This document was ed by and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this report form. Report 3b7i
Overview 3e4r5l
& View Soap Note Directions & Abbreviations as PDF for free.
More details w3441
- Words: 1,268
- Pages: 4
SOAP Notes (excerpt from 2015-2016 Orientation Guide for COMLEX-USA Level 2-PE)
The SOAP Note represents an opportunity to demonstrate documentation skills (in English), document clinical findings, exercise clinical problem-solving skills, formulate a differential diagnosis and a diagnostic and treatment plan. It is acceptable to use either a narrative or a more “bullet” or “laundry list” style for the notes, provided they are documented in English. The “S” is for the subjective components, the “O” for objective findings, the “A” for the assessment/differential diagnosis, and the “P” for the plan. Candidates are instructed to document significant findings from the patient’s history in the “Subjective” portion, and physical examination findings and any other key objective findings in the “Objective” portion. Candidates should try to be as specific as possible when documenting physical findings, avoiding the word “normal”. With the exception of vital signs provided, under no other circumstances should a candidate document results of physical examination maneuvers or techniques that were not performed, or medical history that was not elicited. Documenting results of physical examination maneuvers that were not performed, or medical history that was not elicited will be considered irregular conduct and will be thoroughly investigated and dealt with according to NBOME’s policies and procedures (see “Professionalism” section below). For the “Assessment” section, candidates will be evaluated on the ability to make an accurate or plausible diagnosis, as well as to list at least two other diagnostic possibilities for the patient’s presenting problem. This should be listed in a “Differential Diagnoses” format, with the most likely diagnosis for the presenting concern/symptom/issue listed first. Even if the diagnosis is fairly certain or the presenting problem is more for health promotion and disease prevention, candidates should consider and document at least three potential diagnoses or etiologies in this section. For “health promotion / disease prevention visit” types of encounters, if providing a differential diagnosis would not be relevant, candidates may list the patient’s problems in a “problem list” format, or list relevant risk factors for the area of concern. For the “Plan” component, candidates should note any workup or treatment that he/she would propose for the patient, including questions or physical exam maneuvers that you inadvertently did not ask or perform, but would plan to if time allowed. In most cases, specific drugs or drug dosages are not required, but candidates should try to be as specific as possible when referring to diagnostic tests (e.g., serum electrolytes, BUN, creatinine, and glucose as opposed to “blood tests”, “SMA7”, or “Chemistry ”). All SOAP Notes should be completed to “stand alone” as the only documentation for that encounter, as information on the scrap paper or doorway information sheet will not be considered as part of the required documentation. Candidates should be careful to adhere to the nine minute time limitation on completing their SOAP Notes. The e-SOAP note keyboard will be disabled at the conclusion of the 9 minute completion period. It is generally advisable to avoid or limit abbreviations in medical documentation due to the lack of standardization and the potential for medical error. If a candidate desires to do so, it is advisable to use only those abbreviations that are considered standardized and would be easily recognized by the osteopathic physician examiners scoring the SOAP Notes. Common English language or medical abbreviations are
2015-2016 Orientation Guide for COMLEX-USA Level 2-PE included in the Common Abbreviation List, which will be available at each SOAP Note writing desk throughout the examination. The use of uncommon, obscure, confusing and idiosyncratic abbreviations runs the risk of misinterpretation by the physician examiner, which could negatively impact the score on the note.
SOAP Note Directions (similar to the posting at each desk) Complete a note documenting your findings in the text boxes provided. Please do not type your name on the note. Note that overall synthesis and linkage, organization and accuracy is important as notes are scored by physician examiners. Limit abbreviations to avoid confusion for the examiners; a “Common Abbreviations List” is provided for your reference. With the exception of vital signs provided, under no other circumstances should you document results of physical examination maneuvers or techniques that were not performed or medical history that was not elicited. S = Subjective findings List patient input regarding the problem(s), medical history, etc. O = Objective findings List data from your physical examination, lab or imaging studies, etc. A = Assessment This is your impression as to the diagnosis, listing at least three possible etiologies for the patient problem/symptom or concern. Rank in order of likelihood for the given case. For well visits, list at least three problems or risk factors. P = Plan This is your plan for preliminary work-up and treatment (indicated diagnostic investigations, other history and physical exam data you would gather & therapeutic interventions). Specific drug dosages are generally not required, but be as specific as possible when referring to diagnostic tests.
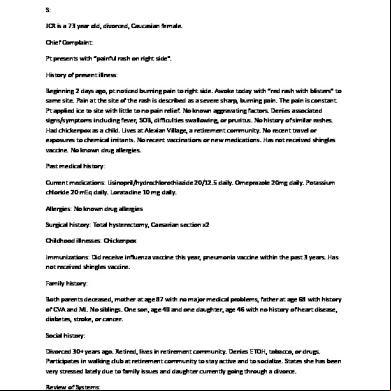
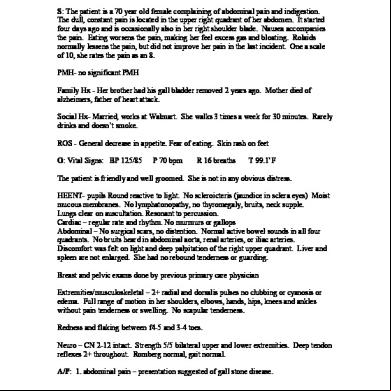
2015-2016 Orientation Guide for COMLEX-USA Level 2-PE A completed SOAP Note example (not necessary exemplary) is provided below:
There is an e-SOAP Note practice module available on the NBOME website: Click here to access the site By visiting the site, you will learn how to get the most out of the SOAP Note online practice resources available. The brief tutorial will guide you through the features and navigation of the electronic SOAP Note used at the NCCST. There is also a sample encounter video that can be used as a base for the content of your practice note, as well as the Doorway Information sheet and an example of a completed SOAP Note.
2015-2016 Orientation Guide for COMLEX-USA Level 2-PE SOAP NOTE – Common Abbreviations It is recommended that you spell out names and rather than abbreviate when creating your SOAP notes. However, if you desire, you may use common abbreviations when creating your notes, similar to those listed below. Avoid abbreviations that might lead to medical errors. Abd AIDS ETOH b BMI BUN CCU R CVA Cspine CXR cc: COPD CTA c/o CBC CT CHF CABG DTR DM ENT ECG or EKG ED EMT E EOM Ext FH f F GI GU HEENT HVLA hx h/o HIV HTN JVD KUB L
abdomen acquired immune deficiency syndrome alcohol black body mass index blood urea nitrogen cardiac care unit cardiopulmonary resuscitation cerebrovascular accident cervical spine chest x-ray chief complaint chronic obstructive pulmonary disease clear to auscultation complaining of complete blood count computed tomography congestive heart failure coronary artery by grafting deep tendon reflexes diabetes mellitus ears, nose and throat electrocardiogram emergency department emergency medical technician extended extraocular muscles extremities family history female flexed gastrointestinal genitourinary head, eyes, ears, nose and throat high velocity, low amplitude history history of human immunodeficiency virus hypertension Jugular venous distention kidney, ureter, and bladder left
LMP LP Lspine MRI m Meds MVA MI Neuro NKA NKDA NIDDM NSR Po OMT Ppd PTT PMH PSH PE +
last menstrual period
PT PERLA ROM RBC RRR ROS R ROT RO SB SH Tspine TIA US URI U/A W WBC WNL Yo
prothrombin time
lumbar puncture lumbar spine magnetic resonance imaging male medications motor vehicle accident myocardial infarction negative neurologic no known allergies no known drug allergies non insulin-dependent diabetes mellitus normal sinus rhythm orally osteopathic manipulative treatment packs per day partial thromboplastin time past medical history past surgical history physical examination positive
pupils equal, react to light and accommodation range of motion red blood cells regular rate and rhythm review of systems right rotated rule out side bent social history thoracic spine transient ischemic attack ultrasound upper respiratory tract infection urinalysis white white blood cells within normal limits year-old
The SOAP Note represents an opportunity to demonstrate documentation skills (in English), document clinical findings, exercise clinical problem-solving skills, formulate a differential diagnosis and a diagnostic and treatment plan. It is acceptable to use either a narrative or a more “bullet” or “laundry list” style for the notes, provided they are documented in English. The “S” is for the subjective components, the “O” for objective findings, the “A” for the assessment/differential diagnosis, and the “P” for the plan. Candidates are instructed to document significant findings from the patient’s history in the “Subjective” portion, and physical examination findings and any other key objective findings in the “Objective” portion. Candidates should try to be as specific as possible when documenting physical findings, avoiding the word “normal”. With the exception of vital signs provided, under no other circumstances should a candidate document results of physical examination maneuvers or techniques that were not performed, or medical history that was not elicited. Documenting results of physical examination maneuvers that were not performed, or medical history that was not elicited will be considered irregular conduct and will be thoroughly investigated and dealt with according to NBOME’s policies and procedures (see “Professionalism” section below). For the “Assessment” section, candidates will be evaluated on the ability to make an accurate or plausible diagnosis, as well as to list at least two other diagnostic possibilities for the patient’s presenting problem. This should be listed in a “Differential Diagnoses” format, with the most likely diagnosis for the presenting concern/symptom/issue listed first. Even if the diagnosis is fairly certain or the presenting problem is more for health promotion and disease prevention, candidates should consider and document at least three potential diagnoses or etiologies in this section. For “health promotion / disease prevention visit” types of encounters, if providing a differential diagnosis would not be relevant, candidates may list the patient’s problems in a “problem list” format, or list relevant risk factors for the area of concern. For the “Plan” component, candidates should note any workup or treatment that he/she would propose for the patient, including questions or physical exam maneuvers that you inadvertently did not ask or perform, but would plan to if time allowed. In most cases, specific drugs or drug dosages are not required, but candidates should try to be as specific as possible when referring to diagnostic tests (e.g., serum electrolytes, BUN, creatinine, and glucose as opposed to “blood tests”, “SMA7”, or “Chemistry ”). All SOAP Notes should be completed to “stand alone” as the only documentation for that encounter, as information on the scrap paper or doorway information sheet will not be considered as part of the required documentation. Candidates should be careful to adhere to the nine minute time limitation on completing their SOAP Notes. The e-SOAP note keyboard will be disabled at the conclusion of the 9 minute completion period. It is generally advisable to avoid or limit abbreviations in medical documentation due to the lack of standardization and the potential for medical error. If a candidate desires to do so, it is advisable to use only those abbreviations that are considered standardized and would be easily recognized by the osteopathic physician examiners scoring the SOAP Notes. Common English language or medical abbreviations are
2015-2016 Orientation Guide for COMLEX-USA Level 2-PE included in the Common Abbreviation List, which will be available at each SOAP Note writing desk throughout the examination. The use of uncommon, obscure, confusing and idiosyncratic abbreviations runs the risk of misinterpretation by the physician examiner, which could negatively impact the score on the note.
SOAP Note Directions (similar to the posting at each desk) Complete a note documenting your findings in the text boxes provided. Please do not type your name on the note. Note that overall synthesis and linkage, organization and accuracy is important as notes are scored by physician examiners. Limit abbreviations to avoid confusion for the examiners; a “Common Abbreviations List” is provided for your reference. With the exception of vital signs provided, under no other circumstances should you document results of physical examination maneuvers or techniques that were not performed or medical history that was not elicited. S = Subjective findings List patient input regarding the problem(s), medical history, etc. O = Objective findings List data from your physical examination, lab or imaging studies, etc. A = Assessment This is your impression as to the diagnosis, listing at least three possible etiologies for the patient problem/symptom or concern. Rank in order of likelihood for the given case. For well visits, list at least three problems or risk factors. P = Plan This is your plan for preliminary work-up and treatment (indicated diagnostic investigations, other history and physical exam data you would gather & therapeutic interventions). Specific drug dosages are generally not required, but be as specific as possible when referring to diagnostic tests.
2015-2016 Orientation Guide for COMLEX-USA Level 2-PE A completed SOAP Note example (not necessary exemplary) is provided below:
There is an e-SOAP Note practice module available on the NBOME website: Click here to access the site By visiting the site, you will learn how to get the most out of the SOAP Note online practice resources available. The brief tutorial will guide you through the features and navigation of the electronic SOAP Note used at the NCCST. There is also a sample encounter video that can be used as a base for the content of your practice note, as well as the Doorway Information sheet and an example of a completed SOAP Note.
2015-2016 Orientation Guide for COMLEX-USA Level 2-PE SOAP NOTE – Common Abbreviations It is recommended that you spell out names and rather than abbreviate when creating your SOAP notes. However, if you desire, you may use common abbreviations when creating your notes, similar to those listed below. Avoid abbreviations that might lead to medical errors. Abd AIDS ETOH b BMI BUN CCU R CVA Cspine CXR cc: COPD CTA c/o CBC CT CHF CABG DTR DM ENT ECG or EKG ED EMT E EOM Ext FH f F GI GU HEENT HVLA hx h/o HIV HTN JVD KUB L
abdomen acquired immune deficiency syndrome alcohol black body mass index blood urea nitrogen cardiac care unit cardiopulmonary resuscitation cerebrovascular accident cervical spine chest x-ray chief complaint chronic obstructive pulmonary disease clear to auscultation complaining of complete blood count computed tomography congestive heart failure coronary artery by grafting deep tendon reflexes diabetes mellitus ears, nose and throat electrocardiogram emergency department emergency medical technician extended extraocular muscles extremities family history female flexed gastrointestinal genitourinary head, eyes, ears, nose and throat high velocity, low amplitude history history of human immunodeficiency virus hypertension Jugular venous distention kidney, ureter, and bladder left
LMP LP Lspine MRI m Meds MVA MI Neuro NKA NKDA NIDDM NSR Po OMT Ppd PTT PMH PSH PE +
last menstrual period
PT PERLA ROM RBC RRR ROS R ROT RO SB SH Tspine TIA US URI U/A W WBC WNL Yo
prothrombin time
lumbar puncture lumbar spine magnetic resonance imaging male medications motor vehicle accident myocardial infarction negative neurologic no known allergies no known drug allergies non insulin-dependent diabetes mellitus normal sinus rhythm orally osteopathic manipulative treatment packs per day partial thromboplastin time past medical history past surgical history physical examination positive
pupils equal, react to light and accommodation range of motion red blood cells regular rate and rhythm review of systems right rotated rule out side bent social history thoracic spine transient ischemic attack ultrasound upper respiratory tract infection urinalysis white white blood cells within normal limits year-old