, BUN, and Creatinine and serum electrolytes, monitor closely lithium levels, monitor closely PT/INR, monitor for fluid retention and edema
1.34. Indomethacin (Indocin) Class: Analgesic, Non-steroidal Anti-inflammatory (NSAID) Actions: It is a potent analgesic, anti-inflammatory, and antipyretic agent. Promotes closure of persistent patent ductus arteriosus. Onset 1-2 hr. Peak: 3 hr. Duration: 4-6 hr. Indications: palliative treatment in active stages of moderate to severe rheumatoid arthritis, ankylosing rheumatoid spondylitis, acute gouty arthritis, and osteoarthritis of hip in patients intolerant to or unresponsive to adequate trials with salicylates and other therapy. Also used IV to close patent ducus arteriosus in the premature infant. Norm. Dosage, Freq, Route, Range: PO/PR: 50 mg tid until pain is tolerable, then rapidly taper Max: 150 mg/day Side Effects: dizziness, tinnitus, nausea, vomiting Nursing Considerations: Monitor for effectiveness, question patient carefully regarding aspirin sensitivity before initiation of therapy, observe patients carefully, Lab tests: monitor renal function, LFTs, CBC w/ differential, BP and HR, visual and hearing acuity periodically
1.35. Ketorolac (Acular, Acuvail, SPRIX) Class: Analgesic, NSAID, Anti-inflammatory, Antipyretic Actions: It inhibits synthesis of prostaglandins by inhibiting both COX-1 and COX-2 enzymes. Is a peripherally acting analgesic. It inhibits platelet aggregation and prolongs bleeding time. Peak: 46-60 min Indications: Pain Norm. Dosage, Freq, Route, Range: IV loading dose 30mg Max: 150mg/day on the first day then 120mg/day subsequent days Side Effects: drowsiness, nausea Nursing Considerations: Lab tests: periodic serum electrolytes and LFTs; urinalysis (for hematuria and proteinuria) with long-term use, monitor urine output, monitor for S&S of GI distress or bleeding including nausea, GI pain, diarrhea, melena, or hematemesis, GI ulceration with perforation can occur anytime during treatment
Page 18 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
10. Analgesic, Antipyretic 1.36. Acetominophen (Tylenol) Class: Nonnarcotic analgesic, Antipyretic Actions: provides temp. relief for mild to mod. pain, ↓ body temp. in indiv. w/ fever. Peak: 0.5-2 hr. Duration: 3-4 hr. Indications: Fever Reduction. Temporary relief of mild to moderate pain. Generally as substitute for aspirin when the latter is not tolerated or is contraindicated Norm. Dosage, Freq, Route, Range: PO: 325-650 mg q4h Max: 4 g/day PR: 650 mg q4h Max: 4 g/day Side Effects: Hepatotoxicity, hepatic coma, acute renal failure Nursing Considerations: Hepatotoxicity, even w/ mod. acetaminophen doses, especially in individuals with poor nutrition or who have ingested alcohol (3+ drinks daily) over prolonged periods; poisoning, usually from accidental ingestion or suicide attempts; potential abuse from psychological depend., do not take other meds containing acetaminophen, do not self-medicate adults for pain more than 10 days w/o consulting a doctor, do not use this med w/o medical direction for: fever persisting longer than 3 days, fever over 103, or recurrent fever
1.37. Acetaminophen Suppository (Tylenol Suppository) Class: Antipyretic, Non-opioid Analgesic Actions: Analgesic; Antipyresis. Peak: 0.5-2hrs. Duration: 3-4hrs. Indications: Mild pain, fever Norm. Dosage, Freq, Route, Range: PR 325-650mg q4-6hr. or 1gram 3xday Side Effects: Hepatic failure, renal failure, neutropenia, rash urticaria Nursing Considerations: Polypharmacy, renal-liver function, pain level, toxicity
1.38. Aspirin (ASA) Class: Non-narcotic, Antiplatelet, Antipyretic Actions: inhibiting the formation of prostaglandins involved in the production of inflammation, pain and fever, powerfully inhibits platelet aggregation. High serum salicylate concentrations can impair hepatic synthesis of blood coagulation factors VII, IX, X. Peak: 15min-2hr. Indications: Anti-inflammatory action, pain, fever reducer, antiplatelet Norm. Dosage, Freq, Route, Range: PO: 350-650 mg q4h Max: 4 g/day Side Effects: Bronchospasm, anaphylactic shock (laryngeal edema), nausea, heartburn, stomach pains, thrombocytopenia, hemolytic anemia Nursing Considerations: Allergy to any ASA, monitor for salicylate toxicity. In adults, a sensation of fullness in the ears, tinnitus, and decreased or muffled hearing are the most frequent symptoms.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 19 of 75
Drug Med Cards
11. Anticholinergic 1.39. Oxybutynin Cl (Anutrol, Ditropan, Gelnique, Oxytrol) Class: Anticholinergic; Antimuscaring; GU Antispasmodic Actions: Synthetic tertiary amine that exerts direct antispasmodic action and inhibits muscarinic effects of acetylcholine on smooth muscle of the urinary muscle. Onset: 0.5-1hr. Peak: 3-6hrs. Duration: 6-10hrs. Indications: Overactive Bladder Norm. Dosage, Freq, Route, Range: PO 5mg 2-4x/day Max: 20mg/day Side Effects: drowsiness, blurred vision, dry mouth, constipation, pruritus at application site (topical) Nursing Considerations: periodic interruptions of therapy are recommended to determine pt.’s need for continued treatment, tolerance has occurred in some pt.’s;; keep prescriber informed of expected responses to drug therapy (e.g., effect on urinary frequency, urgency, urge incontinence, nocturia, completeness of bladder emptying)
1.40. Glycopyrrolate (Robinul, Robinul Forte) Class: Anticholinergic, Antimuscarinic, Antipasmodic Actions: Inhibits motility of GI and genitourinary tract, it also decreases volume of gastric and pancreatic secretions, saliva, and perspiration. Onset: PO: 1 hr., IV: 1 min., IM/SQ: 15-30 min Peak: PO: 1 hr., IM/SQ: 30-45 min. Duration: PO: 8/12 hr., IM/SQ: 2-7 hr. Indications: Adjunctive management of peptic ulcer and other GI disorders associated with hyperacidity Norm. Dosage, Freq, Route, Range: PO: 1 mg tid or 2 mg bid or tid in equally divided intervals Max; 8 mg/day Side Effects: Decreased sweating, Xerostomia, Urinary hesitancy or retention Nursing Considerations: Monitor I&O ratio and pattern particularly in older adults, Monitor vital signs, especially when drug is given parenterally. Report any changes in heart rate and rhythym.
Page 20 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
12. Bronchodilator 1.41. Albuterol (Proventil, Ventolin) Class: Bronchodilator (Resp. Smooth Muscle Relaxant); Beta-Adrenergic Agonist Actions: Bronchodilation decreased airway resistance; facilitates mucous drainage, and increases vital capacity. Onset: Inhaled 5-15 min PO 30 min Peak: 0.5-2 hr PO 2.5 hr Duration: inhaled3-6 hr PO 4-6 hr (8-12hr w/ sustained release) Indications: Bronchospasm Norm. Dosage, Freq, Route, Range: PO 2-4 times/day, 4-8 mg sustained release 2 times/day Inhaled: 1-2 inhalations q4-6hr Side Effects: Tremor, anxiety, nervousness, headache, restlessness Nursing Considerations: Monitor effectiveness, Monitor S&S of fine tremor in fingers, Lab Tests: periodic ABGs, PFTs, pulse oximetry
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 21 of 75
Drug Med Cards
13. Thyroid Hormone Replacement 1.42. Levothyroxine (Synthroid) Class: Thyroid Hormone Replacement Actions: Raises T3 and T4 levels, Normal levels: 0.3-3, Restores metabolic rate. Peak: 3-4wks. Duration: 1-3wks. Indications: Specific replacement therapy for diminished or absent thyroid function Norm. Dosage, Freq, Route, Range: PO 25-50 mcg/day Max: 400 mcg/day Side Effects: insomnia, headache, irritability, nervousness, palpitations Nursing Considerations: monitor T3, & T4 levels, H.R., B.P., PT/INR
Page 22 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
14. Alpha Adronergic Receptor Antagonist 1.43. Tamsulosin HCL (Flomax) Class: Alpha Adrenergic Receptor Antagonist Actions: effectiveness is indicated by improved voiding. Improves symptoms related to BPH related to bladder outlet obstruction. Peak: 4-5hr. fasting 6-7hr. fed Half-life: 14-15hr. Indications: BPH Norm. Dosage, Freq, Route, Range: PO 0.4mg daily 30 min after meal Max 0.8mg/day Side Effects: headache, dizziness, orthostatic hypotension, rhinitis, abnormal ejaculation Nursing Considerations: Monitor for signs of orthostatic hypotension
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 23 of 75
Drug Med Cards
15. Antiparkinson (Cholinergic Receptor Antagonist 1.44. Benztropine Mesylate (Cogentin) Class: Centrally Acting Cholinergic Receptor Antagonist; Antiparkinson Actions: Synthetic centrally acting anticholinergic agent that acts by diminishing excess cholinergic effects associated w/ dopamine deficiency. Onset: IM/IV 15min. PO 1hr. Duration: 6-10hrs. Indications: Parkinsonism; Extrapyramidal reactions; Acute Dystonia Norm. Dosage, Freq, Route, Range: PO/IM 0.5-1mg/day may gradually increase as needed up to 6mg/day Side Effects: sedation, constipation, dry mouth, paralytic ileus Nursing Considerations: Monitor I&O ratio and pattern, monitor HR, monitor and report for muscle weakness
1.45. Donepezil (Aricept) Class: Central Acting Cholinergic; Cholinesterase Inhibitor Actions: improves global function, cognition, and behavior of patients with mild to moderate Alzheimer’s. Peak: 3-4hr. Half-life: 70hr. Indications: mild, moderate, or severe dementia of Alzheimer’s type. Norm. Dosage, Freq, Route, Range: PO 5-10mg at bedtime Max: 10mg/day Side Effects: headache, insomnia, nausea, diarrhea, vomiting, muscle cramps, anorexia Nursing Considerations: Monitor closely for S&S of GI ulceration and bleeding, monitor cardiovascular status, exercise caution
1.46. Ropinirole HCL (Requip) Class: Dopamine Receptor Agonist; Antiparkinson Actions: effectiveness indicated by improvement in idiopathic Parkinson’s disease. Peak: 1-2hr. Half-life: 6hr. Indications: Idiopathic Parkinson’s disease, restless leg syndrome Norm. Dosage, Freq, Route, Range: PO 0.25-4mg Max: 4mg Side Effects: fatigue, viral infection, dizziness, somnolence, sudden sleep attacks, syncope, nausea, vomiting, dyspepsia Nursing Considerations: Lab tests: periodically monitor BUN and creatinine, hepatic function and cardiac status
Page 24 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.47. Trihexyphenidyl HCL (Artane) Class: Centrally Acting Cholinergic Receptor Antagonist; Antiparkinson Agent; Antispasmodic Actions: thought to act by blocking excess of acetylcholine at certain cerebral synaptic sites. Relaxes smooth muscle by direct effect and by atropinelike blocking action on the PNS. Onset: w/in 1 hr. Peak: 23hr. Duration: 6-12hrs. Indications: Parkinsonism; Extrapyramidal reactions Norm. Dosage, Freq, Route, Range: PO 1mg day 1, 2mg day 2 then increased 2mgq3-5days up to 610mg/day in 3 or more divided doses Max: 15mg/day Side Effects: dry mouth, nausea, blurred vision, dizziness, nervousness Nursing Considerations: Monitor vital signs, assess and report severe CNS stimulation, monitor daily I&O if pt. develops urinary hesitancy
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 25 of 75
Drug Med Cards
16. Fluid and Electrolytes 1.48. Calcium Acetate (Norvasc) Class: Calcium Channel Blocker; Antihypertenive Actions: reduces systolic, diastolic, and mean arterial blood pressure. It also decreases pain due to angina. Peak: 6-9hr. Duration: 24hr. Half-life: less than 45yrs: 28-69hr. greater than 60yrs: 40-120hr. Indications: treatment of mild to moderate hypertension and stable angina Norm. Dosage, Freq, Route, Range: PO 5-10mg once daily Max: 10mg Side Effects: peripheral or facial edema, headache, abdominal pain, nausea Nursing Considerations: Monitor BP& HR, monitor for S&S of dose-related peripheral or facial edema, monitor BP w/ postural changes
1.49. Dextrose 50% (Dextrose, D50, D50W, Glucose) Class: Monosaccharide, principal form of charbohydrate used in the body Actions: Increase blood serum glucose levels. Onset: 5-20min Indications: hypoglycemia, coma or seizure of unknown etiology, refractory cardiac arrest Norm. Dosage, Freq, Route, Range: ½ to 1 full amp slow IV (25-100mL of 50% solution) Side Effects: pain, warmth, burning upon , phlebitis, sclerosis, thrombosis, Nursing Considerations: if smaller veins are used, local venous irritation may occur, infiltration may cause necrosis
1.50. Ergocalciferol (Calcidol, D-ViSol, Vitamin D2) Class: Vitamin D Analog Actions: distributed through the circulation and plays a major regulatory role. Responsible for regulation of serum calcium level. Indications: Nutritional Rickets, Osteomalacia, Hypoparathyroidism Norm. Dosage, Freq, Route, Range: PO 25-125 mcg/day for 6-12 weeks; may need to increase to 7.5 mg/day in patients w/ malabsorption. Peak: after 4 weeks Duration: 2 months or more. Side Effects: fatigue, weakness, vertigo, tinnitus, ataxia, muscle and t pain Nursing Considerations: Monitor closely patients receiving therapeutic doses of Vitamin D, must remain under close medical supervision, Lab tests: Serum calcium, phosphorus, magnesium, alkaline, phosphatase, BUN, periodic urine calcium, casts, albumin, and RBC, Monitor for hypercalcemia
Page 26 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.51. Ferrous Sulfate (Feosol) Class: Iron prepartion Actions: Standard iron preparation that corrects erythropoietic abnormalities induced by iron deficiency but does not stimulate erythropoiesis. Absorption: 5-10% absorbed in healthy individuals; 10-30% absorbed in iron deficiency; food decreases amount absorbed Indications: Iron deficiency, Iron supplement Norm. Dosage, Freq, Route, Range: PO 750-1500 mg/day in 1-3 divided doses Max: 1500 mg Side Effects: nausea, heartburn, constipation, black stools Nursing Considerations: Lab tests: monitor Hgb and reticulocyte values during therapy, continue iron therapy for 2-3 months after the hemoglobin level has returned to normal, monitor bowel movements as constipation is common
1.52. Magnesium Hydroxide (Magnesia, Magnesia Magna, Milk of Magnesia, M.O.M.) Class: Saline Cathartic; Antaid Actions: Aqueous suspension of magnesium hydroxide w/ rapid and long-acting neutralizing action. Causes osmotic retention of fluid, which distends colon, resulting in mechanical stimulation of peristaltic activity. Onset: 3-6hrs. Indications: Laxative Norm. Dosage, Freq, Route, Range: PO 2.4-4.8g/day (30-60mL) in 1 or more divided doses. Side Effects: nausea, diarrhea, complete heart block, other ECG abnormalities, respiratory depression, coma Nursing Considerations: Lab tests: monitor serum magnesium w/ signs of hypermagnesemia such as bradycardia, especially w/ frequent use of any degree of renal impairment
1.53. Potassium Chloride (KCl) Class: Electrolytes replacement solution Actions: For maintenance of intracellular isotonicity, transmission of nerve impulses, contraction of cardiac, skeletal and smooth muscles, normal kidney function and enzyme activity Indications: Potassium replacement Norm. Dosage, Freq, Route, Range: PO 10-100 mEq/day in divided doses Max: 100 mEq/day in divided doses Side Effects: Bacteremia, dizziness, edema, fatigue, fever, headache, infection, insomnia, rigors, hypertension, hypotension, tachycardia, abdominal pain, anorexia, constipation, diarrhea, dyspepsia, mucositis, nausea, anemia, febrile neutropenia, neutropenia, petechiae, thrombocytopenia, bilirubinemia, hyperglycemia, hypokalemia, hypomagnesemia, arthralgia, back pain, musculoskeletal pain, cough, dyspnea, epistaxis, pharyngitis, pruritus, rash, vaginal hemorrhage Nursing Considerations: Check serum K+ level, Normal level: 3.5-5.0, monitor I&O renal function
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 27 of 75
Drug Med Cards
17. Antibiotics 1.54. Amoxicillin & Clavulanic Acid (Augmentin) Class: Beta-Lactam, Antibiotic, Aminopenicillin Actions: Inhibits the final stage of bacterial cell wall synthesis , which leads to cell lysis and death. Peak: 1-2hrs. Indications: Infections caused by susceptible beta-lactamase-producing organisms, lower respiratory tract infections, acute bacterial sinusitis, community acquired pneumonia, otitis media, sinusitis, skin and skin structure infections, UTI Norm. Dosage, Freq, Route, Range: PO: 250-500 mg tablet Max:1500 mg/day Side Effects: Diarrhea, agranulocytosis (rare) Nursing Considerations: determine previous hypersensitivity reactions to penicillins, cephalosporins and other allergens prior to therapy, Lab tests: baseline C&S prior to initiation of therapy; start drug pending results, monitor for S&S of an urticarial rash (usually occurring within a few days after start of drug) suggestive of a hypersensitivity reaction, monitor for and report diarrhea which may indicate pseudomembranous colitis
1.55. Amoxicillin (Amoxil) Class: Antibiotic, Aminopenicillin Actions: Inhibits the final stage of bacterial cell wall synthesis, which results in bacterial cell lysis and death. Active against both aerobic gram-positive & aerobic gram negative bacteria. Onset: 1-2hr. Duration: 1-1.3hr. Indications: mild to moderate infections of ear, nose, throat, GU tract, skin, and soft tissue caused by susceptible bacteria, used in uncomplicated Gonorrhea Norm. Dosage, Freq, Route, Range: PO 250-500 mg q8h Max: 60-80 mg/kg/day Side Effects: Anaphaylaxis, pseudomembranous colitis (rare), agranulocytosis (rare), hypersensitivity Nursing Considerations: determine previous hypersensitivity reactions to penicillins, cephalosporins and other allergens prior to therapy, Lab tests: Baseline C&S tests prior to initiation of therapy; start drug pending results, periodic assessment of renal, hepatic and hematologic functions w/ prolonged therapy.
1.56. Ampicillin (Principen) Class: Antibiotic; Aminopenicillin Actions: A broad-spectrum, semi synthetic aminopenicillin that is bactericidal but is inactivated by penicillinase. Inhibits final stage of bacterial cell wall synthesis by binding to specific penicillin-binding proteins located inside the bacteria cell wall resulting in lysis and death of bacteria. Peak: Immed. After IV Duration: 6-8hrs. Indications: Infections of the GU, respiratory and GI tracts, and skin and soft tissues; gonococcal infections, bacterial meningitis, otitis media, sinusitis and septicemia and for prophylaxis of bacterial endocarditis. Used parentally only for moderately severe to severe infections. Norm. Dosage, Freq, Route, Range: PO/IV/IM 250-500 mg q6hr Max: 2000 mg/day Side Effects: Diarrhea, nausea, vomiting, rash
Page 28 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards Nursing Considerations: √ for allergies to penicillin’s, cephalosporin’s and other allergens prior to therapy, monitor closely for signs of hypersensitivity during the first 30 min. after ., Lab tests: baseline C&S prior to ., baseline & periodic renal assessment, monitor for diarrhea (may indicate pseudomembranous colitis)
1.57. Ceftriaxone Sodium (Rocephin) Class: Antibiotic, 3rd generation Cephalosporin Actions: preferentially binds to one or more of the penicillin-binding proteins located on the cell walls on susceptible organisms. Peak: 1.5-4hr after IM, immediately after IV Half-life: 5-10hr Indications: infections in lower respiratory tract, skin and skin structures, urinary tract, bones and ts, intra-abdominal infections, pelvic inflammatory disease, uncomplicated gonorrhea, meningitis, and surgical prophylaxis Norm. Dosage, Freq, Route, Range: IV/IM: 1-2g q12hr x 4-14days Max: 4g/day Side Effects: diarrhea, abdominal cramps Nursing Considerations: hypersensitivity, Lab tests: culture & sensitivity before initiation of therapy, periodic PT & INR, report diarrhea promptly
1.58. Clindamycin HCL (Cleocin) Class: Lincosamide Antibiotic Actions: Semisynthetic derivative if lincomycin that suppresses protein synthesis by binding to 50 S subunits of bacterial ribosomes, and, therefore, inhibits other antibiotics (ex: erythromycin) that act at this site. Peak: PO 45-60 min IM 3 hr Duration: PO 6 hr IM 8-12 hr Indications: Moderate to severe infections, Acne Vulgaris, Bacterial Vaginosis Norm. Dosage, Freq, Route, Range: PO 150-450 mg q6hr IM/IV 600-1,200 mg/day in divided doses Max: 2,700 mg/day Side Effects: Diarrhea, nausea, vomiting, skin rashes Nursing Considerations: Lab tests: C&S susceptibility testing should be performed initially, periodic CBC with differential, liver and kidney function tests, monitor BP and pulse in patients receiving drug parenterally, report diarrhea immediately with or w/o fever, be alert for signs of superinfection and anaphylactoid reactions
1.59. Cortisporin gtts (Cortisporin-TC) Class: Ophthalmic steroid, antibiotic (Suspension Only) Actions: Ear drops used to treat outer ear infections caused by bacteria (aka swimmer's ear). Contains neomycin and colistin, which are antibiotics that work by stopping the growth of bacteria. Also contains hydrocortisone, which is an anti-inflammatory corticosteroid that works by reducing ear swelling and discomfort, and thonzonium, which helps this med through dead cells and pus inside the ear. Indications: Only works for bacterial ear indications Norm. Dosage, Freq, Route, Range: 4 drops in affected ear 3-4 times daily Max: 16 drops/day Side Effects: This medication may temporarily sting or burn your ear for a minute or two when applied. Hearing problems, rash, itching/swelling, redness of the ears, dizziness Nursing Considerations: √ for allergies, rash, redness, itching or swelling to the ears, or any hearing problems
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 29 of 75
Drug Med Cards
1.60. Doxycycline Hyclate (Doryx, Doxy) Class: Antibiotic; Tetracycline Actions: blocks the binding of transfer RNA to the messenger RNA of bacteria, resulting in inhibition of bacterial protein synthesis. Peak: 1.5-4hr Half-life 14-24hr Indications: treatment of chlamydial and mycoplamal infections, gonorrhea, syphilis in penicillin-allergic patients, rickettsial diseases, acute exacerbations of chronic bronchitis Norm. Dosage, Freq, Route, Range: PO/IV 100mg q12hr on day 1, than 100mg/day as single dose Max: 100mg/q12hr Side Effects: nausea, vomiting, diarrhea Nursing Considerations: superinfections
report sudden onset of painful or difficult swallowing and evidence of
1.61. Gentamicin Ointment (Garamycin Ophthalmic) Class: Aminoglycoside Antibiotic Actions: Active against a wide variety of aerobic gram-negative but not anaerobic gram-negative bacteria. Also effective against certain gram-positive organisms, particularly penicillin-sensitive bacteria Indications: Moderate to Severe Infection Norm. Dosage, Freq, Route, Range: Topical 1-2 drops of solution in eye q4hr up to 2 drops q1hr or small amount of ointment bid or tid Side Effects: decreased creatinine clearance Nursing Considerations: Lab tests: perform C&S and renal function prior to first dose and periodically during therapy, watch Creatinine clearance levels, report S&S of ototoxic effect
1.62. Levofloxacin (Levaquin, Iquix, Quixin) Class: Quinolone Antibiotic Actions: A broad-spectum fluoroquinolone antibiotic that inhibits DNA-gyrase, an enzyme necessary for bacterial replication, transcription, repair, and recombination. Peak: PO 1-2 hr. Half-life: 6-8 hr. Indications: treatment of maxillary sinusitis, acute exacerbations of bacterial bronchitis, communityacquired pneumonia, uncomplicated skin/skin structure infections, UTI, acute pyelonephritis caused by susceptible bacteria, acute bacterial sinusitis, chronic bacterial prostatitis, nd bacterial conjunctivitis, treatment of pneumonic and septicemic plague. Norm. Dosage, Freq, Route, Range: PO: 500 mg q24hr x 10 days Side Effects: abdominal pain, nausea, headache, depression Nursing Considerations: Monitor for decreases pulse, perspiration, or pallor during insertion. Keep patient supine until these signs disappear, Monitor BP
Page 30 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.63. Linezolid (Zyvox) Class: Oxazolidinone Antibiotic Actions: Synthetic antibiotic that binds to a site on the 23S ribosomal RNA of bacteria, which prevents the bacterial RNA translation process, thus preventing further growth. Peak: PO 1-2 hr. Half-life: 6-7 hr. Indications: Vancomycin-Resistant Enterococcus faecium, pneumonia, complicated and uncomplicated skin infections
Nosocomial
or
community-acquired
Norm. Dosage, Freq, Route, Range: PO/IV: 600 mg q12hr x 14-28 days Max: 1,200 mg/day Side Effects: diarrhea, nausea, vomiting, constipation, taste alteration Nursing Considerations: Monitor S&S of bleeding, hypertension, or pseudomembranous colitis that begins w/ diarrhea, Lab tests: CBC, platelet count, Hgb, and Hct
1.64. Ofloxacin (Floxin) Class: Quinolone Antibiotic Actions: Inhibits DNA gyrase, an enzyme needed for bacterial DNA replication, broad spectrum against gram +&- most effective against gram – aerobic and anaerobic bacteria. Peak 1-2hr. Half-life: 5-7.5hr. Indications: Gonorrhea; Prosistitis; RTI (PO) OTIC (Tympanic) and Ocular; PID Norm. Dosage, Freq, Route, Range: 0.3% Opthalmic solution 1-2GTTs q2-4hr, qid 0.3% Otic solution GTTS q12hr. x days Side Effects: Dizziness, N&V, DTS menorrhea, menorrhagia, dysuria, urinary frequency Nursing Considerations: C&S, tendon PN, rash, seizures, S&S super infection
1.65. Vancomycin (Vancocin) Class: Antibiotic, Bacteriocidal Actions: Active against many gram-positive organisms. Inhibits cell-wall biosynthesis and alteration of bacterial cell-membrane permeability and RNA synthesis. Peak: 30min after end of infusion Half-life: 4-8hr. Indications: Infections Norm. Dosage, Freq, Route, Range: (C. Diff.) PO 125-500 mg q6h (Staph) PO 500 mg-2 g in 3-4 divided doses x 7-10 days Max: 2 g/day Side Effects: Nephrotoxicity leading to uremia, shock-like state, anaphylactoid reaction w/ vascular collapse, leukopenia, hypotension accompanied by flushing and erythematous rash on face and upper body (red-man syndrome) following rapid IV infusion Nursing Considerations: Allergy, monitor BP and HR, take peak & trough levels, assess hearing. Be aware that serum levels of 60-80 mcg/ml are associated w/ ototoxicity, monitor I&O. Oliguria or cloudy or pink urine may be a sign of nephrotoxicity
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 31 of 75
Drug Med Cards
18. Cholesterol Lowering Agents 1.66. Atorvastatin (Lipitor) Class: Anti-lipemic, HMG-COA, Reductase Inhibitor (statin) Actions: Adjunct to diet for reduction of LDL cholesterol and triglycerides in patients with primary hypercholesterolemia and mixed dyslipidemia, prevention of cardiovascular disease in patients with multiple risk factors. Onset: 2 wk. Peak: Plasma concentration 1-2 hr. effect 2-4 wk. Indications: Lowers LDL cholesterol, prevention of cardiovascular disease Norm. Dosage, Freq, Route, Range: PO start w/ 10-40 mg daily may increase up to 80 mg/day Max: 80 mg/day Side Effects: Back pain, hypersensitivity reaction, headache, abd. pain, constipation, diarrhea, flatulence, increased liver function tests, sinusitis, pharyngitis, rash Nursing Considerations: Lab tests: monitor lipid levels within 2-4 weeks after initiation of therapy or upon change in dosage, assess muscle pain, tenderness or weakness and if present, monitor K level (d/c drug with marked elevations of K or if myopathy is suspected, monitor carefully for digoxin toxicity with concurrent digoxin use, monitor prediabetics and diabetics for loss of glycemia.
1.67. Cholestyramine (Questrane, Prevalite) Class: Antilipemic; Bile Acid Sequestrant Actions: increase fecal loss of bile acids, which leads to lowered serum total cholesterol by decreasing LDL cholesterol, and reducing bile acid deposit in dermal tissues. Indications: as adjunct to diet therapy in management of patients w/ primary hypercholesterolemia w/ a significant risk of atherosclerotic heart disease and MI; for relief of pruritus secondary to partial biliary stasis Norm. Dosage, Freq, Route, Range: PO 4-8g bid to qid and before meals and at bedtime Max: 32g/day Side Effects: constipation, flatulence, abdominal pain Nursing Considerations: membranes, tarry stools
Monitor for petechiae, ecchymoses, abnormal bleeding from mucous
1.68. Fenofibrate (Tricor) Class: Antilipemic; Fibrate Actions: Fibric acid derivative w/ lipid-regulating properties. Lowers plasma triglycerides by inhibiting triglycerides synthesis and, as a result, lowers VLDL production as well as stimulates the catabolism of triglyceride-rich lipoprotein. Produces a moderate increase of HDL cholesterol levels in most patients. Peak: 6-8 hr. Half-life: 20 hr. Indications: Hypertriglyceridemia Norm. Dosage, Freq, Route, Range: PO 43-200 mg/day depending on product Max: 200 mg/day Side Effects: fatigue, headache, nausea, vomiting, flatulence, constipation Nursing Considerations: La tests: periodically monitor lipid levels, LFTs, and CBC w/ differential, assess for muscle pain, tenderness or weakness and if present monitor K level.
Page 32 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.69. Niacin (Niacor, Niaspan) Class: Vitamin B3; Antilipemic Actions: produces vasodilation by direct action on vascular smooth muscles. Inhibits hepatic synthesis of VLDL, cholesterol, and triglyceride, and indirectly LDL. Peak: 20-70 min. Half-life: 45 min. Indications: Niacin deficiency, Pellagra, Hyperlipidemia Norm. Dosage, Freq, Route, Range: PO 10-20 mg/day (Niacin Deficiency) 1.5-3g/day in divided doses, may increase up to 6 g/day if necessary (Hyperlipidemia) Max: 6 g/day Side Effects: headache, tingling, flushing with sensation of warmth, bloating, flatulence, itchy palms Nursing Considerations: monitor therapeutic effectiveness, Lab tests: obtain baseline and periodic blood glucose and LFTs in patients receiving prolonged high dose therapy, monitor diabetics, and monitor closely for evidence of liver dysfunction
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 33 of 75
Drug Med Cards
19. Laxatives/ Stool Softeners 1.70. Bisacodyl Suppository (Dulcolax) Class: Stimulant Laxative Actions: Expands intestinal fluid volume by increasing epithelial permeability. Induces peristaltic contractions by direct stimulation of sensory nerve endings in the colonic wall. Onset: PO 6-8hrs. PR 1560min. Indications: Temporary relief of acute constipation and for evacuation of colon before GI procedures. Norm. Dosage, Freq, Route, Range: PO 5-15 mg PRN Max: 30 mg for special procedures PR 10 mg PRN Side Effects: Mild cramping, nausea, vomiting, diarrhea, fluid and electrolyte disturbances (especially potassium and calcium) Nursing Considerations: evaluate periodically patient’s need for continued use of drug, add high-fiber foods slowly to regular diet to avoid gas and diarrhea, adequate fluid intake includes at least 6-8 glasses/day, use of laxatives results in ↓ absorption of Vitamin K
1.71. Docusate Sodium (Colace) Class: Stool softener Actions: detergent action lowers surface tension, permitting water and fats to penetrate and soften stools for easier age Indications: prophylactically in patients who should avoid straining during defecation and for treatment for constipation Norm. Dosage, Freq, Route, Range: PO 50-500mg/day PR 50-100mg added to enema fluid Max: 500mg/day Side Effects: diarrhea, nausea, bitter taste, abdominal cramps Nursing Considerations: Withhold if diarrhea develops and notify prescriber. Take sufficient liquid with each dose. So not take for prolonged periods (causes slowed bowel mobility).
1.72. Lactulose (Cephulac; Chronulac) Class: Hyperosmotic Laxative; Neurologic Actions: Osmotic effect on lactulose moves water from plasma to intestines, softening stools, and stimulates peristalsis by pressure from water content of stool. Indications: Chronic Constipation, prevention and treatment of portal-systemic encephalopathy (PSE) including stages of hepatic precoma and come Norm. Dosage, Freq, Route, Range: PO 30-60mL/day PRN Max: 60mL/day Side Effects: diarrhea, nausea, vomiting, flatulence Nursing Considerations: promote fluid intake (1,500-2,000mL/day or greater) during drug therapy for constipation
Page 34 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.73. Metoclopramide (Metozolv, Reglan) Class: GI Stimulant; Prokinetic agent Actions: potent central dopamine receptor antagonist that increases resting tone of esophageal sphincter, and tone and amplitude of upper GI contractions. Thus gastric emptying and intestinal transit are accelerated. Antiemetic action results from druf-induced elevation of CTZ threshold and enhanced gastric emptying. Onset: 30-60 min. Peak: 1-2 hr.Duration: 1-3 hr. Indications: GERD, Diabetic gastroparesis, Small –bowel intubation/Radiologic Exam, ChemotherapyInduced Emesis, Postoperative Nausea/ Vomiting Norm. Dosage, Freq, Route, Range: PO 10-15 mg qid before meals and at bedtime IM/IV 10 mg qid Max: 60 mg Side Effects: mild sedation, fatigue, restlessness, diarrhea Nursing Considerations: report S&S immediately, lab tests: periodic serum electrolytes, monitor for possible hypernatremia and hypokalemia, avoid alcohol and other CNS depressants, avoid driving for a few hours after drug .
1.74. Polyethylene Glycol (Miralax) Class: Laxatives, Osmotics Actions: Acts as an osmotic agent, drawing water into the lumen of the GI Tract. Peak: 2-4days Indications: Indicated for evacuation of GI Tract w/o water or electrolyte imbalance. Norm. Dosage, Freq, Route, Range: 17g w/ 8oz of water Side Effects: abdominal bloating, cramping, flatulence, nausea Nursing Considerations: GI obstruction, gastric retention, toxic colitis, megacolon, use cautiously in patients w/ abdominal pain of uncertain cause, particularly if accompanied w/ fever.
1.75. Sennosides (Senokot) Class: Stimulant Laxative Actions: Peristalsis stimulated by conversion of drug to active chemical. Onset: 6-10hr; may take up to 24hr. Indications: Acute constipation and preoperative and preradiographic bowel evacuation Norm. Dosage, Freq, Route, Range: PO 1-2 tabs at bedtime Max 4 tabs Side Effects: nausea, abdominal cramps, flatulence, watery diarrhea Nursing Considerations: Reduce dose in patients who experience considerable abdominal cramping
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 35 of 75
Drug Med Cards
20. Anti-Diarrheal 1.76. Diphenoxylate (Diphenatol, Lofene, Lomanate) Class: Antidiarrheal Actions: reduces GI motility. Onset: 45-60 min Peak: 2hr. Duration: 3-4hr. Indications: management of diarrhea Norm. Dosage, Freq, Route, Range: PO 5-10mL 3-4 times daily Max: 40mL/day Side Effects: hypersensitivity, flushing, palpitation, headache, dizziness Nursing Considerations: Assess GI function, monitor for S&S of dehydration, frequency and consistency of stools
1.77. Loperamide (Maalox, Imodium, Kaopectate, Pepto) Class: Antidiarrheal Actions: Inhibits GI peristaltic activity by direct action on circular and longitudinal intestinal muscles. Prolongs transit time of intestinal contents, increases consistency of stools, and reduces fluid and electrolyte loss. Onset: 30-60min. Peak: 2.5hrs (solution), 4-5hrs. (Capsules) Duration: 4-5hrs. Indications: Acute Diarrhea; Chronic Diarrhea Norm. Dosage, Freq, Route, Range: PO 4mg followed by 2mg after each unformed stool Max: 16mg/day Side Effects: Toxic megacolon, abdominal pain or discomfort, constipation Nursing Considerations: monitor fluid and electrolyte balance, record number and consistency of stools
Page 36 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
21. Beta-Blockers 1.78. Atenolol (Tenormin) Class: Beta-Adrenergic Antagonist; Antihypertensive Actions: reduces rate & force of cardiac contractions (negative inotropic action); cardiac output is reduced as well as systolic and diastolic BP. Decreases peripheral vascular resistance both at rest and with exercise. Peak: 2-4hr. Duration: 24hr. Half-life: 6-7hr. Indications: management of hypertension as a single agent or concomitantly w/ other antihypertensive agents, especially a diuretic, and in treatment of stable angina pectoris, MI Norm. Dosage, Freq, Route, Range: PO 25-50mg/day, may increase to 100mg/day Max: 100mg/day Side Effects: Bradycardia, hypotension, CHF, pulmonary edema, nausea, vomiting Nursing Considerations: Measure trough BP, check apical pulse before ., monitor BP, monitor diabetics for loss of glycemic control
1.79. Carvedilol (Coreg, Coreg CR) Class: Alpha and Beta Adrenergic Antagonist; Antihypertensive Actions: An effective antihypertensive agent reducing BP to normotensive range and useful in managing some angina, dysrhythmias, and CHF by decreasing myocardial oxygen demand and lowering cardiac workload. Peak: Antihypertensive effect 7-14 days Indications: CHF, Left Ventricular Dysfunction, Post MI, Hypertension Norm. Dosage, Freq, Route, Range: PO start w/ 3.125mg bid Max: 50mg/day Side Effects: Dizziness Nursing Considerations: Monitor for therapeutic effectiveness, lab tests: LFTs and digoxin levels w/ concurrent use, monitor for worsening of symptoms in patients w/ PVD
1.80. Metoprolol Tartrate (Lopressor) Class: Cardioselective; Beta-adrenergic antagonist; Antihypertensive; Antianginal Actions: produces a decrease in the systolic and diastolic BPs, and reduces edema in CHF and kidney failure patients. Onset: 15min. Peak: PO 1.5hr. IV 20min. Duration: 13-19hr. Indications: management of hypertension Norm. Dosage, Freq, Route, Range: PO 50-100mg/day in 1-2 divided doses, may increase weekly up to 100-450mg/day Max: 450mg/day Side Effects: fatigue, insomnia, bradycardia, heartburn, shortness of breath Nursing Considerations: Take apical pulse and BP before istering drug. Monitor BP q12hr
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 37 of 75
Drug Med Cards
1.81. Propanolol (Inderal, InnoPran XL) Class: Beta-Adrenergic Receptor Antagonist; Antihypertensive; Class II Antiarrhythmic Actions: Nonselective beta-blocker of both cardiac and bronchial adrenoreceptors that competes w/ epinephrine and norepinephrine for available beta receptor sites. In higher doses, it depresses cardiac function including contractility and arrhythmias. Lowers both supine and standing BP in hypertensive patients. Peak: 60-90 min immediate release, 6 hr sustained release, IV 5 min Indications: Hypertension, Angina, Arrhythmias, Acute MI, Migraine Prophylaxis Norm. Dosage, Freq, Route, Range: PO 40 mg bid, usually need 160-480 mg/day Max: 480 mg/day Side Effects: confusion, fatigue, drowsiness, bradycardia, paresthesia of hands Nursing Considerations: Monitor apical pulse, respirations, BP and circulation to extremities. Be aware of adverse reactions, Lab tests: periodic hematologic, kidney, liver, and cardiac functions, monitor I&O
1.82. Sotalol (Betapace) Class: Beta-Adrenergic Antagonist; Class II and III Antiarrhythmic Actions: slows heart rate, decreases AV nodal conduction, and increases AV nodal refractoriness. Produces significant reduction in both systolic and diastolic blood pressure. Peak: 2-3 hr Duration: 24 hr Indications: Ventricular Arrhythmias, Atrial Fibrillation/Flutter Norm. Dosage, Freq, Route, Range: PO initial dose of 80 mg bid or 160 mg daily taken prior to meals, may increase every 3-4 days in 40-160 mg increments Max: 240 mg/day in 1-2 divided doses Side Effects: bradycardia, dyspnea, chest pain, palpation, fatigue, dizziness Nursing Considerations: Monitor ECG baseline and periodically, Lab tests: baseline serum electrolytes, monitor cardiac status throughout therapy, monitor patients w/ bronchospastic disease (ex: bronchitis, emphysema) for inhibition of bronchodilation, monitor diabetics for loss of glycemic control.
Page 38 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
22. Nitrates 1.83. Isosorbide Dinitrate (Dilatrate-SR, IsoBid) Class: Nitrate Vasodilator (prototype: Nitroglycerin) Actions: has an anti-anginal effect as a result of vasodilation of the coronary arteries. Onset: SL 2-5min. w/in 1hr. reg. tabs w/in 3 min. chewable tabs 30 min. sustained release tabs Duration: SL 1-2hr. Chewable tabs: 1.5-2hrs. Sustained release tabs: 6-8hrs. Indications: relief of acute anginal attacks and for management of long-term angina pectoris Norm. Dosage, Freq, Route, Range: 5-30mg q2-3hr. Max: 360mg/day Side Effects: light-headedness, flushing, headache, pallor Nursing Considerations: Monitor for effectiveness, headaches tend to decrease in intensity and frequency with continued use, may produce tolerance
1.84. Isosorbide Mononitrate (Ismo, Imdur) Class: Nitrate Vasodilator Actions: Long acting metabolite of the coronary vasodilator isosorbide dinitrate. It decreases preload as measured by pulmonary capillary wedge pressure and left ventricular end volume and diastolic pressure with a consequent reduction in myocardial oxygen consumption. Onset: 1 hr. Peak: regular release 30-60 min; sustained release 3-4 hr Duration: regular release 5-12 hr, sustained release 12 hr Indications: Prevention of Angina Norm. Dosage, Freq, Route, Range: PO regular release 20 mg bid 7 hr apart; sustained release 30-60 mg early morning, may increase up to 120 mg after several days if needed Max: 240 mg/day Side Effects: headache, anxiety, coughing, nasal congestion, dry mouth Nursing Considerations: Monitor cardiac status, frequency and severity of angina and BP, assess for S&S for toxicity, Lab tests: monitor serum electrolytes periodically.
1.85. Nitroglycerin (Nitro-Dur, Nitrostat, Nitroquick) Class: Nitrate Vasodilator Actions: Organic nitrate and potent vasodilator that relaxes vascular smooth muscle. After conversion to nitric oxide, it leads to dose-related dilation of both venous and arterial blood vessels. Promotes peripheral pooling of blood, reduction of peripheral resistance, and decreased venous return to the heart. Both left ventricular preload and afterload are reduced and myocardial oxygen consumption or demand is decreased. Onset: SL 2 min PO 3 min Ointment 30 min Duration: SL 30 min PO 3-5 hr Ointment 3-6 hr Indications: Angina Norm. Dosage, Freq, Route, Range: SL 1-2 sprays (0.4-0.8 mg) or 0.3-0.6 mg tablet q3-5min as needed Max: 3 doses in 15 min PO 1.3-9 mg q8-12 hr Ointment apply 1.5-5 cm of ointment q4-6hr Side Effects: dizziness, headache, postural hypotension, Syncope, tachycardia Nursing Considerations: Monitor BP, HR location, duration, pain
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 39 of 75
Drug Med Cards
23. ACE-Inhibitors 1.86. Lisinopril (Prinivil) Class: Antihypertensive, ACE inhibitor Actions: Lowers BP, improves cardiac output and exercise tolerance. Aldosterone is also reduced, thus permitting a potassium-sparing effect. Onset: 1 hr. Peak: 6-8hr. Duration: 24hrs. Indications: Hypertension, Heart Failure Norm. Dosage, Freq, Route, Range: (Hypertension) PO 10 mg once/day, may increase up to 20-40 mg 1-2x/day (Heart Failure) PO 5-40 mg/day Max: 80 mg/day Side Effects: Headache, dizziness, fatigue, hypotension, chest pain, nausea, vomiting, diarrhea, anorexia, constipation, intestinal angioedema, dyspnea, cough, rash, hyperkalemia, increase BUN and creatinine levels Nursing Considerations: Check BP before giving med. With pt. in supine position, monitor serum Na and K+ levels, Lab tests: WBC q month for the first 3-6 months of therapy and at periodic intervals for 1 yr.
1.87. Ramipril (Altace) Class: Angiotensin-Converting Enzyme (ACE) Inhibitor; Antihypertensive Actions: lowers BP, and improves cardiac output as well as exercise tolerance. Onset: 2hr Peak: 6-8hr Duration: up to 24hr Half-life: 2-3hr Indications: Norm. Dosage, Freq, Route, Range: PO 2.5-5mg daily, may increase up to 20 mg/day in 1-2 divided doses Max: 20mg/day Side Effects: Nursing Considerations: Monitor BP, Lab Tests: BUN and serum creatinine periodically. Observe for S&S of hyperkalemia
Page 40 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
24. Calcium Channel Blockers 1.88. Amlopidine (Norvasc) Class: Calcium Channel Blocker; Antihypertensive Actions: selectively block calcium influx across cell membranes of cardiac and vascular smooth muscle without changing serum calcium concentrations. Peak: 6-9 hr. Duration: 24 hr. Indications: Hypertension, Stable/Vasospastic Angina Norm. Dosage, Freq, Route, Range: PO 5-10 mg once daily Max: 10 mg Side Effects: peripheral and facial edema, headache Nursing Considerations: Monitor BP & HR, monitor for S&S of peripheral and facial edema, monitor BP with postural changes
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 41 of 75
Drug Med Cards
25. Central Acting Antihypertensive 1.89. Clonidine (Catapres) Class: Central-Acting Antihypertensive; Analgesic Actions: Decreases systolic and diastolic BP and HR. Reportedly minimizes or eliminates many of the common clinical S&S associated w/ withdrawal of heroin, methadone, or other opiates. Onset: PO 3060min. Peak: PO 2-4hr. Duration: PO 8hr. Indications: Hypertension, ADHD, Severe Pain Norm. Dosage, Freq, Route, Range: PO 0.1mg Max: 2.4mg/day Side Effects: Hypotension, dry mouth, drowsiness, sedation, constipation Nursing Considerations: Monitor BP closely, monitor I&O during period of dosage adjustment
1.90. Guanfacine HCL (Intuniv, Tenex) Class: Alpha-Adrenergic Agonist; Central-Acting Antihypertensive Actions: In cerebral cortex, stimulation of alpha2-adrenoreceptors triggers inhibitory neurons to reduce central sympathetic outflow (ie., impulses from vasomotor center to heart * blood vessels) Onset: 2hr.; 6hr. ER Peak: 6hr. Duration: Up to 24hr. Indications: Hypertension; Attention Deficit Hyperactivity Disorder (ADHD) Norm. Dosage, Freq, Route, Range: PO 1mg/day titrate up (Normal range: 1-4mg/day) Side Effects: dizziness, sedation, fatigue, dry mouth, constipation, impotence Nursing Considerations: do not d/c abruptly, may cause plasma & urinary catecholamine increases leading symptoms of tachycardia, insomnia, anxiety, nervousness; monitor BP until stabilized; assess mental status & alertness; employ measure to keep mouth moist; avoid alcohol & do not self-medicate w/ OTC drugs
Page 42 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
26. Antihypertensives 1.91. Losartan (Cozaar) Class: Angiotensin II Receptor Antagonist; Antihypertensive Actions: Antihypertensive effect is due to vasodilation and inhibition of aldosterone effects on sodium and water retention. Peak: 6hr. Duration 24hr. Indications: Hypertension Norm. Dosage, Freq, Route, Range: PO 25-52mg in 1-2 divided doses Max: 100mg/day Side Effects: dizziness, dyspepsia, insomnia, headache Nursing Considerations: Monitor BP at drug trough, lab tests: monitor CBC, electrolytes, liver and kidney functions w/ long-term therapy
1.92. Valsartan (Diovan) Class: Renin Angiotensin System Antagonist; Antihypertensive Actions: Blocks angiotensin II receptors results in vasodilation as well as decreasing the aldosteronesecreting effects of angiotensin II. These actions result in the antihypertensive effect of valsartan. Onset: BP decreased in 2 weeks. Peak: Plasma levels, 2-4hr; BP effect 4 weeks Indications: Hypertension, Heart Failure Norm. Dosage, Freq, Route, Range: PO 40-80mg daily Max: 320mg/day Side Effects: headache, dizziness, nausea, vomiting Nursing Considerations: monitor BP, lab tests: periodic LFTs, BUM, and creatinine, serum potassium, and CNC w/ differential
1.93. Terazosin (Prazosin) Class: Alpha-Adrenergic Receptor Antagonist, Antihypertensive Actions: Selectively blocks Alpha1-adrenergic receptors in vascular smooth muscle in many tissues, including vascular smooth muscle, the bladder neck, and the prostate. Promotes vasodilation, thus producing relaxation that leads to reduction of peripheral vascular resistance and lowers BP as well as increased urine flow. Peak: 1-2 hr. Indications: Hypertension, Benign Prostatic Hypertrophy Norm. Dosage, Freq, Route, Range: PO start with 1 mg at bedtime, then 1-5 mg/day Max: 20 mg/day Side Effects: Asthenia (weakness), dizziness, headache, 1st –dose phenomenon syncope Nursing Considerations: Monitor BP, be alert for possible 1st –dose phenomenon
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 43 of 75
Drug Med Cards
27. Antipsychotics 1.94. Aripiprazole (Abilify) Class: Atypical Antipsychotic; Dopamine System Stabilizer Actions: combination of partial agonist activity at D2 and 5-HT1A receptors and antagonists activity at 5HT2A receptors. Peak: 3-5hrs. Indications: Schizpphrenia; Bipolar Mania; Agitation associated w/ Schizophrenia/Bipolar; Adjunct in Major Depression; Irritability associated w/ Autism Norm. Dosage, Freq, Route, Range: PO 10-15mg once daily, may increase at 2wk intervals to Max: 30mg/day Side Effects: headache, insomnia, light-headedness, somnolence, akathisia, risk of stroke in elderly w/ dementia-related-psychosis, N&V, constipation Nursing Considerations: monitor cardiovascular status, Lab tests: periodic Hct and Hbg, and blood glucose, monitor for elevated K and myoglobinuria if NMS is suspected.
1.95. Asenapine (Saphris) Class: Atypical Antipsychotic; Serotonin Antagonist; Antimanic; Antidepressant Actions: thought to be related to antagonism to certain CND dopamine (D2) and serotonin (5-HT2a) receptors. Peak: 0.5-1.5hr. Indications: Schizophrenia; Bipolar Disorder Norm. Dosage, Freq, Route, Range: SL 5mg bid Side Effects: Extrapyramidal symptoms (EPS), headache, somnolence, insomnia Nursing Considerations: monitor BP, HR, and weight; monitor for orthostatic hypotension; monitor diabetes
1.96. Atomoxetine (Strattera) Class: Miscellaneous Psychotherapeutic Actions: Selective inhibition of the presynaptic norepinephrine transporter, resulting in norepinephrine reuptake inhibition. Peak: 1-2hr. Indications: Attention Deficit Hyperactivity Disorder (ADHD) Norm. Dosage, Freq, Route, Range: PO start w/ 40mg in a.m., may increase after 3 days to target dose of 80mg/day given either in a.m. or divided dose. May increase to 100mg/day if needed. Side Effects: headache, insomnia, suicidal ideation, upper abdominal pain, nausea, vomiting, decreased appetite, severe liver failure, and cough Nursing Considerations: evaluate therapeutic effectiveness; report increased aggression & irritability as there may indicate need to d/c the drug; monitor children & adolescence for behavior changes that may indicate suicidal ideation; monitor cardiovascular status especially w/ preexisting hypertension; monitor HR & BP at baseline, following a dose increase, and periodically during therapy; Lab tests: periodic LFTs
Page 44 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.97. Chlorpromazine (Thorazine) Class: Antipsychotic; Phenothiazine; Antiemetic Actions: mechanism thought to be related to blockade of post-synaptic dopamine receptors in the brain. Onset: 30-60min. Peak: PO 2-4hr. IM 15-20min. Duration: 4-6hr. Indications: Psychotic disorder, agitation; nausea and vomiting; dementia; intractable hiccups; tetanus Norm. Dosage, Freq, Route, Range: PO 25-100mg tid or qid, Max: 1,000mg/day IM/IV: 25-50mg Max: 600mg Side Effects: Agranulocytosis,Neuroleptic malignant syndrome (NMS), hypothermia,adynamic ileus, sedation, extrapyramidal symptoms (EPS) Nursing Considerations: Lab tests: LFTs, periodic CBC w/ diff, and blood glucose, monitor cardiac status, be alert for NMS and report immediately, report EPS, monitor BP frequently, may cause pink to red-brown discoloration of urine, have pt. wear protective clothing and sunscreen when outdoors, have pt. practice meticulous oral hygiene to prevent oral candidiasis
1.98. Clozapine (Clozaril) Class: Atypical Antipsychotic Actions: Interferes w/ binding of dopamine to D1 and D2 receptors in the limbic region of the brain. Onset: 2-4 wk. Peak: 2.5 hr. Indications: Schizophrenia Norm. Dosage, Freq, Route, Range: PO initiate 12.5mg daily or bid and increase by 25-50mg/day and titrate to a target of 350-400mg/day in 3 divided doses Max: 900mg/day Side Effects: tachycardia, agranulocytosis, transient fever, neuroleptic malignant syndrome (NMS), increased mortality from severe hematologic, cardiovascular, and respiratory adverse effects. Nursing Considerations: Lab tests: baseline WBC and absolute neutrophil count must be made before initial treatment q wk. for first 6 mon. then q2wk.for the next 6 mon. then q4wk.periodic blood glucose, monitor cardiovascular and respiratory status,
1.99. Fluphenazine HCL (Prolixin) Class: Antipsychotic; Phenothiazine Actions: thought to be related to blockade of post-synaptic dopamine receptors in the brain. Onset: 1hr. Peak: 0.5hr. Duration: 6-8hr. Indications: Psychosis; Dementia Behavior Norm. Dosage, Freq, Route, Range: PO 0.5-10mg/day in 1-4 divided doses Max: 20mg/day Side Effects: extrapyramidal symptoms (EPS), tardive dyskinesia, impaired thermoregulation, leukopenia, agranulocytosis, photosensitivity Nursing Considerations: report any EPS or mental depression, Lab tests: periodic WBC w/ diff, LFTs, monitor renal function and notify prescriber if BUN is elevated, have pt. wear protective clothing and sunscreen when outdoors, may discolor urine pink to red or reddish brown
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 45 of 75
Drug Med Cards
1.100. Haloperidol (Haldol) Class: Antipsychotic, Butyrophenone Actions: Blocks postsynaptic dopamine receptors in the limbic system of the brain. ↓ in dopamine neurotransmission has been correlated w/ its higher instance of extrapyramidal effects. ↓ Psychotic manifestations & exerts strong antiemetic effect. Onset: IM 30-45min. Peak: PO 2-6hr., IM 10-20min. Indications: Management of manifestations of psychotic disorders & for control of tics & vocal utterances of Tourette’s syndrome, for treatment of agitated state is acute and chronic psychoses. Norm. Dosage, Freq, Route, Range: PO 0.2-5 mg bid or tid Max: 15 mg.day IM 2-5 mg q4hr PRN Max: 30 mg/day Side Effects: extrapyramidal reactions, tardive dyskinesia, agitation, drowsiness, lethargy, fatigue, tremor, ataxia, headache, confusion, vertigo, tachycardia Nursing Considerations: monitor for drug effectiveness (long half-life), monitor patients’ mental status daily, be alert for behavioral changes
1.101. Iloperidone (Fanapt) Class: Atypical Antipsychotic Actions: is both a dopamine (D2) and serotonin (5-HT2) antagonist. Peak: 2-4hr. Indications: Schizophrenia Norm. Dosage, Freq, Route, Range: PO initial 1mg big, then titrated to 6-12mg bid Side Effects: dizziness, somnolence, tachycardia Nursing Considerations: monitor for suicidal ideation, monitor BP, HR, and weight, monitor for orthostatic hypotension, Lab tests: baseline and periodic CBC w/ diff
1.102. Lithium Carbonate (Eskalith, Lithane, Lithobid, Lithonate, Lithotabs) Class: Antipsychotic; Mood Stabilizer Actions: The lithium ions behaves in the body much like the sodium ion: but its exact mechanism of action is unclear. Peak: 0.5-3hrs. Indications: Mania Norm. Dosage, Freq, Route, Range: PO: Loading Dose 600mg tid or 900mg sustained release bid or 30mL of solution tid PO: Maintenance Dose 300mg tid or qid or 15-20mL solution in 2-4 divided dose Max: 2.4g/day Side Effects: headache, lethargy fatigue, recent memory loss, peripheral circulatory collapse, nephrogenic diabetes insipidus, nausea, vomiting, anorexia, abdominal pain, diarrhea, dry mouth, fine, hand tremors, muscle weakness, reversible leukocytosis Nursing Considerations: Lab tests: periodic lithium levels; periodic thyroid function tests; monitor for S&S of lithium toxicity; be alert to and report symptoms of hypothyroidism; drink plenty of liquids (2-3L/day)during stabilization and at least (1-1.5L/day) during ongoing therapy
Page 46 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.103. Lurasidone (Latuda) Class: Atypical Antipsychotic Actions: the mechanism of action is unknown but the efficacy of lurasidone in schizophrenia is thought to be mediated through central dopamine type 2 (D2) and serotonin Type 2 (5HT2a) receptor antagonism. Indications: Schizophrenia Norm. Dosage, Freq, Route, Range: PO 40-160mg one daily Side Effects: akathisia, dizziness, somnolence, parkinsonism, nausea Nursing Considerations: monitor orthostatic VS, Lab tests: periodic blood glucose, lipid profile, LFTs, and CBC w/ diff, monitor closely pts. w/ neutropenia, monitor weight, monitor for and report promptly seizure activity, S&S of Neuroleptic Malignant Syndrome (NMS) or tardive dyskinesia
1.104. Olanzapine (Zyprexa) Class: Atypical Antipsychotic Actions: thought to be due to antagonism for both serotonin 5-HT2A/2C and dopamine D1-4 receptors. Peak: 6hr. Indications: Psychotic disorders; Bipolar Mania; Acute Agitation Norm. Dosage, Freq, Route, Range: PO start w/ 5-10mg/day, may increase by 2.5-5mg q wk. until desired response Max: 20mg/day Side Effects: weight gain, somnolence, dizziness, agitation, insomnia, headache, nervousness, hostility, Parkinsonism Nursing Considerations: monitor cerebrovascular status closely, Lab tests: periodically monitor ALT, blood glucose, monitor BP and HR periodically and monitor temp.
1.105. Paliperidone (Invega) Class: Atypical Antipsychotic Actions: Interferes w/ binding of dopamine to dopamine type 2 (D2) receptors, serotonin (5-HT2a) receptors and alpha-adrenergic receptors. Peak: 24hrs Indications: Schizophrenia; Schizoaffective Disorder Norm. Dosage, Freq, Route, Range: PO initially 6mg/day, may adjust up/down in 3mg increments Max: 12mg/day Side Effects: Akathisia, headache, somnolence Nursing Considerations: Baseline ECG is recommended to rule out congenital long-QT syndrome; Lab tests: baseline and periodic serum electrolytes, periodic blood glucose, and CBC; monitor diabetes and loss of glycemic control
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 47 of 75
Drug Med Cards
1.106. Prochlorperazine Meleate (Compazine) Class: Antipsychotic; Phenothiazine, Antiemetic Actions: Strong antipsychotic effects thought to be due to blockade of postsynaptic dopamine receptors in the brain. Antiemetic effect is produced by suppression of the chemoreceptor trigger zone (CTZ). Onset: PO 30-40 min, PR 60 min, IM 10-20 min Duration: PO 3-4 hr, Sustained Release PO 10-12 hr, PR 3-4 hr, IM up to 12 hr Indications: Severe Nausea/Vomiting, Psychotic Disorders Norm. Dosage, Freq, Route, Range: PO 5-10 mg 3-4 times/day, Sustained Release PO 10-15 mg q 12 hr PR 25 mg bid IM 5-10 mg q3-4hr up to 40 mg/day IV 2.5-10 mg q3-4hr Max: 40 mg/day Side Effects: drowsiness, extrapyramidal reactions (akathisia, dystonia or parkinsonism) Nursing Considerations: position carefully to prevent aspiration, Lab tests: periodic CBC with diff in longterm therapy, be alert of high core temperature
1.107. Quetiapine (Seroquel) Class: Atypical Antipsychotic Actions: effectiveness indicated to a reduction in psychotic behavior. Peak: 1.5hr. Half-life: 6hrs. Indications: management of schizophrenia, maintenance of acute bipolar disorder, and add-on therapy for major depressive disorder Norm. Dosage, Freq, Route, Range: 25-50mg dose and increase by 25-50mg/day Max: 800mg/day Side Effects: dizziness, headache, somnolence, leukopenia Nursing Considerations: Monitor for respiratory depression in patients with chronic respiratory insufficiency and suicidal tendencies
1.108. Risperidone (Risperdol) Class: Atypical Antipsychotic Actions: interferes w/ binding of dopamine to D2-interlimbic region of the brain, serotonin (5-HT2) receptors, and alpha-adrenergic receptors in the occipital cortex. Onset: therapeutic effect 1-2 wk. Peak: 12hr. Indications: Schizophrenia; Bipolar Disorder; Irritability Associated w/ Autism Norm. Dosage, Freq, Route, Range: PO 1-2mg/day in 1 or 2 doses then titrate up Max: 8mg/day Side Effects: sedation, drowsiness, headache, insomnia, agitation, extrapyramidal symptoms (EPS), neuroleptic malignant syndrome (NMS) Nursing Considerations: monitor cardiovascular status closely, Lab tests: monitor periodically blood glucose, serum electrolytes, LFTs, and CBC, be aware of risk for orthostatic hypotension
Page 48 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.109. Thioridazine HCL (Mellaril) Class: Antipsychotic; Phenothiazine Actions: blocks post-synaptic dopamine receptors in the mesolimbic system of the brain. Onset: days to weeks Indications: Psychotic disorders; moderate to marked depression; dementia behavior Norm. Dosage, Freq, Route, Range: PO 50-100mg tid Max: 800mg/day Side Effects: sedation, paralytic ileus, urinary retention Nursing Considerations: monitor I&O ratio and bowel elimination pattern, orthostatic hypotension may occur, Lab tests: obtain periodic CBC and LFTs during therapy, avoid alcohol, may cause pink-red to reddish-brown urine
1.110. Trifluoperazine HCL (Stelazine) Class: Antipsychotic; Phenothiazine Actions: thought to be related to blockade of post-synaptic dopamine receptors in the brain. Onset: Rapid Peak: 2-3hr. Duration: up to 12hr. Indications: Schizophrenia; Anxiety Norm. Dosage, Freq, Route, Range: PO 1-2mg bid Max: 20mg/day Side Effects: drowsiness, extrapyramidal symptoms (EPS), neuroleptic malignant syndrome (NMS), dry mouth, hypotension Nursing Considerations: monitor HR and BP, monitor I&O ratio and bowel elimination pattern, Lab tests: periodic CBC and serum prolactin, cover as much skin surface as possible with clothing when you must be in direct sunlight, urine may be discolored or reddish-brown
1.111. Ziprasidone HCL (Geodon) Class: Atypical Antipsychotic Actions: exerts antischizophrenic effects through dopamine (D2) and serotonin (5-HT2a) receptors antagonism. Peak: 6-8hrs. Indications: Schizophrenia; Acute episodes of Agitation/Acute psychosis, Acute Mania/Bipolar Disorder Norm. Dosage, Freq, Route, Range: PO start w/ 20mg bid w/ food, may increase q2days up to 80mg bid if needed Max: 160mg/day Side Effects: somnolence, nausea Nursing Considerations: Lab tests: baseline and periodic ECGs, serum potassium and serum magnesium, periodically monitor blood glucose, monitor I&O ratio and pattern, monitor BP, monitor cognitive status, monitor for loss of seizure control, avoid strenuous exercise, exposure to extreme heat, or other activities that may cause dehydration
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 49 of 75
Drug Med Cards
28. Anti-Coagulants 1.112. Enoxaparin (Lovenox) Class: Anticoagulant; Low Molecular Weight Heparin Actions: An effective anticoagulation agent, if is used for prophylactic treatment as an antithrombotic agent following certain types of surgery. Peak: 3 hr. Duration 4-6 hr. Indications: Prevention of DVT after Hip or Knee Surgery, Prevention of DVT after Abdominal Surgery, Treatment of DVT and Pulmonary Embolus, Non-Q Wave MI Acute STEMI Norm. Dosage, Freq, Route, Range: SQ 30 mg bid for 10-14 days starting 12-24 hr post-surgery Max: 60 mg/day Side Effects: Dyskinesia, Hyperkinesia, Nausea, Diarrhea, Urine discoloration Nursing Considerations: Monitor carefully for hyperpyrexia, confusion, or emergence of Parkinson’s S&S during drug w/drawal, monitor for orthostatic hypotension and worsening of dyskinesia, or hyperkinesia, Lab tests: Hgb and serum ferritin levels w/ prolonged therapy
1.113. Heparin (Heparin Sodium) Class: Anticoagulant Actions: Has rapid anticoagulant effect, does not lyse already existing thrombi but may prevent their extension & propagation. Onset: SQ 20-60min. Peak: in min. Duration: SQ 8-12hr. IV 2-6hr. Indications: prophylaxis and treatment of venous thrombosis and pulmonary embolism & to prevent thromboembolic complications arising from cardiac & vascular surgery, frostbite, & curing acute stage of MI Norm. Dosage, Freq, Route, Range: IV 5,000 units bolus dose then 20,000-40,000 units infused over 24hr, dose adjusted to maintain desired aPTT or 5,000-10,000 units IV piggyback q4-6 hr Max: 60,000 units/day SQ 10,000-20,000 units/m2/24hr Side Effects: spontaneous bleeding, fever, chills, numbness, elevated BP, headache Nursing Considerations: Lab tests: baseline blood coag., Hct, Hgb, RBC, & platelet count prior to ., monitor aPTT levels closely, blood draw for coag. test 30 min before each scheduled SQ or intermittent IV dose, observe all needle sites daily, monitor vital signs
Page 50 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
29. Antiplatelets 1.114. Aspirin (ASA) Class: Non-narcotic, Antiplatelet, Antipyretic Actions: inhibiting the formation of prostaglandins involved in the production of inflammation, pain and fever, powerfully inhibits platelet aggregation. High serum salicylate concentrations can impair hepatic synthesis of blood coagulation factors VII, IX, X. Peak: 15min-2hr. Indications: Anti-inflammatory action, pain, fever reducer, antiplatelet Norm. Dosage, Freq, Route, Range: PO: 350-650 mg q4h Max: 4 g/day Side Effects: Bronchospasm, anaphylactic shock (laryngeal edema), nausea, heartburn, stomach pains, thrombocytopenia, hemolytic anemia Nursing Considerations: Allergy to any ASA, monitor for salicylate toxicity. In adults, a sensation of fullness in the ears, tinnitus, and decreased or muffled hearing are the most frequent symptoms.
1.115. Clopidogrel (Plavix) Class: Antiplatelet Actions: prolongs bleeding time, thereby reducing atherosclerotic events in high-risk patients. Onset: 2hr. reaches steady state in 3-7 days Half-life: 8hr. Indications: acute coronary syndrome (ST or non-ST elevations). Secondary of MI, stroke, and vascular death Norm. Dosage, Freq, Route, Range: PO 75mg/day Max: 75mg/day Side Effects: fatigue, back pain, diarrhea, nausea, headache, dizziness Nursing Considerations: Monitor for S&S of GI bleeding. Lab tests: platelet count, and lipid profile
1.116. Dipyridamole (Apo-Dipyridamole) Class: Antiplatelet; Platelet Aggregate Inhibitor Actions: Nonnitrate coronary vasodilator that increase coronary blood flow by selectively dilating coronary arteries, thereby increasing myocardial oxygen supply. Peak: 45-150 min. Indications: Prevention of thromboembolism in cardiac valve replacement, Thromboembolic Disorders, Thallium Stress Test Norm. Dosage, Freq, Route, Range: PO 150-400 mg/day in divided doses Max: 400 mg/day Side Effects: headache, dizziness, faintness, syncope, weakness Nursing Considerations: monitor therapeutic effectiveness
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 51 of 75
Drug Med Cards
30. Proton Pump Inhibitor 1.117. Omeprazole (Prilosec, Prilosec OTC) Class: Proton Pump Inhibitor (PPI); Antisecretory Actions: Suppresses gastric acid secretion relieving gastrointestinal distress and promoting ulcer healing. Onset: 0.5-3.5hr. Peak: 5 days Indications: GERD, Duodenal Ulcer, Erosive Esophagitis, Hyper secretory disease, gastric ulcer Norm. Dosage, Freq, Route, Range: PO 20-40mg once/day for 4-8 weeks Max: 360mg/day Side Effects: headache, dizziness, fatigue, diarrhea, abdominal pain, nausea Nursing Considerations: Lab tests: monitor urinalysis for hematuria and proteinuria, periodic LFTs w/ prolonged use.
1.118. Pantoprazole (Protonix) Class: Gastric Proton Pump Inhibitor; Antisecretory Actions: suppresses gastic acid secretion by inhibiting the acid (proton H+) pump in the parietal cells. Peak: 2-4hrs. Indications: short-term treatment of erosive esophagitis associated w/ gastroesphageal reflux disease (GERD), hyper secretory Norm. Dosage, Freq, Route, Range: PO 40mg daily for 7-10days Max: 40mg/day Side Effects: diarrhea, flatulence, abdominal pain, headache, insomnia, rash Nursing Considerations: Lab tests: Urea breath test 4-6 wks after completion of therapy. Monitor for severe skin reaction
Page 52 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
31. H2- Receptor Antagonist 1.119. Famotidine (Pepcid) Class: Antisecretory (H2-Receptor Antagonist) Actions: reduces parietal cell output if hydrochloric acid; thus, detrimental effects of acid on gastric mucosa are diminished. Onset: 1hr Peak: 1-3hr Duration: 10-12hr Indications: short-term treatment of active duodenal ulcer, GERD, gastritis Norm. Dosage, Freq, Route, Range: PO 40mg at bedtime or 20mg bid IV 20 mg q12hr. Max: 40mg/day Side Effects: dizziness, headache, confusion, depression, constipation, diarrhea Nursing Considerations: Monitor for improvement in GI distress. Monitor for signs of GI bleeding. Be aware that pain relief may not be experience for several days.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 53 of 75
Drug Med Cards
32. Cerebral Stimulant 1.120. Amphetamine Sulfate (Adderall) Class: Cerebral Stimulant; Anorexiant Actions: Marked stimulant effect on CNS thought to be due to action on cerebral cortex & possibly the reticular activating system. Acts indirectly on adrenergic receptors by increasing synaptic release of norepinephrine in the brain & by blocking reuptake of norepinephrine at the presynaptic membrane. Peak: 1-5hr. Duration: Up to 10hr. Indications: Narcolepsy; Attention Deficit Disorder (ADD) Norm. Dosage, Freq, Route, Range: PO 10mg ER once daily in a.m.; may increase by 5-10mg at weekly intervals if need to max of 30mg/day Side Effects: Sudden death; irritability; restlessness; insomnia; euphoria; palpitation Nursing Considerations: Monitor S&S of toxicity in children; monitor for S&S of insomnia or anorexia; monitor BP & HR; monitor diabetic closely; monitor growth in children; meticulous oral hygiene is required because of decreased saliva; rinse mouth frequently with clear water; avoid caffeine-containing beverages because caffeine increase amphetamine effects; taper drug on withdrawal
1.121. Methylphenidate HCL (Ritalin, Focalin, Concerta) Class: Cerebral Stimulant Actions: Acts mainly on cerebral cortex exerting stimulant effect. Peak: 1.9hr. 4-7hr. sustained release, 2hr. transdermal Duration: 3-6hr., 8 hr. sustained release Indications: Narcolepsy; Attention Deficit Disorder (ADD) Norm. Dosage, Freq, Route, Range: PO immediate release products 20-30mg/day in divided doses Concerta extended release 18-36mg/day Side Effects: nervousness, insomnia, exfoliative dermatitis Nursing Considerations: Monitor BP & pulse at appropriate intervals; Lab tests: obtain periodic CBC w/ diff & platelet counts during prolonged therapy; monitor closely pt. w/ history of alcoholism; supervise drug withdrawal; check weight at least 2-3 times weekly & report weight loss; check height & weight in children, failure to gain in either should be reported to prescriber; w/hold patch from an ADHD child who exhibits anxiety, tension, or agitation & consult prescriber
Page 54 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
33. Antihistamines 1.122. Diphenhydramine (Benadryl) Class: Centrally acting cholinergic antagonist, Antihistamine, h1-receptor antagonist Actions: suppresses central cholinergic activity and prolongs action of dopamine by inhibiting its reuptake and storage. Onset: 15-30 min. Peak: 1-4hr. Duration: 4-7hr. Indications: temporary symptomatic relief of various allergic conditions and to treat or prevent motion sickness, vertigo, and reactions to blood or plasma in susceptible patients Norm. Dosage, Freq, Route, Range: PO 25-50mg tid or qid Max: 300mg/day IV/IM 10-50mg q4-6hr Max: 400mg/day Side Effects: drowsiness, tachycardia, dry mouth Nursing Considerations: supervise ambulation, monitor cardiovascular status, do not use with alcohol and other CNS depressants, increase fluid intake
1.123. Hydroxyzine HCL (Atarax) Class: Antihistamine, H1-receptor antagonist Actions: H1 receptor antagonist blocks histamine. Onset: PO 15-30min. Duration: 4-6hrs. Indications: Anxiety; Pruritus; Nausea Norm. Dosage, Freq, Route, Range: PO 50-100mg tid IM 50-100mg q4-6hrs. Side Effects: drowsiness, dizziness, headache, hypotension, urticarial, dyspnea, chest tightness, wheezing, involuntary motor activity Nursing Considerations: reduce if CNS depressants are prescribed concomitantly, monitor oral membranes, alertness and drowsiness
1.124. Hydroxyzine Pamoate (Vistaril) Class: Antihistamine, H1-receptor antagonist Actions: H1 receptor antagonist blocks histamine. Onset: PO 15-30min. Duration: 4-6hrs. Indications: Anxiety; Pruritus; Nausea Norm. Dosage, Freq, Route, Range: PO 50-100mg tid IM 50-100mg q4-6hrs. Side Effects: drowsiness, dizziness, headache, hypotension, urticarial, dyspnea, chest tightness, wheezing, involuntary motor activity Nursing Considerations: reduce if CNS depressants are prescribed concomitantly, monitor oral membranes, alertness and drowsiness
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 55 of 75
Drug Med Cards
1.125. Promethazine (Phenergan) Class: Antihistamine, Antiemetic, Antivertigo Actions: Long-acting derivative of phenothiazine with marked antihistamine activity and prominent sedative, amnesic, and anti-motion sickness actions. Onset: PO/PR/IM 20 min IV 5 min Duration: 2-8 hr Indications: Motion sickness, nausea, pruritus sedation Norm. Dosage, Freq, Route, Range: PO/PR 25mg q12hr Max: 50mg Side Effects: drowsiness, blurred vision, dry mouth Nursing Considerations: supervise ambulation, monitor respiratory function, drug may suppress cough reflex and cause thickening of bronchial secretions
Page 56 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
34. Antidiabetic 1.126. Glipizide (Glucotrol) Class: Antidiabetic, Sulfonylurea Actions: It lowers blood glucose level by stimulating pancreatic beta cells. Glipizide improves postprandial glycemic control. Onset: 15-30 min. Peak: 1-2 hr. Duration up to 24 hr. Indications: Adjunct to diet for control of hyperglycemia in patient with type 2 diabetes mellitus. Norm. Dosage, Freq, Route, Range: PO: 2.5-5 mg/day 30 min. before breakfast, may increase by 2.5-5 mg q1-2 wk; greater than 15mg/day in divided doses before morning and evening meals Max: 40 mg/day Side Effects: hypoglycemia, anorexia, nausea, epigastric discomfort, heartburn, diarrhea, allergic skin reactions Nursing Considerations: Observe for early signs of hypoglycemia, lab tests: monitor fasting and postprandial blood glucose, and periodic HgbA1C, LFTs, electrolytes and serum osmolarity, must be made aware of the potential for hypoglycemia responses.
1.127. Glyburide (DiaBeta, Glynase) Class: Antidiabetic; Sulfonylurea Actions: One of the most potent of the 2nd generation sulfonylurea hypoglycemic agents. Appears to lower blood sugar concentration in both diabetic and nondiabetic individuals by sensitizing pancreatic beta cells to release insulin in the presence of elevated serum glucose levels. Onset: 15-60min. Peak: 1-2hr. Duration: up to 24hr. Half-life: 10hr. Indications: adjunct to diet and exercise to lower blood glucose in patients with type 2 diabetes mellitus. Norm. Dosage, Freq, Route, Range: PO 1.25mg-5mg/day, may increase by 2.5-5mg q1-2wk; greater than 15mg/day should be given in divided doses with morning and evening meal Max: 20mg/day Side Effects: hypoglycemia, nausea, vomiting, blurred vision Nursing Considerations: Monitor blood glucose levels carefully, monitor at regular intervals: Fasting and postprandial blood glucose, HbA1C, and LFTs.
1.128. Insulin (Regular) (Humulin R, Novolin R) Class: Antidiabetic, short-acting insulin Actions: Lowers blood glucose levels by increasing peripheral glucose uptake and by inhibiting the liver from changing glycogen to glucose. Onset: 0.5-1hr. Peak: 2-4hr. Duration: 5-7hrs. Indications: Emergency treatment of diabetic ketoacidosis or coma, to initiate therapy in patient w/ insulindependent diabetes, an in combo w/ inter.-acting or long-acting insulin to provide better control of blood glucose concentration. Norm. Dosage, Freq, Route, Range: SQ 5-10 units 30-60 min a.c and at bedtime (dose adjustments based on blood glucose determinations) Side Effects: hypoglycemia, nausea, palpitation, profuse sweating, hunger, tremulousness, weakness, fatigue, numb mouth and tongue Nursing Considerations: lab tests: periodically monitor fasting and postprandial blood glucose and HbA1C, test urine for ketones in new, unstable & Type 1 diabetes, if patient lost weight, exercises
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 57 of 75
Drug Med Cards vigorously, or has an illness, whenever blood glucose is substantially elevated (Onset: 0.5-1 hr. Peak: 2-4 hr. Duration: 5-8 hr.)
1.129. Insulin (NPH) (Humulin N, Novolin N) Class: Antidiabetic, Intermediate-acting insulin Actions: Controls post-pyramidal hyperglycemia, usually w/o supplemental doses of insulin injection. Onset: 1-2hr. Peak: 4-12hrs. Duration: 18-24hrs. Indications: Used to control hyperglycemia in the diabetic patient. Norm. Dosage, Freq, Route, Range: SQ 5-10 units 30-60 min a.c and at bedtime (dose adjustments based on blood glucose determinations) Side Effects: hypoglycemia, nausea, palpitation, profuse sweating, hunger, tremulousness, weakness, fatigue, numb mouth and tongue Nursing Considerations: lab tests: periodically monitor fasting and postprandial blood glucose and HbA1C, test urine for ketones in new, unstable and Type 1 diabetes, if patient lost weight, exercises vigorously, or has an illness, whenever blood glucose is substantially elevated (Onset: 1-2 hr. Peak: 4-12 hr. Duration: 10-18hr.)
1.130. Insulin Detemir (Levemir) Class: Antidiabetic; Long-acting insulin Actions: effective as a glucose-lowering agent, w/ glycemic control equivalent to that of NPH insulin. Peak: 6-8hrs. Indications: treatment of diabetes mellitus Norm. Dosage, Freq, Route, Range: SQ 0.1-0.2units/kg daily in evening or 10units daily or bid in evenly spaced doses Side Effects: hypoglycemia, weight gain, allergic reactions, rash Nursing Considerations: Monitor for S&S of hypoglycemia. Periodic fasting blood glucose and HbA1C, serum potassium with concurrent potassium-lowering drugs
1.131. Insulin Glargine (Lantus) Class: Antidiabetic long-acting insulin Actions: Lowers blood glucose levels over an extended period of time. It also prevents the conversion of glucagon to glucose in the liver. Onset: 3-4hrs. Duration: 10.4-24hrs. Indications: Bedtime dosing of adults and children w/ type 1 diabetes, or adults w/ type 2 diabetes Norm. Dosage, Freq, Route, Range: SQ for Type 1: if not taking insulin, give 10 units at same time each day (usually at bedtime) once daily, adjust based on patient need and concurrent medication SQ Type 2: if already taking oral hypoglycemic drugs, start w/ 10 units at same time each day (usually at bedtime) once daily and adjust according to patient’s need Side Effects: hypoglycemia, hypokalemia, injection site reaction Nursing Considerations: monitor for S&S of hypoglycemia, lab tests: periodically monitor fasting and postprandial blood glucose and HbA1C (Onset: 2-8 hr. Peak: none Duration: 5-24 hr.)
Page 58 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
1.132. Insulin Lispro (Humalog) Class: Antidiabetic; Rapid-Acting Insulin Actions: It lowers blood glucose levels and inhibits liver from changing glycogen to glucose. Onset: less than 15 minutes Peak: 0.5-1hr Duration: 3-4hr. Indications: Diabetes Mellitus Norm. Dosage, Freq, Route, Range: SQ 5-10 units 0-15min before meals (dose adjustments based on blood glucose determinations) Side Effects: hypoglycemia, hypokalemia, injection site reaction Nursing Considerations: monitor for S&S of hypoglycemia, lab tests: periodically monitor fasting and postprandial blood glucose and HbA1C
1.133. Metformin (Glucophage) Class: Antidiabetic; Biguanide Actions: Effective in lowering serum glucose level and ultimately, the HbA1C valve. Peak: 1-3hr. Half-life: 6.2-17.6hr. Indications: treatment of type 2 diabetes mellitus as adjunct to diet and exercise Norm. Dosage, Freq, Route, Range: PO start w/ 500mg daily tid or 850mg daily bid w/ meals, may increase by 500-850mg/day q1-3wk Max: 2550mg/day Side Effects: nausea, vomiting, abdominal pain, diarrhea, bitter or metallic taste, bloatedness, anorexia Nursing Considerations: Monitor vital signs and fasting and postprandial blood glucose valves, monitor cardiopulmonary status, Lab tests: baseline and periodic LFTs, kidney function tests, hematologic parameters for anemia, periodic fasting blood glucose, and HbA1C q3months.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 59 of 75
Drug Med Cards
35. Antihypoglycemic 1.134. Glucagon (Glucagen) Class: Antihypoglycemic Actions: increases blood glucose secondary to gluconeogenesis, which is the breakdown of glycogen in the liver. Onset: 5-20 min. Peak: 30 min. Duration: 1-1.5hr. Half-life: 3-10 min. Indications: hypoglycemia, radiologic studies of GI Tract Norm. Dosage, Freq, Route, Range: IM/IV/SQ 1mg may repeat q5-20min if no response for 1-2more doses Side Effects: nausea, vomiting, Stevens-Johnson syndrome Nursing Considerations: be prepared to give IV glucose if patient fails to respond to glucagon
Page 60 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
36. Anti-fungal 1.135. Metronidazole (Flagyl) Class: Antitrichomonal; Amebicide Actions: Has direct trichomonacidal and amebicial activity; exhibits antibacterial activity against obligate anaerobic bacilli, and Clostridia. Peak: 1-3 hr. Indications: Trichomoniasis, Giardiasis, Amebiasis, Pseudomembranous Colitis, Rosacea Norm. Dosage, Freq, Route, Range: PO 7.5 mg/kg q6hr. IV Loading Dose 1.5 mg/kg IV Maintenance Dose 7.5 mg/kg q6hr. Max: 4 g/day Side Effects: Candida, Nausea Nursing Considerations: Discontinue therapy immediately if symptoms of CNS toxicity develop, Monitor for seizures and peripheral neuropathy, Lab tests: obtain total and differential WBC count before, during, and after therapy, monitor S&S of sodium retention, monitor patients on lithium, report appearance of candidiasis, repeat feces exam, usually up to 3 months to ensure that amebae have been eliminated.
1.136. Ticonozole (Monistat Cream) Class: Anti-fungal Actions: spectrum antifungal that inhibits the growth of yeast (Candida Albacans) Indications: Vulvovaginal candidiasis Norm. Dosage, Freq, Route, Range: 6.5% vaginal ointment, intra vaginal x1day (one full applicator at bed time) Side Effects: mild erythema, burning, discomfort, rash, and itching Nursing Considerations: monitor for sensitization, and allergic response.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 61 of 75
Drug Med Cards
37. Eye Drops 1.137. Brimonidine Tartrate (Alphagan P) Class: Carbonic Anhydrase Inhibitor; Sulfonamide Actions: to reduce IOP and to protect the lens during surgery and laser iridotomy; to counteract effects of mydriatics and cycloplegics following surgery or, ophthalmoscopic exam Indications: Intraoperative and postsurgical increase in IOP, Open-Angle Glaucoma, Glaucoma Norm. Dosage, Freq, Route, Range: 1-2 drops per eye/day Side Effects: diminished vision in poorly illuminated areas, headache, drowsiness Nursing Considerations: Do not use in patients with Sulfa allergies
1.138. Timolol Maleate (Timoptic GTTS) Class: Beta-Adrenergic Antagonist, eye prep, miotic, antihypertensive, antuanginal Actions: GTTS: lowers elevated and normal IOP by reducing formation of aqueous humor/may increase out flow. Peak: PO 1-2hr. Topical: 1-5hrs. Indications: Chronic, open angle glaucoma, sec. glaucoma, or ocular hypertension Norm. Dosage, Freq, Route, Range: 0.25%, 0.5% one drop bid Side Effects: eye irritant, conjunctivitis, blepharitis, keratitis, superficial punctuate Nursing Considerations: √ pulse before istering oral or topical, √ BP for any extreme rates or rhythm
Page 62 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
38. Antidepressant 1.139. Bupropion HCL (Wellbutrin, Zyban, Aplenzin, Budeprion) Class: Antidepressant Actions: The neurochemical mechanisms of bupropion is not fully understood. It selectively inhibits the neuronal reuptake of dopamine. Onset: 3-4wks. Peak: 1-3hrs. Indications: Depression/Seasonal Affective Disorder Norm. Dosage, Freq, Route, Range: PO 100mg tid (immediate release) or 150mg bid (SR), or 300mg daily (XL), doses greater than 450mg/day are associated w/ an increased risk of adverse reactions including seizures Max: 300mg/day Side Effects: agitation, insomnia, dry mouth, blurred vision, headache, dizziness, tremor, nausea, vomiting, constipation. Nursing Considerations: Lab tests: periodic renal function tests and LFTs; monitor for and report delusions, hallucinations, psychotic, episodes, confusion, and paranoia; report significant restlessness, agitation, anxiety, and insomnia; monitor weight weekly; report promptly suicidal thoughts; do not take any OTC drugs w/o consulting physician.
1.140. Desvenlafaxine (Pristiq) Class: Antidepressant; Serotonin Norepinephrine Reuptake Inhibitor (SNRI) Actions: Potent inhibitor of neuronal serotonin and norepinephrine reuptake. Onset: 2wks. Peak: 1-2hrs. Duration: extensively tissue bound Indications: Depression; Anxiety Norm. Dosage, Freq, Route, Range: PO 25-125mg tid Max: 375mg/day Side Effects: increased BP & HR, dizziness, somnolence, suicidality, nausea, vomiting, dry mouth, sweating Nursing Considerations: Monitor for worsening of depression or emergence of suicidal ideation; monitor cardiovascular status periodically w/ measurements of BP & HR; Lab tests: periodic lipid profile; monitor neurologic status and report excessive anxiety, nervousness, and insomnia; monitor weight periodically and report excess weight loss; avoid using alcohol
1.141. Duloxetine (Cymbalta) Class: Antidepressant; Selective Serotonin Norepinephrine Reuptake Inhibitor (SSNRI) Actions: Causes potentiation of serotonergic and noradrenergic activity in the CNS. Antidepressant and antianxiety effects are presumed to be due to its dual inhibition of CNS presynaptic neuronal uptake of serotonin and norepinephrine, this increasing the serum levels of bith substances. Peak: 6hrs. Indications: Depression; Generalized Anxiety/Diabetic Neuropathy/Musculoskeletal Pain; Fibromyalgia Norm. Dosage, Freq, Route, Range: PO 40-60mg/day in 1-2 divided doses Side Effects: insomnia, dry mouth, constipation Nursing Considerations: Monitor for S&S of numerous drug-drug interactions; Lab tests: LFTs for unexplained abdominal pain or enlarged liver; monitor closely for and report suicidal ideation; report emergence of any of the following: anxiety, insomnia, agitation, panic attacks, irritability, hostility, psychomotor restlessness, hypomania, and mania
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 63 of 75
Drug Med Cards
1.142. Mirtazapine (Remeron) Class: Tetracyclic Antidepressant; Anxiolytic Actions: Acts as antidepressant. Effectiveness is indicated by mood elevation. Peak: 2 hr. Indications: Depression Norm. Dosage, Freq, Route, Range: PO 15mg/day in a single dose at bedtime, may increase Q1-2week Max: 45mg/day Side Effects: Somnolence, increased appetite, constipation, dry mouth Nursing Considerations: Lab tests: monitor WBC count w/ differential, lipid profile, and ALT/AST periodically, monitor for worsening of depression or suicidal ideation, asses for weight gain and excessive somnolence or dizziness, monitor for orthostatic hypotension w/ a Hx of cardiovascular disease or cerebrovascular disease.
1.143. Trazadone (Desyrel, Oleptro) Class: Antidepressant Actions: Centrally acting antidepressant that potentiates serotonin effects by selectively blocking its reuptake at presynaptic membranes in CNS. Onset: 1-2wks. Peak: 1-2hrs. Indications: Depression Norm. Dosage, Freq, Route, Range: PO 150mg/day in divided doses, may increase by 50mg/day q34days Max: 400-600mg/day (Immediate release) PO 150mg/day may increase by 75mg/day at 3 day intervals Max: 375mg/day (Extended release) Side Effects: drowsiness, hypotension (including orthostatic hypotension), dry mouth Nursing Considerations: Monitor BP & HR & rhythm; monitor for orthostatic hypotension; be aware that overdose is characterized by an extension of common adverse effects: vomiting, lethargy, drowsiness, and exaggerated anticholinergic effects.
1.144. Venlafaxine (Effexor) Class: Antidepressant; Serotonin Norepinephrine Reuptake Inhibitor (SNRI) Actions: Potent inhibitor of neuronal serotonin and norepinephrine reuptake. Onset: 2wks. Peak: 1-2hrs. Duration: extensively tissue bound Indications: Depression; Anxiety Norm. Dosage, Freq, Route, Range: PO 25-125mg tid Max: 375mg/day Side Effects: increased BP & HR, dizziness, somnolence, suicidality, nausea, vomiting, dry mouth, sweating Nursing Considerations: Monitor for worsening of depression or emergence of suicidal ideation; monitor cardiovascular status periodically w/ measurements of BP & HR; Lab tests: periodic lipid profile; monitor neurologic status and report excessive anxiety, nervousness, and insomnia; monitor weight periodically and report excess weight loss; avoid using alcohol
Page 64 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
39. Tricyclic Antidepressants 1.145. Amitriptyline HCL (Elavil) Class: Tricyclic Antidepressant Actions: a tricyclic antidepressant that inhibits the reuptake of serotonin (5-HT) and norepinephrine from the synaptic gap; also inhibits norepinephrine reuptake to a moderate degree. Peak: 2-12hrs. Indications: Antidepressant Norm. Dosage, Freq, Route, Range: Side Effects: drowsiness, sedation, dizziness, orthostatic hypotension, dry mouth, constipation, urinary retention, bone marrow suppression Nursing Considerations: Lab tests: baseline and periodic leukocyte and differential counts, renal and hepatic function tests, monitor BP and pulse rate, monitor I&O and bowel elimination pattern
1.146. Doxepin HCL (Sinequan, Prudoxin, Silenor, Zonalon) Class: Tricyclic Antidepressants; Anxiolytic Actions: inhibits serotonin reuptake from the synaptic gap; also inhibits norepinephrine reuptake to a moderate degree. Peak: 2hrs. Indications: Depression/Anxiety; Insomnia (Silenor), Dermatitis Norm. Dosage, Freq, Route, Range: PO 25-150mg/day in divided doses, may increase up to 300mg/day Max: 300mg/day Side Effects: drowsiness, orthostatic hypotension, dry mouth, blurring or stinging at application site Nursing Considerations: monitor use of other CNS depressants, including alcohol; be alert to changes in voiding and evaluate pt. for constipation and abdominal distention; maintain established dosage regimen and avoid change of intervals, doubling, reducing, or skipping doses.
1.147. Imipramine HCL (Tofranil) Class: Tricyclic Antidepressant (TCA) Actions: TCAs potentiate both norepinephrine and serotonin in the CNS by blocking their reuptake. Peak: 1-2hr. Indications: Depression; enuresis Norm. Dosage, Freq, Route, Range: PO 75-100mg/day Max: 300mg/day in 1 or more divided doses. Side Effects: sedation, drowsiness, angioedema, orthostatic hypotension, arrhythmias, MI, heart block, blurred vision, slight mydriasis, dry mouth, urinary retention, agranulocytosis, thrombocytopenia Nursing Considerations: Lab tests: monitor periodic LFTs, renal function, CBC w/ diff, and fluid and electrolyte balance, monitor HR and BP frequently, report EPS, Avoid exposure to sunlight and use sunscreen
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 65 of 75
Drug Med Cards
1.148. Nortriptyline HCL (Aventyl, Pamelor) Class: Tricyclic Antidepressant Actions: Secondary amine derivative of amitriptyline that inhibits that action of many chemical agents including catecholamines. Mood elevation may be due to its inhibition of reuptake of serotonin or another neurotransmitter at the presynaptic membrane. Peak: 7-8.5hrs. Duration: Crosses placenta; distributed in breast milk Indications: Antidepressant; Nocturnal Enuresis Norm. Dosage, Freq, Route, Range: PO 25mg tid or qid, gradually increase to 100-150mg/day Side Effects: orthostatic hypotension, dry mouth, agranulocytosis, urinary retention Nursing Considerations: monitor BP & pulse rate during adjustment period, if systolic BP fall more than 20mm Hg or if there is a sudden increase in pulse rate, w/hold medication and notify prescriber; inspect oral membranes daily; monitor bowel elimination pattern and I&O ratio; do not use OTC drugs unless your prescriber approves
Page 66 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
40. Selective Serotonin Reuptake Inhibitor (SSRI) 1.149. Citalopram Hydrobromide (Celexa) Class: Selective Serotonin Reuptake Inhibitor (SSRI) Actions: SSRI w/ an antidepressant effect presumed to be linked to its inhibition of CNS presynaptic neuronal uptake of serotonin. Peak: steady-state serum concentrations in 1wk; peak blood levels at 4hrs. Indications: Depression Norm. Dosage, Freq, Route, Range: PO start at 20mg/day, may increase to 40mg/day if needed Side Effects: nausea, dry mouth, insomnia, somnolence Nursing Considerations: watch closely for worsening of depression or emergence of suicidal ideations; Lab tests: monitor periodically hepatic function, CBC, serum sodium, and lithium levels when the two drugs are given concurrently; monitor periodically HR & BP, and carefully monitor complete cardiac status in person w/ known or cardiac disease; avoid alcohol
1.150. Escitalopram Oxalate (Lexapro) Class: Antidepressant; Selective Serotonin Reuptake Inhibitor (SSRI) Actions: antidepressant effect is presumed to be linked to its inhibition of CNS presynaptic neuronal uptake of serotonin. Onset: Approximately 1 wk. Peak: 3hr Half-life: 25hr Indications: depression, generalized anxiety disorder Norm. Dosage, Freq, Route, Range: PO 10mg daily, may increase to 20mg daily if needed after 1 wk Max: 20mg/day Side Effects: nausea, insomnia, somnolence, decreased libido Nursing Considerations: closely observe for worsening of depression or suicide, Lab tests: monitor periodically LFTs, serum sodium, and lithium levels, monitor periodically HR and BP and carefully monitor complete cardiac status
1.151. Fluoxetine HCL (Prozac) Class: Selective Serotonin Reuptake Inhibitor (SSRI), Antidepressant Actions: antidepressant effect is presumed to be linked to inhibition of CNS neuronal uptake of serotonin Indications: disorder
depression, gastric depression, OCD, bulimia, premenstrual dysphoric disorder, panic
Norm. Dosage, Freq, Route, Range: PO 20mg/day in AM, may increase by 20mg/day at weekly intervals Max: 80mg/day Side Effects: headache, nervousness, anxiety, insomnia, nausea, diarrhea Nursing Considerations: Monitor renal and hepatic functions. Supervise patients closely who are high suicide risks. Lab tests: periodic serum electrolytes, monitor closely plasma glucose in diabetes.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 67 of 75
Drug Med Cards
1.152. Paroxetine (Paxil, Pexeva) Class: Antidepressant; Selective Serotonin Reuptake Inhibitor (SSRI) Actions: It is highly potent and a highly selective inhibitor of serotonin reuptake by neurons in CNS. Onset: 2wks. Peak: 5-8hrs. Indications: Depression; OCD; Panic Attacks; Social Anxiety; Generalized Anxiety, PTSD; Premenstrual Dysphoric Disorder Norm. Dosage, Freq, Route, Range: PO 10-50mg/day Max: 80mg/day Side Effects: Headache, sedation, nausea, dry mouth Nursing Considerations: monitor for worsening of depression or emergence of suicidal ideation; monitor for significant weight loss; monitor pt. w/ history of mania for reactivation of condition; monitor pts. w/ preexisting cardiovascular disease carefully because paroxetine may adversely affect hemodynamics status
1.153. Sertraline HCL (Zoloft) Class: Antidepressant; Selective Serotonin Reuptake Inhibitor (SSRI) Actions: Effective in controlling depression, obsessive-compulsive disorder, anxiety, and panic disorder. Onset: 2-4 weeks Indications: Depression, Anxiety, Obsessive-Compulsive Disorder Norm. Dosage, Freq, Route, Range: begin w/ 50mg/day, gradually increase every few weeks according to response Max: 200mg/day Side Effects: agitation, insomnia, headache, dizziness, somnolence, fatigue Nursing Considerations: supervise patients at risk for suicide closely, monitor for worsening of depression or emergence of suicidal ideation, monitor older adults for fluid and sodium imbalances, monitor patients w/ a Hx of a seizure disorder closely, lab tests: monitor PT /INR w/ patients receiving concurrent warfarin therapy
1.154. Vilazodone (Vibryd) Class: Selective Serotonin Reuptake Inhibitor (SSRI); Psychotherapeutic Agent; Antidepressant Actions: Antidepressant is presumed to be linked to inhibition of CNS neuronal uptake of the neurotransmitter, serotonin. Peak: 4-5hrs. Indications: Major Depressive Disorder Norm. Dosage, Freq, Route, Range: PO initial dose of 10mg/day for 7 days, increase to 20mg/day for 7 days, then to 40mg/day Side Effects: dizziness, diarrhea, nausea Nursing Considerations: monitor for worsening of depression or emergence of suicidal ideation; supervise pts. Closely who are high suicide risks; do not stop medication abruptly
Page 68 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
41. Monoamine Oxidase Inhibitors (MAOIs) 1.155. Isocarboxazid (Marplan) Class: Antidepressant; MAOI Actions: Inhibits monoamine oxidase, the enzyme involved in the catabolism of catecholamine neurotransmitters and serotonin. Duration: up to 2wks. Indications: Refractory Depression Norm. Dosage, Freq, Route, Range: PO 10-30mg/day in 1-3 divided doses Max: 30mg/day Side Effects: drowsiness, overactivity, insomnia, orthostatic hypotension, paradoxical hypertension, blurred vision, nausea, constipation, anorexia, urinary retention, dry mouth Nursing Considerations: Monitor BP for orthostatic hypotension, monitor for therapeutic effectiveness, monitor and report promptly signs of clinical deterioration or suicidal ideation, check for peripheral edema daily and monitor weight several times weekly and monitor weight several times weekly, toxic symptoms from over-dosage or from substances or from ingestion of contraindicated substances (e.g., foods high in tyramine) may occur w/in hours
1.156. Phenelzine Sulfate (Nardil) Class: Antidepressant; MAOI Actions: potent hydrazine MAOI. Antidepressant action believed to be due to irreversible inhibition of MAOI, thereby permitting increased conxentrations of endogenous epinephrine, norepinephrine, serotonin, and dopamine w/in presynaptic neurons and at receptor sites. Onset: 2 weeks Indications: Depression Norm. Dosage, Freq, Route, Range: PO 1.5mg tid, rapidly increase to at least 60mg/day, may need up to 90mg/day Max: 90mg/day Side Effects: orthostatic hypotension, insomnia, respiratory depression, coma, hypertensive crisis, circulatory collapse, constipation, dry mouth, nausea, vomiting, anorexia, leukopenia Nursing Considerations: Monitor BP and Pulse, Lab tests: baseline and periodic CBC and LFTs; pts on prolonged therapy should be checked periodically for altered color perception, changes in fundi or visual fields, changes in red-green vision may be the 1st indication of eye damage, strict thymine diet
1.157. Tranylcypromine Sulfate (Parnate) Class: Antidepressant; MAOI Actions: Potent MAO w/ a antidepressant activity that arises from the increased availability of monoamines resulting from the inhibition of the enzyme MAO. This leads to increased concentration of neurotransmitters, such as epinephrine, norepinephrine, and dopamine in the CNS. Onset: 10 days Indications: Severe Depression Norm. Dosage, Freq, Route, Range: PO 30mg/day in 2 divided doses, may increase by 10mg/day at 23wk intervals Max: 60mg/day Side Effects: Orthostatic hypotension, hypertensive crisis Nursing Considerations: monitor BP closely, sever hypertensive reactions are known to occur with MAOIs; monitor for changes in behavior; do not eat tyramine-containing foods; be aware of excessive use of caffeine-containing beverages; make position changes slowly; avoid alcohol and other CNS depressants
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 69 of 75
Drug Med Cards
42. Anti-Emetic 1.158. Ondansetron HCL (Zofran) Class: 5-HT3 Anatagonist, Antiemetic Actions: Prevents nausea and vomiting associated with cancer chemotherapy and anesthesia. Peak: 11.5hr Half-life: 3hr Indications: prevention of nausea and vomiting associated with initiation and repeated courses of cancer chemotherapy, including high-dose cisplatin; postoperative nausea and vomiting Norm. Dosage, Freq, Route, Range: PO 8-24mg 30 min before chemotherapy, than q8hr times 2 more doses Side Effects: headache, sedation, diarrhea Nursing Considerations: monitor fluid and electrolyte status, cardiovascular status
Page 70 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
43. Antituberculosis 1.159. Isoniazid (INH, Laniazid) Class: Anti-infective; Antituberculosis Actions: Exerts bacteriostatic action against actively growing tubercle bacilli, may be bactericidal in higher concentrations. Peak: 1-2 hr Indications: Treatment of Active Tuberculosis, preventative therapy Norm. Dosage, Freq, Route, Range: PO/IM 5mg/kg Max: 300 mg/day Side Effects: Paresthesias, peripheral neuropathy, hepatotoxicity (elevated AST, ALT; bilirubinemia; jaundice; hepatitis) Nursing Considerations: Monitor for therapeutic effectiveness, w/hold drug and notify prescriber immediately of a hypersensitivity reaction, Lab tests: monitor LFTs periodically, monitor for and report signs of hepatotoxicity, monitor BP, check weight at least twice weekly under standard conditions
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 71 of 75
Drug Med Cards
44. Substance Abuse Deterrent 1.160. Acamprosate Calcium (Campral) Class: Substance Abuse Deterrent Actions: Reduces craving for alcohol intake due to chronic use, but does not cause alcohol aversion or a disulfiram-like reaction as a result of alcohol ingestion. Half-life: 20-33hr. Indications: Maintenance of Alcohol Abstinence Norm. Dosage, Freq, Route, Range: PO 666mg tid Side Effects: diarrhea, flatulence Nursing Considerations: Monitor S&S of depression or suicidal thinking; monitor or impaired judgment or thinking, dizziness or impaired motor skills; report promptly unusual anxiousness or nervousness, depression or suicidal thoughts, burning or tingling sensations in arms, legs, hands or feet, chest pains or palpitations, or difficulty urinating; report any alcohol consumption during therapy.
1.161. Antabuse Class: Enzyme Inhibitor; Anti-Alcoholic Agent Actions: Acts as a deterrent to alcohol ingestion by inhibiting the enzyme acetaldehyde dehydrogenase, which normally metabolizes alcohol in the body. Onset: Up to 12hr. Duration: Up to 2wk. Onset: Up to 12hr. Duration: Up to 2wk. Indications: Alcoholism Norm. Dosage, Freq, Route, Range: PO 500mg/day for 1-2wk, then 125-500mg/day Max: 500mg/day Side Effects: marked respiratory depression, unconsciousness, convulsions, sudden death, hepatotoxicity Nursing Considerations: Lab tests: baseline & follow-up transaminase studies every 10-14 days to detect hepatic dysfunction; treat pt. w/ severe disulfiram reaction as though in shock, monitor potassium levels, especially if pt. has diabetes mellitus; explain the danger of alcohol ingestion during treatment to pt.; report promptly to prescriber the onset of nausea w/ RUQ pain or discomfort, itching, jaundiced sclera or skin, dark urine or clay-colored stools, w/hold drug pending LFTs
Page 72 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
45. Bone Metabolism Regulatory 1.162. Pamidronate (Aredia) Class: Bisphosphonate (Bone Metabolism Regulatory) Actions: Reduces bone turnover and, when used in combination with adequate hydration, it increases renal excretion of calcium, thus reducing serum calcium concentrations. Onset: 24-48 hr Peak: 6 days Duration: 2 weeks-3months Indications: Moderate to severe hypercalcemia of malignancy, Paget’s Diease, Osteolytic Metastases Norm. Dosage, Freq, Route, Range: IV 60-90 mg infused over 4-24 hr, may repeat in 7 days Side Effects: fever w/ or w/o rigors, thrombophlebitis at injection site, hypocalcemia, epigastric discomfort Nursing Considerations: Assess IV injection site for thrombophlebitis, Lab tests: monitor serm calcium, phosphate, magnesium, and potassium at frequent intervals; CBC with defferential, Hct and Hgb; and kidney function tests throughout course of therapy, monitor for S&S of hypocalcemia, hypokalemia, hypomagnesemia and hypophosphatemia, monitor for seizures, monitor vital signs
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 73 of 75
Drug Med Cards
46. Bacterial Collagenase Enzyme 1.163. Collagenase Clostridum Histolyticum (Xiaflex) Class: Bacterial Collagenase enzyme Actions: Collagenases are proteinases that hydrolyze collagen in its native triple helical conformation under physiological conditions, resulting in lysis of collagen deposits. Indications: Dupuytren’s contracture, Peyronie’s Disease Norm. Dosage, Freq, Route, Range: Topical 1-3x daily to affected areas Side Effects: mild pain or tenderness in treated hand, cracked skin, under arm pain Nursing Considerations: call physician if fever, chills, body aches, flu symptoms, or swollen glands in your elbow or under arm, watch for bleeding, bruising, swelling, redness, warmth, numbness, tingling, or sudden pain or loss of movement
Page 74 of 75
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Drug Med Cards
Bibliography Ebersole, P., Hess, P., Touhy, T.A., Schmidt Logan, A., & Jett, K. (2008) Toward healthy aging: Human needs and nursing response ( 7th ed.). St. Louis, MO: Mosby. Eliopoulous C. (2009). Gerontological nursing. ( 7th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. Grodner, M., Long, S., & Walkingshaw,B.C. (2007). Foundations and clinical application of nutrition: A nursing approach ( 4th ed.). St. Louis, MO: Mosby. Ignatavicius, D. D., & Workman, M. L. (2010). Medical-Surgical nursing (6th ed.). St. Louis, MO: Saunders. Lowdermilk, D.L.,& Perry, S.E. ( 2007) . Maternity & women’s health care (9th ed.). St. Louis, MO: Mosby. Lehne, R.A. (2010). Pharmacology for nursing care (7th ed.). St. Louis, MO: Saunders. Lilley, L. L., Harrington, S., & Snyder, J.S. (2007). Pharmacology and the nursing process (5th ED.). St. Louis, MO: Mosby. Roach, S. S.,& Ford, S. M. (2008). Introductory clinical pharmacology. Philadelphia, PA: Lippincott Williams & Wilkins. Smeltzer, S. C., Bare, B.G., Hinkle, J. L., & Cheever, K.H. ( 2008). Brunner and Suddarth’s textbook of medical-surgical nursing ( 11th ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Simplenursing.com 60% Less Study Time, Less Stress More Success!
Page 75 of 75
Acyclovir
Amantadine HCl
(Zovirax)
(Symmetrel)
Class: Antiviral
Class: Antiviral; Central-Acting Cholinergic Receptor Antagonist; Antiparkinson
Actions: reduces viral shedding and formation of new lesions and speeds healing time. Peak: 1.5-2hr. Half-life: 2.5-5hr.
Actions: Because Amantadine does not suppress antibody formation, it can be istered for interim protection in combination w/ influenza. Onset: w/in 48hrs. Peak: 1-4hrs
Indications: (IV treatment) viral encephalitis, herpes simplex, varicella-zoster virus (shingles/chickpox); (orally) herpes simplex, varicella-zoster virus; (topically) herpes labialis (cold sores) and initial episodes of herpes gentitalis
Indications: Influenza A Treatment; Influenza A Preventative; Parkinsonism; DrugInduced Extrapyramidal Symptoms (EPS)
Norm. Dosage, Freq, Route, Range: PO 400mg bid Max: 800mg/day
Norm. Dosage, Freq, Route, Range: PO 100mg 1-2times/day
Side Effects: headache, nausea, vomiting, diarrhea
Side Effects: dizziness, light-headedness, difficulty in concentrating, insomnia, leukopenia
Nursing Considerations: Monitor I&O & hydration status. Lab tests: baseline and periodic renal function tests
Nursing Considerations: Lab tests: pH and serum electrolytes; monitor and report mental status changes, nervousness, difficulty concentrating, or insomnia, loss of seizure control, S&S of toxicity, especially in doses over 200mg/day
Alprazolam
Diazepam
(Xanax)
(Diastat, Valium)
Class: Anxiolytic; Sedative-Hypnotic; Benzodiazepine
Class: Benzodiazepine Anticonvulsant; Anxiolytic
Actions: A CNS depressant that appears to act at the limbic, thalamic, and hypothalamic levels of the CNS. Has antianxiety and sedative effects w/ addictive potential. Peak: 1-2 hr. Halh-life: 12-15 hr.
Actions: Long-acting benzodiazepine psychotherapeutic agent. Benzodiazepines act at the limbic. Thalamic, and hypothalamic regions of the CNS and produce CNS depression resulting in sedation, and anticonvulsant activity dependent on the dosage. Onset: PO 30-60 min Peak: PO 1-2 hr Duration: IV 15 min-1 hr PO up to 3 hr
Indications: Anxiety Disorders, Panic Attacks Indications: Status Epilepticus, Muscle Spasm, Anxiety, Alcohol Withdrawal, Pre-op Norm. Dosage, Freq, Route, Range: PO 0.25-5 mg tid Max: 4 mg/day Norm. Dosage, Freq, Route, Range: IV/IM 5-10 m, repeat if needed at 10-15 min intervals up to 30 mg, then repeat if needed q2-4hr
Side Effects: Drowsiness, sedation Nursing Considerations: Monitor S&S of drowsiness and sedation, especially in older adults or the debilitated, Lab tests: CBC, urinalysis and blood chemistry studies particularly during continuing therapy
Side Effects: Drowsiness, fatigue, confusion, vivid dreams, headache Nursing Considerations: Monitor for adverse reactions, Monitor for therapeutic effectiveness-max effect may require 1-2 week, monitor for and report promptly signs of suicidal ideation especially in those treated for anxiety states accompanied by depression, observe patient closely and monitor vital signs when diazepam is given parentally; hypotension, muscular weakness, tachycardia, and respiratory depression may occur, Lab tests: periodic CBC and LFTs
Lorazepam
Temazepam
(Ativan)
(Restoril)
Class: Anxioltic; Sedative-Hypnotic; Benzodiazepine
Class: Benzodiazepine, Anxiolytic, Sedative-Hypnotic
Actions: most potent of the available benzodiazepine. Effects (antianxiety, sedative, hypnotic, and skeletal muscle relaxant) are mediated by the inhibition neurotransmitter GABA. Action sites are thalamic, hypothalamic, and limbic levels of CNS. Onset: IV 1-5 min. IM 15-30 min. Peak: IM 60-9 min. PO 2 hr Duration 12-24 hr
Actions: reduces night awakenings and early morning awakenings; increases total sleep times, absence of rebound effects. Onset: 30-50 min. Peak: 2-3hr. Duration: 10-12hr. Half-life: 8-24hr Indications: to relieve insomnia
Indications: Antianxiety, Insomnia, Premedication, Status Epilepticus Norm. Dosage, Freq, Route, Range: PO 7.5-30mg at bedtime Max: 30mg/night Norm. Dosage, Freq, Route, Range: PO 2-6 mg/day in divided doses Max: 10 mg/day Side Effects: drowsiness, sedation, dizziness, weakness Nursing Considerations: Supervise ambulation, Lab tests: Assess CBC and LFTs periodically
Side Effects: drowsiness, dizziness, lethargy Nursing Considerations: hypersensitivity, Lab tests: LFTs and kidney function tests during long-term use, be aware of S&S of overdose: weakness, confusion, slurred speech, ataxia, coma w/ reduced or absent reflexes, hypertension and respiratory depression