Breech Presentation 5n51p
This document was ed by and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this report form. Report 3b7i
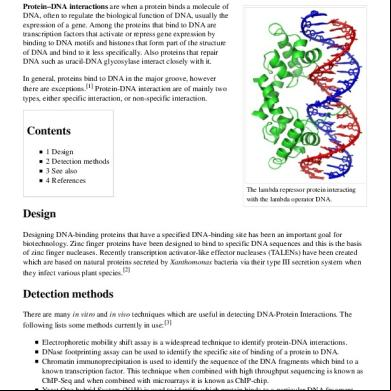
Overview 3e4r5l
& View Breech Presentation as PDF for free.
More details w3441
- Words: 2,258
- Pages: 57
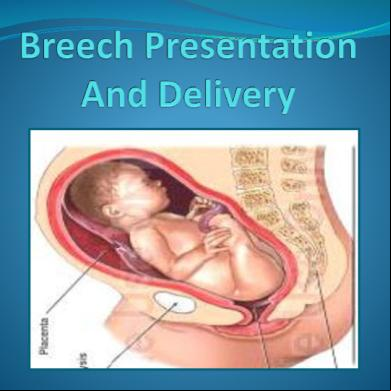
Breech Presentation Commonest malpresentation. The incidence is highly dependent on the gestational age. At 28 weeks about 20 % preganacies, at 34 weeks, 5 %. By full term, the incidence is about 3%.
Etiology Factors that appear to predispose to breech presentation Prematurity – commonest cause Polyhydramnios / oligohydramnios Lax abdominal wall associated with great parity Multiple fetuses Hydrocephalus , Anencephaly Pelvic tumor Placenta implantation at cornual-fundal region Uterine abnormalities - Malformation, fibroids Fetal abnormalities - CNS Malformations; Neck Masses , IUD Previous breech delivery
Types Of Breech • Complete (10%) : The hips
and knees are flexed • Incomplete (25%) : due to varying degrres of extension of thighs or legs. - Frank (65%) : Hips are flexed, knees are extended. - Footling : one of the lower extremities is lowermost. - Knee : one /both knee are lowermost
Clinical Varieties Complicated breech Complicated breech delivery
Positions Sacrum – denominator. Anterior positions - sacrum towards iliopubic eminence.
L.S.A. R.S.A. Posterior positions - sacrum towards sacro-iliac t. R.S.P. L.S.P.
Diagnosis Abdominal examination –
– Hard round and ballotable fetal head is found to occupy the fundus – FHS heard loudest above the umbilicus
Leopold Maneuvers
Diagnosis Vaginal examination Frank breech • Both ischial tuberosities, sacrum and anus are palpable • The mouth and malar eminences form triangular shape in face whereas the ischial tuberosities and anus are in straight line. Complete breech • Feet & external genitalia may be felt alongside the buttock Incomplete breech • One or both feet are inferior to the buttock. Foot can be differentiated from hand by position of thumb & prominence of heel.
Diagnosis Imaging technique – Ultrasound • Confirms a clinically suspected breech presentation and fetal anomalies, liquor, placental localization • If vaginal delivery is considered – Type of breech presentation – Degree of flexion or deflexion of head
Mechanism of labor Mechanism of labor Delivery of buttocks Delivery of shoulders Delivery of aftercoming head
Mechanism of labor in L.S.A. Delivery of buttocks – Engagement and descent of breech – Bitrochanteric diameter (10 cm) in lt. oblique diameter of inlet Internal rotation of breech towards sacrum through 45° – Bitrochanteric diameter in anteroposterior pelvic diameter Descent on perineum Lateral flexion of body – Forced by perineal floor – delivery Restitution of breech to relive torsion on trunk
Mechanism of labor in L.S.A. Delivery of shoulders Engagement - Bisacromial diameter in lt. oblique diameter Internal rotation of shoulder – Bisacromial in AP diameter External rotation of the trunk Delivery of posterior followed by anterior shoulders Restitution to relive the torsion on neck
Mechanism of labor in L.S.A. Delivery of aftercoming head – Flexion of head upon the thorax Engagement of head – suboccipitofrontal (10 cm) in Rt. oblique diameter of inlet ( rarely transverse ) Internal rotation of occiput through 45o or 90o as to bring the occiput behind pubic symphysis Further descent so that subocciput hinges under pubic symphysis Delivery of head by flexion – chin – mouth - face - brow – vertex – occiput succesively
Antenatal Management Identification of complicating factors ECV Selection of patient for vaginal delivery
ECV External cephalic version : The object of this procedure is to substitute a vertex for a less favourable presentation Indication : The common indication for external cephalic version is a breech or shoulder presentation diagnosed in the last weeks of pregnancy. Timing : A majority of the malpresentations correct themselves by the 34th week of pregnancy. Therefore, it is advisable to correct, by external version, breech and shoulder presentations found persisting after 34 weeks. Correction could also be done prior to 34 weeks but more often the abnormal presentation recurs.
ECV Prerequisites: - Before resorting to this procedure it is necessary to make sure that 1) the abdominal wall is sufficiently thin to permit accurate palpation, 2) the uterus is lax and contains sufficient liquor to help easy mobility of the fetus, 3) the membranes have not ruptured, and 4) the presenting part is not deeply engaged. 5) Anti D Immunoglobulin in non immunized Rh-negative mother
ECV Contraindications A large baby, major congenital anomalies, IUD Significant contraction of the pelvis, Antepartum hemorrhage, Obstetric complications - Pre-eclampsia, multiple pregnancy Previous caesarean section scar Uterine malformation PROM
ECV Technique: It is best to avoid anesthesia. The patient’s abdomen is bared and the presentation and position of the fetus are carefully ascertained. Each hand then seizes each of the fetal poles. The cephalic pole is then gently manipulated toward the pelvic inlet while the other is moved in the opposite direction. By a series of gentle stroking and pushing movements the head is brought over the pelvic brim. To keep it in position, an abdominal pad and binder may be applied.
ECV During the manipulations - which should always be gentle, The fetal heart should be auscultated frequently. Any significant alterations in the fetal heart rate should be taken as a warning, and it would be wise not to proceed with the version. As far as possible the attitude of flexion in the fetus must be maintained. Follow up – These patients should be re-examined a few days later (1 week)when if needed, version may be tried again. External version can be attempted early in labour also, and chances of recurrence of the malpresentation are very much reduced.
ECV Causes of failure of version : Frank breech, Oligohydramnios Large baby, Obesity Short cord Complications : Abruption PPROM Preterm labor Entanglement of cord around fetal parts & formation of true knot Fetomaternal haemorrhage Amniotic fluid embolism
Management During Labor
Types of Delivery -
Vaginal delivery: - Spontaneous - Partial breech extraction - Total breech extraction Cesarean of delivery
Types Of Vaginal Breech Delivery • •
•
Spontaneous breech (rare) : No manipulation of the infant is necessary, other than ing the infant. Assisted breech delivery (Partial breech extraction) : lower half of Fetus (upto umbilicus) descends spontaneously at the vaginal introitus; then the fetus is extracted completely. Total breech extraction : The entire body is extracted. This is indicated only if there is evidence of fetal distress unresponsive to routine maneuvers and a cesarean delivery is not possible.
Conditions Unfavorable For Vaginal Delivery Fetus weight more than 3500 g Unfavorable pelvis – Breech delivery does not allow sufficient time for molding of the fetal head; thus a platypelloid or android pelvis decreases ability of fetal head to navigate maternal pelvis Hyperextension of the head – increases risk of cervical spine injury Footling - incidence of umbilical cord prolapse increases with coiling of the umbilical cord around the legs of the fetus
Indications For Cesarean Delivery Primi with breech Footling breech Any degree of contraction or unfavorable shape of pelvis
Hyperextended head When delivery is indicated in the absence spontaneous
labor A large fetus Healthy ,viable preterm fetus with mother in active labor Severe IUGR Lack of an experienced operator
Vaginal Delivery Prerequisites – Multipara patient with previous normal delivery Uncomplicated breech presentation Estimated fetal weight – 1.5 – 3.5 kg Pelvic adequacy Flexed head Experienced operator
Management Of Labor No place for induction of labor Rapid assessment of the patient
– Satisfactory progress in labor is the best indicator of pelvic adequacy – Close surveillance FHR and Uterine Contraction Assessment of fetal condition – USG to detect anomalies and extended head if vaginal delivery is planned – Monitoring FHS every 15 min, – When membranes rupture, per vaginum examination to check for cord prolapse,
Breech Vaginal Delivery The anterior buttock appears at the introitus A mediolateral episiotomy Further descent of the anterior buttock
Both buttocks come into view. The buttocks are expelled by
voluntary maternal effort. The fetal sacrum rotates anteriorly.
Breech Vaginal Delivery
Breech Vaginal Delivery The legs are delivered by flexion of the thighs and knees.
Assisted Delivery Of Frank Breech Moderate traction exerted by finger in each groin and
facilitated by generous episiotomy Pinard maneuver - Two fingers are inserted along one
extremity to the knee , then pushed away from midline after spontaneous flexion to deliver a foot into vagina
Assisted Delivery Of Frank Breech Both groin method
Pinard maneuver
Breech Vaginal Delivery No downward or outward traction is applied until the
umbilicus has been reached A towel wrapped around the fetal hips, gentle downward and outward traction in conjunction with maternal expulsive efforts until the scapula is reached Don’t elevate body and keep the body low.
Assisted Vaginal Breech Delivery After the scapula is reached,
the fetus should be rotated 90° in order to deliver the anterior arm. The anterior arm is followed to the elbow, and the arm is swept out of the vagina.
Assisted Vaginal Breech Delivery The fetus is rotated 180°,
and the contralateral arm is delivered. The infant is then rotated 90° to the backup position in preparation for delivery of the head.
Breech Vaginal Delivery • Delivery of the anterior shoulder - delivery of the posterior shoulder.
• Back is kept anterior. • The trunk is allowed to hang to encourage descent of the head.
Delivery Of The Aftercoming Head Modified Mauriceau – Smellie - Veit maneuver Burns-Marshall method Forceps
Prague maneuver
Modified Mauriceau – Smellie – Veit Maneuver Modified Mauriceau – Smellie – Veit maneuver – (Jaw
flexion shoulder traction ) – Baby placed on supinated left forearm with limbs on either side – Index and middle finger of one hand are applied over maxilla to flex the head (originally index finger was introduced in the mouth, not done to avoid dislocation of jaw). – Use the other hand to grasp the baby’s shoulders. – Downward traction until subocciput appears beneath the PS – Elevate body toward maternal abdomen. – Head flexion maintained by suprapubic pressure given by assistant.
Burns-Marshall Method Burns-Marshall method:
Fetus is left hanging. Its weight will exert traction -- when occiput appears under symphysis, fetus is grasped by feet and elevated upwards towards mother’s abdomen.
Forceps Forceps – Application of Piper forceps, employing towel
sling . The forceps are introduced from below, left blade first aiming directly for intended positions on sides of the head. Suspension of body in a towel effectively holds the fetus and help keep the arm out of the way Type: Piper’s forceps which have long shank, perineal curve
Long Shank
Perineal Curve
Piper Forceps Advantages:
1- Promotion of flexion 2- Traction is directly applied on head preventing overstretch of neck so protecting roots of brachial plexus 3- Prevention of sudden compression and decompression of head thus preventing ICH 4- Protection of head from injury by projecting ischial spines in cases of mild degrees of contracted pelvis
Difficulties Extended arm (nuchal arm) Entrapment Of Aftercoming Head
Lovset's Maneuver Extended Arm (nuchal arm) Prerequisites- inferior angle of scaula is visible underneath the pubic arch Anaesthesia – not required as intrauterine manipulation is nil. Principle: The maneuver is based on the fact that the posterior shoulder enters the pelvic cavity before the anterior because of the curved birth canal. If the fetal body is rotated with slight traction keeping back anterior through 180° posterior shoulder will appear below the pubic symphysis.
Lovset's Maneuver Technique - The fetal body is lifted slightly and ed
by the obstetrician's hands, and is rotated with slight traction through 180° (keeping back anterior), so that the posterior shoulder comes to lie in front. Since it is on a lower level than the anterior shoulder, it will deliver spontaneously or may be hooked out. The other shoulder may deliver spontaneously. If it is not delivered, the body of the child is now rotated through 180° in the opposite direction, so that the other arm is brought into the anterior position again, and the arm and shoulder are born spontaneously. The back then to be rotated to lie anteriorly.
Entrapment Of Aftercoming Head Prague maneuver – in occipitoposterior Dührssen incision - Incision at 10 o’clock , 2 o’clock and
may required at 6 o’clock Symphysiotomy - rarely use, serious maternal injury
Prague Maneuver Prague maneuver – Rarely, the back of the fetus is
posterior. Prague maneuver Consists of two fingers of one hand grasping the shoulders of the back-down fetus from below while the other hand draws the feet up over maternal abdomen.
Maternal Complications Increase risk of infection - caused by manual
manipulation within birth canal Maternal injuries - Rupture of uterus and cervical laceration - intrauterine maneuver, delivery of after coming head through an incompletely dilate cervix - Deep perineal tear - Extension of episiotomy
Perinatal Complications Fetal injuries from difficult delivery-
Intracranial haemorrhage – tentorium cerebelli tear Fracture humerus, clavicle & femur Hematoma of sternocleidomastoid muscle Dislocations – hip t, cervical vertebrae, mandible Brachial plexus injuries (paralysed arm) Visceral injuries LBW from preterm delivery, IUGR or both Cord prolapse Anomalies Operative intervention, especially cesarean delivery
Etiology Factors that appear to predispose to breech presentation Prematurity – commonest cause Polyhydramnios / oligohydramnios Lax abdominal wall associated with great parity Multiple fetuses Hydrocephalus , Anencephaly Pelvic tumor Placenta implantation at cornual-fundal region Uterine abnormalities - Malformation, fibroids Fetal abnormalities - CNS Malformations; Neck Masses , IUD Previous breech delivery
Types Of Breech • Complete (10%) : The hips
and knees are flexed • Incomplete (25%) : due to varying degrres of extension of thighs or legs. - Frank (65%) : Hips are flexed, knees are extended. - Footling : one of the lower extremities is lowermost. - Knee : one /both knee are lowermost
Clinical Varieties Complicated breech Complicated breech delivery
Positions Sacrum – denominator. Anterior positions - sacrum towards iliopubic eminence.
L.S.A. R.S.A. Posterior positions - sacrum towards sacro-iliac t. R.S.P. L.S.P.
Diagnosis Abdominal examination –
– Hard round and ballotable fetal head is found to occupy the fundus – FHS heard loudest above the umbilicus
Leopold Maneuvers
Diagnosis Vaginal examination Frank breech • Both ischial tuberosities, sacrum and anus are palpable • The mouth and malar eminences form triangular shape in face whereas the ischial tuberosities and anus are in straight line. Complete breech • Feet & external genitalia may be felt alongside the buttock Incomplete breech • One or both feet are inferior to the buttock. Foot can be differentiated from hand by position of thumb & prominence of heel.
Diagnosis Imaging technique – Ultrasound • Confirms a clinically suspected breech presentation and fetal anomalies, liquor, placental localization • If vaginal delivery is considered – Type of breech presentation – Degree of flexion or deflexion of head
Mechanism of labor Mechanism of labor Delivery of buttocks Delivery of shoulders Delivery of aftercoming head
Mechanism of labor in L.S.A. Delivery of buttocks – Engagement and descent of breech – Bitrochanteric diameter (10 cm) in lt. oblique diameter of inlet Internal rotation of breech towards sacrum through 45° – Bitrochanteric diameter in anteroposterior pelvic diameter Descent on perineum Lateral flexion of body – Forced by perineal floor – delivery Restitution of breech to relive torsion on trunk
Mechanism of labor in L.S.A. Delivery of shoulders Engagement - Bisacromial diameter in lt. oblique diameter Internal rotation of shoulder – Bisacromial in AP diameter External rotation of the trunk Delivery of posterior followed by anterior shoulders Restitution to relive the torsion on neck
Mechanism of labor in L.S.A. Delivery of aftercoming head – Flexion of head upon the thorax Engagement of head – suboccipitofrontal (10 cm) in Rt. oblique diameter of inlet ( rarely transverse ) Internal rotation of occiput through 45o or 90o as to bring the occiput behind pubic symphysis Further descent so that subocciput hinges under pubic symphysis Delivery of head by flexion – chin – mouth - face - brow – vertex – occiput succesively
Antenatal Management Identification of complicating factors ECV Selection of patient for vaginal delivery
ECV External cephalic version : The object of this procedure is to substitute a vertex for a less favourable presentation Indication : The common indication for external cephalic version is a breech or shoulder presentation diagnosed in the last weeks of pregnancy. Timing : A majority of the malpresentations correct themselves by the 34th week of pregnancy. Therefore, it is advisable to correct, by external version, breech and shoulder presentations found persisting after 34 weeks. Correction could also be done prior to 34 weeks but more often the abnormal presentation recurs.
ECV Prerequisites: - Before resorting to this procedure it is necessary to make sure that 1) the abdominal wall is sufficiently thin to permit accurate palpation, 2) the uterus is lax and contains sufficient liquor to help easy mobility of the fetus, 3) the membranes have not ruptured, and 4) the presenting part is not deeply engaged. 5) Anti D Immunoglobulin in non immunized Rh-negative mother
ECV Contraindications A large baby, major congenital anomalies, IUD Significant contraction of the pelvis, Antepartum hemorrhage, Obstetric complications - Pre-eclampsia, multiple pregnancy Previous caesarean section scar Uterine malformation PROM
ECV Technique: It is best to avoid anesthesia. The patient’s abdomen is bared and the presentation and position of the fetus are carefully ascertained. Each hand then seizes each of the fetal poles. The cephalic pole is then gently manipulated toward the pelvic inlet while the other is moved in the opposite direction. By a series of gentle stroking and pushing movements the head is brought over the pelvic brim. To keep it in position, an abdominal pad and binder may be applied.
ECV During the manipulations - which should always be gentle, The fetal heart should be auscultated frequently. Any significant alterations in the fetal heart rate should be taken as a warning, and it would be wise not to proceed with the version. As far as possible the attitude of flexion in the fetus must be maintained. Follow up – These patients should be re-examined a few days later (1 week)when if needed, version may be tried again. External version can be attempted early in labour also, and chances of recurrence of the malpresentation are very much reduced.
ECV Causes of failure of version : Frank breech, Oligohydramnios Large baby, Obesity Short cord Complications : Abruption PPROM Preterm labor Entanglement of cord around fetal parts & formation of true knot Fetomaternal haemorrhage Amniotic fluid embolism
Management During Labor
Types of Delivery -
Vaginal delivery: - Spontaneous - Partial breech extraction - Total breech extraction Cesarean of delivery
Types Of Vaginal Breech Delivery • •
•
Spontaneous breech (rare) : No manipulation of the infant is necessary, other than ing the infant. Assisted breech delivery (Partial breech extraction) : lower half of Fetus (upto umbilicus) descends spontaneously at the vaginal introitus; then the fetus is extracted completely. Total breech extraction : The entire body is extracted. This is indicated only if there is evidence of fetal distress unresponsive to routine maneuvers and a cesarean delivery is not possible.
Conditions Unfavorable For Vaginal Delivery Fetus weight more than 3500 g Unfavorable pelvis – Breech delivery does not allow sufficient time for molding of the fetal head; thus a platypelloid or android pelvis decreases ability of fetal head to navigate maternal pelvis Hyperextension of the head – increases risk of cervical spine injury Footling - incidence of umbilical cord prolapse increases with coiling of the umbilical cord around the legs of the fetus
Indications For Cesarean Delivery Primi with breech Footling breech Any degree of contraction or unfavorable shape of pelvis
Hyperextended head When delivery is indicated in the absence spontaneous
labor A large fetus Healthy ,viable preterm fetus with mother in active labor Severe IUGR Lack of an experienced operator
Vaginal Delivery Prerequisites – Multipara patient with previous normal delivery Uncomplicated breech presentation Estimated fetal weight – 1.5 – 3.5 kg Pelvic adequacy Flexed head Experienced operator
Management Of Labor No place for induction of labor Rapid assessment of the patient
– Satisfactory progress in labor is the best indicator of pelvic adequacy – Close surveillance FHR and Uterine Contraction Assessment of fetal condition – USG to detect anomalies and extended head if vaginal delivery is planned – Monitoring FHS every 15 min, – When membranes rupture, per vaginum examination to check for cord prolapse,
Breech Vaginal Delivery The anterior buttock appears at the introitus A mediolateral episiotomy Further descent of the anterior buttock
Both buttocks come into view. The buttocks are expelled by
voluntary maternal effort. The fetal sacrum rotates anteriorly.
Breech Vaginal Delivery
Breech Vaginal Delivery The legs are delivered by flexion of the thighs and knees.
Assisted Delivery Of Frank Breech Moderate traction exerted by finger in each groin and
facilitated by generous episiotomy Pinard maneuver - Two fingers are inserted along one
extremity to the knee , then pushed away from midline after spontaneous flexion to deliver a foot into vagina
Assisted Delivery Of Frank Breech Both groin method
Pinard maneuver
Breech Vaginal Delivery No downward or outward traction is applied until the
umbilicus has been reached A towel wrapped around the fetal hips, gentle downward and outward traction in conjunction with maternal expulsive efforts until the scapula is reached Don’t elevate body and keep the body low.
Assisted Vaginal Breech Delivery After the scapula is reached,
the fetus should be rotated 90° in order to deliver the anterior arm. The anterior arm is followed to the elbow, and the arm is swept out of the vagina.
Assisted Vaginal Breech Delivery The fetus is rotated 180°,
and the contralateral arm is delivered. The infant is then rotated 90° to the backup position in preparation for delivery of the head.
Breech Vaginal Delivery • Delivery of the anterior shoulder - delivery of the posterior shoulder.
• Back is kept anterior. • The trunk is allowed to hang to encourage descent of the head.
Delivery Of The Aftercoming Head Modified Mauriceau – Smellie - Veit maneuver Burns-Marshall method Forceps
Prague maneuver
Modified Mauriceau – Smellie – Veit Maneuver Modified Mauriceau – Smellie – Veit maneuver – (Jaw
flexion shoulder traction ) – Baby placed on supinated left forearm with limbs on either side – Index and middle finger of one hand are applied over maxilla to flex the head (originally index finger was introduced in the mouth, not done to avoid dislocation of jaw). – Use the other hand to grasp the baby’s shoulders. – Downward traction until subocciput appears beneath the PS – Elevate body toward maternal abdomen. – Head flexion maintained by suprapubic pressure given by assistant.
Burns-Marshall Method Burns-Marshall method:
Fetus is left hanging. Its weight will exert traction -- when occiput appears under symphysis, fetus is grasped by feet and elevated upwards towards mother’s abdomen.
Forceps Forceps – Application of Piper forceps, employing towel
sling . The forceps are introduced from below, left blade first aiming directly for intended positions on sides of the head. Suspension of body in a towel effectively holds the fetus and help keep the arm out of the way Type: Piper’s forceps which have long shank, perineal curve
Long Shank
Perineal Curve
Piper Forceps Advantages:
1- Promotion of flexion 2- Traction is directly applied on head preventing overstretch of neck so protecting roots of brachial plexus 3- Prevention of sudden compression and decompression of head thus preventing ICH 4- Protection of head from injury by projecting ischial spines in cases of mild degrees of contracted pelvis
Difficulties Extended arm (nuchal arm) Entrapment Of Aftercoming Head
Lovset's Maneuver Extended Arm (nuchal arm) Prerequisites- inferior angle of scaula is visible underneath the pubic arch Anaesthesia – not required as intrauterine manipulation is nil. Principle: The maneuver is based on the fact that the posterior shoulder enters the pelvic cavity before the anterior because of the curved birth canal. If the fetal body is rotated with slight traction keeping back anterior through 180° posterior shoulder will appear below the pubic symphysis.
Lovset's Maneuver Technique - The fetal body is lifted slightly and ed
by the obstetrician's hands, and is rotated with slight traction through 180° (keeping back anterior), so that the posterior shoulder comes to lie in front. Since it is on a lower level than the anterior shoulder, it will deliver spontaneously or may be hooked out. The other shoulder may deliver spontaneously. If it is not delivered, the body of the child is now rotated through 180° in the opposite direction, so that the other arm is brought into the anterior position again, and the arm and shoulder are born spontaneously. The back then to be rotated to lie anteriorly.
Entrapment Of Aftercoming Head Prague maneuver – in occipitoposterior Dührssen incision - Incision at 10 o’clock , 2 o’clock and
may required at 6 o’clock Symphysiotomy - rarely use, serious maternal injury
Prague Maneuver Prague maneuver – Rarely, the back of the fetus is
posterior. Prague maneuver Consists of two fingers of one hand grasping the shoulders of the back-down fetus from below while the other hand draws the feet up over maternal abdomen.
Maternal Complications Increase risk of infection - caused by manual
manipulation within birth canal Maternal injuries - Rupture of uterus and cervical laceration - intrauterine maneuver, delivery of after coming head through an incompletely dilate cervix - Deep perineal tear - Extension of episiotomy
Perinatal Complications Fetal injuries from difficult delivery-
Intracranial haemorrhage – tentorium cerebelli tear Fracture humerus, clavicle & femur Hematoma of sternocleidomastoid muscle Dislocations – hip t, cervical vertebrae, mandible Brachial plexus injuries (paralysed arm) Visceral injuries LBW from preterm delivery, IUGR or both Cord prolapse Anomalies Operative intervention, especially cesarean delivery